Manipulating the HIF Pathway in Renal Transplantation, Current Progress and Future Developments
Received: 14-Sep-2017 / Accepted Date: 02-Nov-2016 / Published Date: 07-Nov-2016 DOI: 10.4172/2475-7640.1000110
Abstract
Renal transplantation is the gold standard treatment for end stage renal disease; however, there are currently not enough suitable organs to meet a growing demand. The Hypoxia Inducible Factor (HIF) pathway comprises a number of oxygen sensitive transcription factors which activate cellular protective functions. Allografts from cadaveric organs make up a large proportion of the organ pool. These organs are subjected to hypoxic and ischemic conditions during the harvesting and transplant process. Manipulation of the HIF pathway may reduce organ damage and improve outcomes. This review evaluates the current evidence for the use of the HIF pathway in renal transplantation and also adds new research conducted into the effect on organ metabolism.
Keywords: Transplantation; HIF; Renal; Metabolism
15154Introduction
The success of renal transplantation and ever pressing demand for donor organs has resulted in the utilisation of organs previously deemed to be non-transplantable including those termed ‘marginal’ and Extended Criteria Donor (ECD) kidneys [1-3]. These organs have worse associated clinical outcomes compared with living donor or standard criteria donor kidneys [1,2,4]. Given the global decline in cadaveric organ quality, the need to optimise their function is self-evident in order to strive for optimal patient outcomes.
Hypothermic Machine Perfusion (HMP) is a common method of organ preservation which involves the recirculation of cooled perfusion fluid through the renal vasculature. The clinical benefits of HMP are now well documented with reduction in Delayed Graft Function (DGF) and improved graft survival at 1 and 3 years [5,6]. In addition to these benefits, HMP provides a window during which novel therapies can be introduced into the perfusion fluid and delivered to cells within the renal parenchyma.
Organ ischemia results from cessation of blood flow following organ retrieval from both live and cadaveric donors. The resultant shift towards anaerobic metabolism is reflected in rising lactate levels as an end product of anaerobic respiration [7-9]. Hypothermia reduces cellular metabolism and oxygen requirement, along with a reduction in the rate of substrate and energy depletion. There is a 1.5-2 fold reduction in metabolism for every 10°C drop in temperature with activity present even at 1°C. A consequence of anaerobic metabolism and the inefficient generation of ATP per glucose molecule is a rapid depletion of intracellular energy stores [10]. The lack of intracellular ATP leads to the failure of the ATP dependent sodium-potassium membrane pump, resulting in cellular influx of sodium and efflux of potassium with a loss of cellular integrity and ultimately, cell death. Thus rapid organ cooling following organ retrieval is essential in order to reduce short and long-term detrimental effects of prolonged anaerobic metabolism.
1D 1H Nuclear Magnetic Resonance (NMR) analysis of metabolites present in HMP perfusate has shown that metabolism occurs while under HMP conditions [7,11,12]. Moreover, the metobolomic profile of perfusion fluid appears to differ between kidneys with immediate and delayed graft function. Modification of metabolic processes such as the upregulation of the HIF pathway may improve outcomes for HMP kidneys.
The Hypoxia Inducible Factor (HIF) pathway is activated as part of the cellular response to hypoxia and exerts its beneficial effects via multiple mechanisms. Upregulation of the HIF pathway has been shown in an animal model to reduce Ischaemia Reperfusion Injury (IRI) [13-15] which is known to be deleterious during renal transplantation and is associated with an increased risk of DGF and reduced graft survival [15-17]. Furthermore, in hypoxic conditions, activation of the HIF pathway is associated with upregulation of mechanisms that facilitate glycolysis such as facultative glucose transporter-1, aldolase A, phosphoglycerate kinase 1 and pyruvate kinase M [18].
The increased delivery of glucose to the intracellular environment and subsequent glycolysis to produce ATP [19,20] would be seemingly beneficial during HMP given the glucose rich environment of commonly used perfusion fluids (Kidney Perfusion Solution 1/ University of Wisconsin Machine Perfusion Solution) in the absence of oxygen carriers or exogenous oxygen.
Aim
Given these two potentially protective mechanisms of HIF activation during organ preservation, namely amelioration of the IRI phenomenon and promotion of glycolytic activity, we aim to review and add to existing research on the role of the HIF pathway activation in renal transplantation and explore its manipulation in order to improve clinical outcomes following renal transplantation.
The HIF pathway and metabolic actions
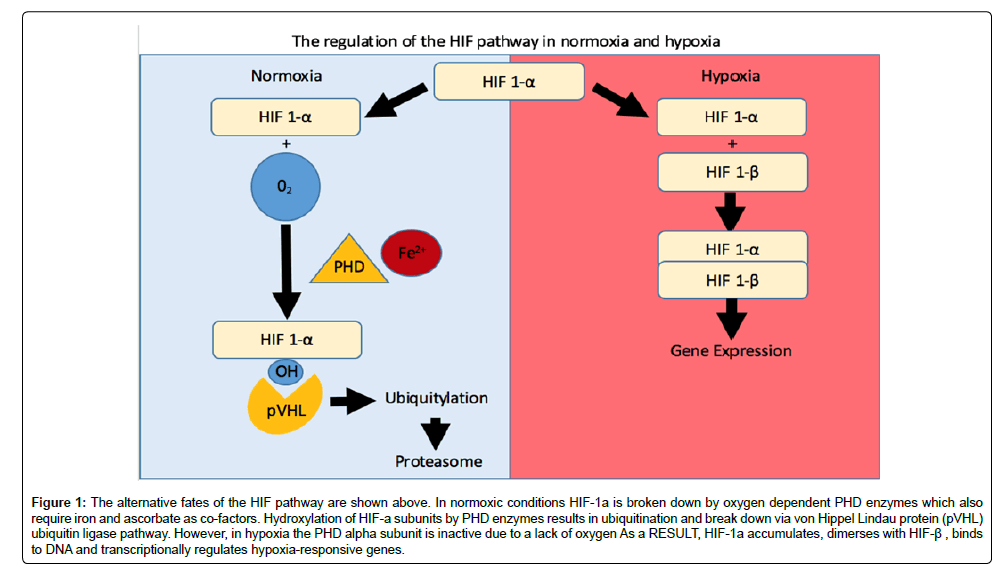
The HIF pathway, described as the ‘master regulator of the cellular hypoxic response, [21,22] has been shown to play key regulatory mechanisms in multiple disease states including acute ischemic renal failure and renal fibrosis [23,24]. HIF is a hetero-dimeric transcription factor composed of an oxygen dependent α subunit (1α,2α,3α) and an oxygen independent β sub-unit [24,25]. In normoxic environments HIF is rendered transcriptionally inactive. The α sub-unit is degraded by Propyl-Hydroxylase Enzymes (PHD-1, PHD-2, PHD-3), which require iron as a co-factor prior to subsequent ubiquitination and break down via von Hippel Lindau protein (pVHL) ubiquitin ligase pathway [24-31]. PHD inhibition up-regulates the HIF pathway by preventing this homeostatic mechanism. The von Hippel Lindau protein plays a key role in the degradation of the HIF pathway under normoxic conditions and the prevention of its over-expression (Figure 1) [31,32].
Figure 1: The alternative fates of the HIF pathway are shown above. In normoxic conditions HIF-1a is broken down by oxygen dependent PHD enzymes which also require iron and ascorbate as co-factors. Hydroxylation of HIF-a subunits by PHD enzymes results in ubiquitination and break down via von Hippel Lindau protein (pVHL) ubiquitin ligase pathway. However, in hypoxia the PHD alpha subunit is inactive due to a lack of oxygen As a RESULT, HIF-1a accumulates, dimerses with HIF-β , binds to DNA and transcriptionally regulates hypoxia-responsive genes.
Experimental studies have highlighted distinct roles for the HIF sub-units in the hypoxic cellular response with HIF-1α activation demonstrating clear metabolic effects with the a shift in cellular metabolism from aerobic to anaerobic [25,32-34]. HIF-1α activation facilitates ATP production as a result of an increase in anaerobic glycolytic activity via the upregulation of both glycolytic pathway enzymes and glucose transporters (Glut-1) [34-36]. Further metabolic sequelae of HIF-1α activation is the inhibition of the TCA cycle via upregulation of pyruvate dehydrogenase kinase 1, which reduces the amount of the TCA substrate Acetyl-CoA [37].
Further beneficial effects of HIF-1α pathway activation are the improved respiratory efficiency in hypoxic cells [33,38,39]. This mechanism occurs via the regulation of cytochrome c oxidase (complex IV) as it catalyses the final step of the electron transport chain, the reduction of oxygen to water, thus increasing mitochondrial ATP generation [38-40]. In contrast, stimulation of HIF-2α has wide ranging effects including pro survival gene upregulation such as VEGF, TGF-a and EPO [41].
Manipulation of the HIF pathway
Mechanical and pharmacological upregulation of the HIF pathway has been described in animal transplant models. Mechanical upregulation of the pathway has been induced in a rat mode by bilateral clamping of the renal pedicle for 45 min [13]. This induces total ischaemia for the designated period, however, preconditioning leading to a hypoxic/ischaemic tolerance can achieved by sequential clamping and unclamping of the renal pedicle although the clinical application pre-retrieval of organs is understandably limited [42].
Pharmacological methods for inducing the HIF pathway include specific PHD inhibitors FG-4497 [43] or non-specific inhibitors such as desferrioxamine [44], xenon [45], fenoldopam [46] and dimethyloxalylglycine (DMOG) [47]. Interestingly, lactobionate which is a constituent of the University of Wisconsin (UW) preservation solution, is an iron chelator and therefore inhibits HIF via a mechanism similar to desferrioxamine, [48] as PHD enzymes depend on iron as a cofactor [15,49,50].
HIF in human observational studies
HIF-1α activation is one mechanism by which cells are protected from the effects of hypoxia, [34,51] thus, attempts to characterise and manipulate this pathway have been explored in both human [13] and animal studies [43,52].
Post-transplant HIF-1α levels have been shown to be upregulated in functioning grafts (CIT>15 h), and at considerably lower levels in non-functioning kidneys. The authors describe the trend that kidneys with increased post-transplant HIF-1α expression had lower rates of rejection, although this relationship was not statistically significant [53].
HIF-1α accumulates as a result of both renal ischaemia and also reperfusion in human proximal tubule cells, even after prolonged ischaemia, illustrating how both ‘hits’ are important [14]. Analysis of the biopsies of transplanted kidneys in the same study demonstrated HIF-1α was absent in kidney biopsies with marked ischemic damage and higher in proximal tubule cells with a lesser severity of ATN post-transplantation; expression was even higher in those cells with non-damaged tubule cells illustrating how HIF-1α stabilized during reperfusion may be required for proximal tubule survival and repair [13]. Accounting for this is the observation that proximal tubule cells have the potential to fully recover from ischemic pathology [54].
Rather than relying on a separate progenitor lineage, each individual Renal Proximal Tubule Epithelial Cell (RPTEC) has the potential to mediate tubule repair through an interplay between proliferation and efferocytosis of damaged cells [55]. In vitro studies have demonstrated that post ischemic insult, RPTEC de-differentiate and proliferate [56], undergoing a glycolytic switch to fuel expansion [57], rather than utilising fatty acids, the preferred metabolic entry point preferred by the mature PT epithelium [58]. This glycolytic switch coincides with increased HIF1 activity [57], which as described before upregulates genes necessary for glycolysis, suggesting a key role for HIF-1α in tubule repair.
The absence of HIF-1α from severely damaged tubules is also interesting, and suggests limited proliferation of the PTEC and therefore a finite reparative capability of the proximal tubule. Post-transplant proximal tubule function, in the absence of any other detectable underlying pathologies is linked with patient outcomes [59].
Parallel to this, HIF-1α has previously been thought to have a role in the late rejection of renal transplants by facilitating the process of renal fibrosis. The expression of HIF-1α was shown to be higher amongst infiltrating inflammatory cells in areas of tubular atrophy/ interstitial fibrosis in biopsies of chronic graft dysfunction, suggesting that the HIF pathway activation is associated with renal fibrosis [60].
Inactivation of the HIF-1α response via the use of HIF-1α small interfering RNA (siRNA), provoked significant cell death in a human proximal epithelial cell line further exposing the role HIF-1α plays in mediating proximal tubular cell survival in response to ischemia reperfusion injury both in vitro and in vivo [13].
The correlation between HIF-1α expression in graft biopsies and histological/clinical outcome is widely debated yet patterns have emerged. HIF-1α expression was shown to be higher in primarily functioning kidneys compared to those with primary non-function. Protocol biopsies at 2 weeks showed widespread HIF-1α expression with biopsies beyond 3 month void of HIF-1α other than in clinical/ sub-clinical rejection [53] thus implicating hypoxia in the process of chronic rejection. The presence of HIF-1α was absent in kidney biopsies with marked ischemic damage and only present in those with less severe injury leading to the hypothesis that the HIF pathway was responsible for protective mechanisms. Manipulation of the HIF pathway in vivo and ex vivo transplant models has been explored, however, no clinical trials have attempted to stimulate the HIF pathway in donors, recipients or during preservation of solid organ transplants [61].
Opportunities for the HIF pathway manipulation during the transplantation process
Manipulating the HIF pathway response in animal models: A transplant model using porcine kidneys demonstrated the increased expression of HIF-1α following transplantation and its potential positive role in tubular repair [62]. Interrogation of the HIF pathway response has been reported in several murine kidney models [13,45,52,60,63-66]. In a murine model those treated with Xenon or FG-4497 (Non-specific and specific HIF pathway inducers, respectively) prior to nephrectomy led to significantly improved results following transplant. The recipients of kidney transplants from those pre-treated animals demonstrated improved function (reduced DGF) following transplantation, which correlated with degree of HIF-1α up regulation [43,67]. Similar findings were demonstrated in a renal ischaemia model and the benefits of the HIF induction effects were abrogated with the introduction of HIF-1α siRNA [13,45]. The beneficial effects of pharmacological HIF-1 pathway stimulation appear to be long lasting with genetic (upregulation of EPO and HO-1) and functional effects of donor treatment persisting in the recipient post-transplant, even when these organs were subjected to significant period of cold ischaemia [65]. These results imply that in animal models, donor pre-treatment with a HIF pathway inducer has beneficial transplant outcomes and that activation of HIF is maintained under organ preservation conditions. Similar results have been reproduced when PHD inhibitors have been given to recipient mice following transplant with improved function demonstrated several weeks later [63].
HIF pathway modification during HMP
Findings from animal studies indicate that the HIF pathway activation is not exhausted even after total mechanical ischaemia (such as during DCD retrieval conditions) [13]. Given that there are potential benefits to further HIF stimulation following organ retrieval and HMP can deliver pharmaceutical agents to the cells within an organ, it is perhaps surprising that there are no previous reports detailing the role of pharmacological HIF pathways stimulators during HMP.
Having previously used metobolomic analysis to show the porcine kidney behaves similarly to human kidneys [7] and that isotopic glucose 13C 2D-NMR tracer experiments can be used to determine new metabolism during HMP [8] we aimed to investigate the metabolic effects of pharmacological the HIF pathway activation while under HMP. We hypothesised that even after being subject to extreme ischaemic conditions in this DCD model, the HIF pathway could be further stimulated to alter the metabolism during HMP to facilitate greater anaerobic glycolytic activity.
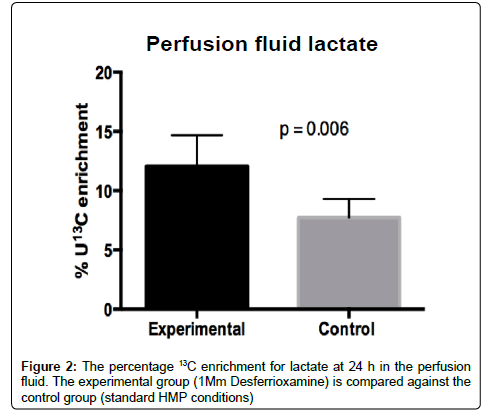
Kidneys (n=6) were perfused for 24 h under HMP conditions following organ retrieval (Warm ischemia time: WIT 14 min). One kidney from each pair was perfused with fluid containing the nonspecific PHD inhibitor (and therefore HIF inducer) desferrioxamine (1 mM) with the contralateral kidneys undergoing standard HMP serving as the control group. The perfusion fluid was similar to KPS-1 perfusion fluid with the substitution of glucose with the uniformly labelled non-radioactive isotope (U13C glucose) to allow metabolic tracer analysis.
The presence of fully labelled lactate (i.e., 13C in each carbon position) in the perfusion fluid demonstrates de novo glycolytic activity within the kidney with subsequent export from the perfused organ. The proportion of labelled lactate in the fluid after 24 h was found to be significantly higher in the presence of the PHD inhibitor (desferrioxamine) indicating upregulation of glycolysis (Mean 12.0% vs. 7.7% p=0.006) (Figure 2). Similarly, the proportion of labelled lactate was greater in the kidney tissue for the desferrioxamine treated group (14.0% vs. 9.3% p=0.008). Whilst the metabolic differences between the two groups may be due to the direct metabolic influence of the iron chelator desferrioxamine on the kidney, there was no difference in proportion of labelled lactate in the system after 6 h indicating that the impact on the metabolism of desferrioxamine is more protracted. Metabolic influence resulting from HIF activity would occur at a gene transcriptional level and therefore the delay in metabolic impact of desferrioxamine in this kidney perfusion model would support HIF as the likely aetiology.
Although, the HIF pathway activation has been previously suggested as a being potentially beneficial in transplantation [61], to our knowledge this is the first report whereby the metabolic effects of HIF stimulation has been investigated during the HMP period. Although the functional consequences of HIF stimulation are not investigated in this study, we have shown in this animal model that the metabolic phenotype during HMP can be altered by the introduction of the iron chelator and non-specific pharmacological HIF pathway stimulator desferrioxamine. This finding corroborates previous studies, suggesting that in this DCD model, the HIF pathway is not exhausted despite periods of prolonged ischaemia [13]. Furthermore, the increase in the glycolytic endpoint U13C lactate in the desferrioxamine treated group demonstrates that metabolic upregulation of glycolytic activity is achievable in these ex vivo hypothermic hypoxic conditions which could potentially be used to optimise organ metabolism in the pre-transplant period.
Harmful effects of HIF pathway manipulation
Despite the potential benefits, there are also concerns regarding the possible harmful effects of manipulation of the HIF pathway in humans. There is some evidence in cancer studies that overexpression of the HIF pathway may have a role in hypoxia induced apoptosis [68]. VHL is a key component in the normoxic regulation and degradation of the HIF pathway, subsequently VHL mutation, specifically inactivation, plays a key role in clear cell renal carcinoma due to a loss of this feedback pathway [69]. This failure to break down HIF-1α has been shown to lead to overexpression of the HIF pathway which can predispose the cell to an invasive, highly vascular and cytotoxic resistant phenotype [70]. A link has also been demonstrated between high levels of the HIF pathway activation and renal fibrosis [71,72]. Although in other studies, correlating Banff scores from post-transplant histological samples with HIF-1α expression has not shown any significant relationship [73].
In addition, there are some concerns that HIF pathway stimulation can lead to immune mediated complications such as BK virus. HIF-1α has been known to interact with viruses with an increased HIF-1α expression reported in transplant biopsies from patients with active polyoma (BK) virus [74], a major cause of morbidity post transplantation [75].
Discussion
The HIF pathway plays a key role in the protective cellular response to ischaemia and hypoxia [13,47,70]. This has further been shown in transplantation models to have the potential to improve outcomes when active in donors prior to transplantation [43,45,46].
The murine studies discussed highlight the potential benefit of donor preconditioning via HIF pathway stimulation prior to organ retrieval [13,14,43]. However, these potential benefits remain at the experimental phase and have not been validated in the human setting. HIF pathway stimulation would be seemingly most advantageous for Deceased Cardiac Death (DCD) donors, who have an inevitable period of warm ischaemia. There are ethical concerns regarding the administration of ‘organ-priming’ drugs prior to organ retrieval [76] from which these donors who are alive at the time of drug administration would receive no direct benefit. Over activity of the HIF pathway is associated with several potential harmful effects [68,72,77] thus its modification should be approached with caution.
HMP provides a novel opportunity to pre-condition organs prior to transplantation. To our knowledge this is the first report to suggest that pharmacological stimulation of the HIF pathway during HMP can alter metabolism during the hypothermic hypoxic conditions of organ preservation. The metabolic shift to a more glycolytic metabolic state could perhaps be a demonstration of improved respiratory efficacy induced by HIF pathway upregulation. However, further research should increase the sample size and correlate changes in the metabolomics profile with clinical outcomes in order to explore the potential for pre-conditioning in the HMP setting.
Acknowledgements and Funding
This work was funded by grants from the Arthur Thompson charitable trust (Birmingham Medical School) and the Kidney Research UK Intercalated award.
Funding was also provided by the University Hospitals Birmingham charities.
Organ recovery systems provided the Lifeport TM machines.
References
- Rao PS, Ojo A (2009) The alphabet soup of kidney transplantation: SCD, DCD, ECD--fundamentals for the practicing nephrologist. Clin J Am Soc Nephrol 4: 1827-1831.
- Jochmans I, O'Callaghan JM, Pirenne J, et al. (2015) Hypothermic machine perfusion of kidneys retrieved from standard and high-risk donors. Transpl Int 28: 665-676.
- Guibert EE, Petrenko AY, Balaban CL, Somov AY, Rodriguez JV, et al. (2011) Organ Preservation: Current Concepts and New Strategies for the Next Decade. Transfus Med Hemother 38: 125-142.
- NHS Kidney Care. Kidney Disease: Key facts and figures [Internet]. NHS; 2010 Sep.
- Moers C, Smits JM, Maathuis MH, Treckmann J, van Gelder F, et al. (2009) Machine perfusion or cold storage in deceased-donor kidney transplantation. N Engl J Med 360: 7-19.
- O'Callaghan JM, Morgan RD, Knight SR, Morris PJ (2013) Systematic review and meta-analysis of hypothermic machine perfusion versus static cold storage of kidney allografts on transplant outcomes. Br J Surg 100: 991-1001.
- Nath J, Guy A, Smith TB, Cobbold M, Inston NG, Hodson J, et al. Metabolomic perfusate analysis during kidney machine perfusion: the pig provides an appropriate model for human studies. PLoS ONE 12: e114818.
- Nath J, Smith T, Hollis A, Ebbs S, Canbilen SW, Tennant DA, et al. (2016) 13C glucose labelling studies using 2D NMR are a useful tool for determining ex vivo whole organ metabolism during hypothermic machine perfusion of kidneys. Transplant Res 5.
- Guy AJ, Nath J, Cobbold M, Ludwig C, Tennant DA, et al. (2015) Metabolomic analysis of perfusate during hypothermic machine perfusion of human cadaveric kidneys. Transplantation 99: 754-759.
- Vander Heiden MG, Cantley LC, Thompson CB (2009) Understanding the Warburg effect: the metabolic requirements of cell proliferation. Science 324: 1029-1033.
- Guy AJ, Nath J, Cobbold M, Ludwig C, Tennant DA, et al. (2015) Metabolomic analysis of perfusate during hypothermic machine perfusion of human cadaveric kidneys. Transplantation 99: 754-759.
- Bon D, Billault C, Claire B, Thuillier R, Hebrard W, Boildieu N, et al. (2014) Analysis of perfusates during hypothermic machine perfusion by NMR spectroscopy: a potential tool for predicting kidney graft outcome. Transplantation 8: 810-816.
- Conde E, Alegre L, Blanco-Sánchez I, Sáenz-Morales D, Aguado-Fraile E, Ponte B, et al. (2012) Hypoxia Inducible Factor 1-Alpha (HIF-1 Alpha) Is Induced during Reperfusion after Renal Ischemia and Is Critical for Proximal Tubule Cell Survival. PLoS ONE 3: e33258.
- Bernhardt WM, Warnecke C, Willam C, Tanaka T, Wiesener MS, Eckardt K. (2007) Organ Protection by Hypoxia and Hypoxia-Inducible Factors. In: Enzymology B-M 435: 219-245.
- Shen X, Wan C, Ramaswamy G, Mavalli M, Wang Y, Duvall CL, et al. (2009) Prolyl hydroxylase inhibitors increase neoangiogenesis and callus formation following femur fracture in mice. J Orthop Res Off Publ Orthop Res Soc 10: 1298-1305.
- Schröppel B, Legendre C (2014) Delayed kidney graft function: from mechanism to translation. Kidney Int 86: 251-258.
- An Y, Zhang J, Han J, Yang H, Tie L, Yang X, et al. (2013) Hypoxia-inducible factor-1a dependent pathways mediate the renoprotective role of acetazolamide against renal ischemia-reperfusion injury. Cell Physiol Biochem Int J Exp Cell Physiol Biochem Pharmacol 5: 1151-1166.
- Alfarouk KO, Verduzco D, Rauch C, Muddathir AK, Adil HHB, Elhassan GO, et al. (2014) Glycolysis, tumor metabolism, cancer growth and dissemination. A new pH-based etiopathogenic perspective and therapeutic approach to an old cancer question. Oncoscience 12: 777-802.
- Morten KJ, Badder L, Knowles HJ (2013) Differential regulation of HIF-mediated pathways increases mitochondrial metabolism and ATP production in hypoxic osteoclasts. J Pathol 229: 755-764.
- Ebert BL, Firth JD, Ratcliffe PJ. (1995) Hypoxia and Mitochondrial Inhibitors Regulate Expression of Glucose Transporter-1 via Distinct Cis-acting Sequences. J Biol Chem 49: 29083-29089.
- Semenza GL (2004) Hydroxylation of HIF-1: oxygen sensing at the molecular level. Physiology (Bethesda) 19: 176-182.
- Howell NJ, Tennant DA (2014) The role of HIFs in ischemia-reperfusion injury. Hypoxia (Auckl) 2: 107-115.
- Haase VH (2006) The VHL/HIF oxygen-sensing pathway and its relevance to kidney disease. Kidney Int 69: 1302-1307.
- Jiang BH, Rue E, Wang GL, Roe R, Semenza GL (1996) Dimerization, DNA binding, and transactivation properties of hypoxia-inducible factor 1. J Biol Chem 271: 17771-17778.
- Adams JM, Difazio LT, Rolandelli RH, Luján JJ, Haskó G, et al. (2009) HIF-1: a key mediator in hypoxia. Acta Physiol Hung 96: 19-28.
- Carmeliet P1, Dor Y, Herbert JM, Fukumura D, Brusselmans K, et al. (1998) Role of HIF-1alpha in hypoxia-mediated apoptosis, cell proliferation and tumour angiogenesis. Nature 394: 485-490.
- Koh MY1, Spivak-Kroizman TR, Powis G (2010) HIF-1alpha and cancer therapy. Recent Results Cancer Res 180: 15-34.
- Schofield CJ, Ratcliffe PJ (2004) Oxygen sensing by HIF hydroxylases. Nat Rev Mol Cell Biol 5: 343-354.
- Berra E, Benizri E, Ginouvès A, Volmat V, Roux D, et al. (2003) HIF prolyl-hydroxylase 2 is the key oxygen sensor setting low steady-state levels of HIF-1alpha in normoxia. EMBO J 22: 4082-4090.
- Ivan M, Kondo K, Yang H, Kim W, Valiando J, Ohh M, et al. (2001) HIF alpha targeted for VHL-mediated destruction by proline hydroxylation: implications for O2 sensing. Science 5516: 464-468.
- Masson N, Willam C, Maxwell PH, Pugh CW, Ratcliffe PJ. (2001) Independent function of two destruction domains in hypoxia-inducible factor-alpha chains activated by prolyl hydroxylation. EMBO J 18: 5197-5206.
- Maxwell P (2003) HIF-1: an oxygen response system with special relevance to the kidney. J Am Soc Nephrol 14: 2712-2722.
- Papandreou I, Cairns RA, Fontana L, Lim AL, Denko NC. (2006) HIF-1 mediates adaptation to hypoxia by actively down regulating mitochondrial oxygen consumption. Cell Metab 3: 187-197.
- Loboda A, Jozkowicz A, Dulak J (2010) HIF-1 and HIF-2 transcription factors--similar but not identical. Mol Cells 29: 435-442.
- Harkness, R.A. (1999) Metabolism at a Glance, 2nd Edition. J.G. Salway. J Inherit Metab Dis 8: 914.
- Solaini G, Baracca A, Lenaz G, Sgarbi G (2010) Hypoxia and mitochondrial oxidative metabolism. Biochim Biophys Acta 1797: 1171-1177.
- Ziello JE, Jovin IS, Huang Y (2007) Hypoxia-Inducible Factor (HIF)-1 regulatory pathway and its potential for therapeutic intervention in malignancy and ischemia. Yale J Biol Med 80: 51-60.
- Kumar H, Choi D-K, Kumar H, Choi D-K. (2015) Hypoxia Inducible Factor Pathway and Physiological Adaptation: A Cell Survival Pathway?, Hypoxia Inducible Factor Pathway and Physiological Adaptation: A Cell Survival Pathway? Mediat Inflamm Mediat Inflamm 2015: e584758.
- Tsukihara T, Aoyama H, Yamashita E, Tomizaki T, Yamaguchi H, et al. (1996) The whole structure of the 13-subunit oxidized cytochrome c oxidase at 2.8 A. Science 272: 1136-1144.
- Semenza GL (2007) Oxygen-dependent regulation of mitochondrial respiration by hypoxia-inducible factor 1. Biochem J 405: 1-9.
- Ratcliffe PJ (2007) HIF-1 and HIF-2: working alone or together in hypoxia? J Clin Invest 117: 862-865.
- Yang C-C, Lin L-C, Wu M-S, Chien C-T, Lai M-K. (2009) Repetitive hypoxic preconditioning attenuates renal ischemia/reperfusion induced oxidative injury via upregulating HIF-1 alpha-dependent bcl-2 signaling. Transplantation 11: 1251-1260.
- Bernhardt WM, Gottmann U, Doyon F, Buchholz B, Campean V, Schödel J, et al. Donor treatment with a PHD-inhibitor activating HIFs prevents graft injury and prolongs survival in an allogenic kidney transplant model. Proc Natl Acad Sci 50: 21276-21281.
- ernhardt WM, Gottmann U, Doyon F, Buchholz B, Campean V, Schödel J, et al. Donor treatment with a PHD-inhibitor activating HIFs prevents graft injury and prolongs survival in an allogenic kidney transplant model. Proc Natl Acad Sci 50: 21276-21281.
- Woo KJ, Lee TJ, Park JW, Kwon TK (2006) Desferrioxamine, an iron chelator, enhances HIF-1alpha accumulation via cyclooxygenase-2 signaling pathway. Biochem Biophys Res Commun 343: 8-14.
- Ma D, Lim T, Xu J, Tang H, Wan Y, Zhao H, et al. (2009) Xenon Preconditioning Protects against Renal Ischemic-Reperfusion Injury via HIF-1a Activation. J Am Soc Nephrol 4: 713-720.
- Yi X, Zhang G, Yuan J (2013) Renoprotective role of fenoldopam pretreatment through hypoxia-inducible factor-1alpha and heme oxygenase-1 expressions in rat kidney transplantation. Transplant Proc 45: 517-522.
- Song YR, You SJ, Lee YM, Chin HJ, Chae DW, et al. (2010) Activation of hypoxia-inducible factor attenuates renal injury in rat remnant kidney. Nephrol Dial Transplant 25: 77-85.
- Isaacson Y, Salem O, Shepherd RE, Van Thiel DH (1989) Lactobionic acid as an iron chelator: a rationale for its effectiveness as an organ preservant. Life Sci 45: 2373-2380.
- Fan L, Li J, Yu Z, Dang X, Wang K, Fan L, et al. (2014) The Hypoxia-Inducible Factor Pathway, Prolyl Hydroxylase Domain Protein Inhibitors, and Their Roles in Bone Repair and Regeneration, The Hypoxia-Inducible Factor Pathway, Prolyl Hydroxylase Domain Protein Inhibitors, and Their Roles in Bone Repair and Regeneration. BioMed Res Int BioMed Res Int 2014: e239356.
- Karuppagounder SS, Ratan RR (2012) Hypoxia-inducible factor prolyl hydroxylase inhibition: robust new target or another big bust for stroke therapeutics? J Cereb Blood Flow Metab 32: 1347-1361.
- Hu CJ, Wang LY, Chodosh LA, Keith B, Simon MC (2003) Differential roles of hypoxia-inducible factor 1alpha (HIF-1alpha) and HIF-2alpha in hypoxic gene regulation. Mol Cell Biol 23: 9361-9374.
- Bernhardt WM, Câmpean V, Kany S, Jürgensen J-S, Weidemann A, Warnecke C, et al. Preconditional Activation of Hypoxia-Inducible Factors Ameliorates Ischemic Acute Renal Failure. J Am Soc Nephrol 7: 1970-1978.
- Rosenberger C, Pratschke J, Rudolph B, Heyman SN, Schindler R, Babel N, et al. (2007) Immunohistochemical detection of hypoxia-inducible factor-1alpha in human renal allograft biopsies. J Am Soc Nephrol JASN 1: 343-351.
- Gall JM. Hexokinase and mitofusin 2: Mitochondrial modulators of apoptosis in ischemic acute kidney injury [Internet]. BOSTON UNIVERSITY; 2012
- Devarajan P (2006) Update on mechanisms of ischemic acute kidney injury. J Am Soc Nephrol 17: 1503-1520.
- Humphreys BD, Valerius MT, Kobayashi A, Mugford JW, Soeung S, et al. (2008) Intrinsic epithelial cells repair the kidney after injury. Cell Stem Cell 2: 284-291.
- Aschauer L, Gruber LN, Pfaller W, Limonciel A, Athersuch TJ, et al. (2013) Delineation of the key aspects in the regulation of epithelial monolayer formation. Mol Cell Biol 33: 2535-2550.
- Mandel LJ. (1985) Metabolic Substrates, Cellular Energy Production, and the Regulation of Proximal Tubular Transport. Annu Rev Physiol 1: 85-101.
- Câmara NO, Williams WW Jr, Pacheco-Silva A (2009) Proximal tubular dysfunction as an indicator of chronic graft dysfunction. Braz J Med Biol Res 42: 229-236.
- Yu TM, Wen MC, Li CY, Cheng CH, Wu MJ, et al. (2013) Expression of hypoxia-inducible factor-1a (HIF-1a) in infiltrating inflammatory cells is associated with chronic allograft dysfunction and predicts long-term graft survival. Nephrol Dial Transplant 28: 659-670.
- Akhtar MZ, Sutherland AI, Huang H, Ploeg RJ, Pugh CW. (2014) The role of hypoxia-inducible factors in organ donation and transplantation: the current perspective and future opportunities. Am J Transplant 7: 1481-1487.
- Lario S, Mendes D, Bescós M, Iñigo P, Campos B, Alvarez R, et al. (2003) Expression of transforming growth factor-beta1 and hypoxia-inducible factor-1alpha in an experimental model of kidney transplantation. Transplantation 10: 1647-1654.
- Franceschini N, Cheng O, Zhang X, Ruiz P, Mannon RB. (2003) Inhibition of prolyl-4-hydroxylase ameliorates chronic rejection of mouse kidney allografts. Am J Transplant 4: 396-402.
- Rosenberger C, Mandriota S, Jürgensen JS, Wiesener MS, Hörstrup JH, et al. (2002) Expression of hypoxia-inducible factor-1alpha and -2alpha in hypoxic and ischemic rat kidneys. J Am Soc Nephrol 13: 1721-1732.
- Bernhardt WM, Gottmann U, Doyon F, Buchholz B, Campean V, Schödel J, et al. (2009) Donor treatment with a PHD-inhibitor activating HIFs prevents graft injury and prolongs survival in an allogenic kidney transplant model. Proc Natl Acad Sci 50: 21276-21281.
- Zhang XL, Yan ZW, Sheng WW, Xiao J, Zhang ZX, et al. (2011) Activation of hypoxia-inducible factor-1 ameliorates postischemic renal injury via inducible nitric oxide synthase. Mol Cell Biochem 358: 287-295.
- Zhao H, Watts HR, Chong M, Huang H, Tralau-Stewart C, Maxwell PH, et al. Xenon Treatment Protects Against Cold Ischemia Associated Delayed Graft Function and Prolongs Graft Survival in Rats. Am J Transplant 8: 2006-2018.
- Greijer AE, van der Wall E (2004) The role of hypoxia inducible factor 1 (HIF-1) in hypoxia induced apoptosis. J Clin Pathol 57: 1009-1014.
- Cowey CL, Rathmell WK (2009) VHL gene mutations in renal cell carcinoma: role as a biomarker of disease outcome and drug efficacy. Curr Oncol Rep 11: 94-101.
- Tung-Wei H, Jia-Hung L, Kun-Tu Y, Jen-Pi T, Sheng-Wen W, Hui-Chun T, et al. (2013) Renal expression of hypoxia inducible factor-1a in patients with chronic kidney disease: a clinicopathologic study from nephrectomized kidneys. Indian J Med Res 1: 102-110.
- Haase VH (2012) Hypoxia-inducible factor signaling in the development of kidney fibrosis. Fibrogenesis Tissue Repair 5: S16.
- Semenza GL (2002) HIF-1 and tumor progression: pathophysiology and therapeutics. Trends Mol Med 8: S62-67.
- Kellenberger T, Marcussen N, Nyengaard JR, Wogensen L, Jespersen B. Expression of hypoxia-inducible factor-1a and hepatocyte growth factor in development of fibrosis in the transplanted kidney. Transpl Int 2: 180-190.
- Signorini L, Croci M, Boldorini R, Varella RB, Elia F, et al. (2016) Interaction Between Human Polyomavirus BK and Hypoxia Inducible Factor-1 alpha. J Cell Physiol 231: 1343-1349.
- Weikert BC, Blumberg EA (2008) Viral infection after renal transplantation: surveillance and management. Clin J Am Soc Nephrol 3 Suppl 2: S76-86.
- Moch H (2008) [Von-Hippel-Lindau (VHL) protein function by initiation and progression of renal cancer]. Pathologe 29 Suppl 2: 149-152.
Citation: Hollis A, Patel K, Smith T, Nath J, Tennant D, et al. (2016) Manipulating the HIF Pathway in Renal Transplantation, Current Progress and Future Developments. J Clin Exp Transplant 1: 110. DOI: 10.4172/2475-7640.1000110
Copyright: © 2016 Hollis A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 12587
- [From(publication date): 12-2016 - Nov 21, 2024]
- Breakdown by view type
- HTML page views: 11899
- PDF downloads: 688