Man-in-A-Barrel: Amytrophic Lateral Sclerosis Misdiagnosed as Rotator Cuff Injury in a Military Veteran
Received: 23-May-2023 / Manuscript No. JADP-23-99646 / Editor assigned: 25-May-2023 / PreQC No. JADP-23-99646 (PQ) / Reviewed: 08-Jun-2023 / QC No. JADP-23-99646 / Revised: 23-Jun-2023 / Manuscript No. JADP-23-99646 (R) / Published Date: 03-Jul-2023 DOI: 10.4172/2161-0460.1000573
Abstract
Amytrophic Lateral Sclerosis (ALS) is a neurodegenerative disorder defined by its effects on both Upper Motor Neurons (UMN) and Lower Motor Neurons (LMN). ALS typically spares other neurologic functions (sensory, autonomic, etc), however case reports show rare instances of extrapyramidal, cerebellar, sensory and autonomic degeneration. ALS has an estimated annual prevalence of approximately 4 to 6 per 100,000 in the United States. While it most common in adult men (with age of onset typically between 40 and 70), ALS can affect anyone. ALS has an annual prevalence of approximately 4 to 6 per 100,000 in the United States. Its relative rarity as well variable clinical presentation can make diagnosing ALS a challenge. Here we discuss the case of one patient who had received several other diagnoses, both orthopedic and neurologic in nature, prior to the eventual diagnosis of his atypical presentation of ALS.
Keywords: Amytrophic lateral sclerosis; Motor neuron disease; Neurodegeneration
Introduction
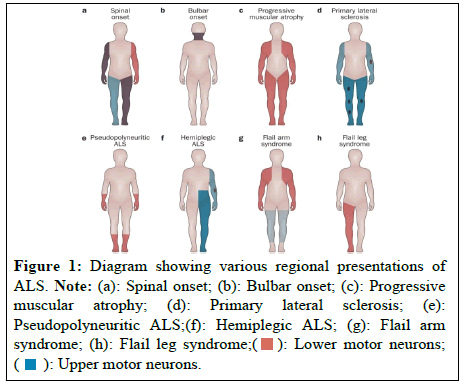
Three distinct phenotypes of ALS have been described (Combined UMN and LMN, also known as Classical or Charcot; UMN predominant; and LMN predominant). Classical ALS accounts for approximately 70 percent of all cases and can be further subdivided into limb onset (ex. Brachial Amyotrophic Diplpegia, Leg Amyotrophic Diplegia) and Bulbar-onset ALS, which are named for the region of the body where the patient’s symptoms first appeared [1-6]. Other less common variants exist, though there is debate as to whether some of these represent separate disorders as opposed to variants of ALS (Figures 1a-1h).
Leg amytrophic diplegia is the most well-known presentation, often featured in popular media, such as the 2014 film The Theory of Everything. In some patients the disease may be limited to single region for many years, while other cases rapidly prove fatal.
Sporadic ALS accounts for more than 90% of all cases. More 40 genes have been associated with the development of ALS. As of sporadic ALS 1 in 10 patients have a related genetic mutation; mean while two out of three case of familial ALS have an associated mutation [7]. Research indicates toxic exposures (such as heavy metals) are associated with development of ALS however the nature of the relationship has not been fully explored [8,9]. Rates of ALS are significantly higher among military veterans, regardless of type (combat versus noncombat) or era of service (World War II versus Korea versus Vietnam) [10]. In a somewhat unprecedented stance, the Veterans Administration presumes ALS to be service connected in any veteran who served more than 90 days on active duty at any point during their career [11]. Veterans are twice as likely as the general population to develop ALS and make up sixteen percent of ALS patients, despite representing around four percent of the general population [8].
Case Presentation
An 83-year-old male with a Pure Motor Hemiplegia (PMH) of hypertension, hyperlipidemia, hypothyroidism, and deep vein thrombosis presented to the emergency department following a fall at home. He is seeking treatment for a three-inch head laceration and a full diagnostic work-up for a multiyear history of progressive, mostly painless weakness that he felt lead to his fall.
The patient was right-handed. He was a non-combat military veteran and a high school graduate. He continued to work as a machinist. The patient was also treated by his Primary Care Physician (PCP) with donepezil for self-reported cognitive decline, however showed no deficits at any time during his admission.
The patient was unsure when the weakness began but he became concerned about progressive proximal muscle weakness in late 2018 or early 2019. At the shooting range he noticed was unable hold up a handgun with his right (dominant) hand alone and needed to use both arms. The patient was seen by his PCP who noted slightly decreased strength in both shoulders but no wasting. The patient was referred to a shoulder specialist at a well-known orthopedic practice. Having previous been treated by the same practice a less than a year prior for right adhesive capsulitis he had the same procedure performed on his left shoulder. His proximal upper extremity weakness did not improve. Eventually the patient also noted proximal lower extremity weakness and possibly some distal upper extremity weakness.
In 2022 the patient was referred to outpatient Neurology where he was worked up for upper extremity weakness. A cervical MRI without contrast showed cervical spondylosis insufficient to explain his symptoms and brain MRI without contrast showed normal age-related changes. Electromyography (EMG) of the upper extremities showed mixed axonal and demyelinating patterns. The patient showed no cranial nerve deficits and sensation was grossly intact. Neck flexion was 2/5 and extension was 1/5. Upper and lower extremity strength were 2/5 proximally and 4/5 distally. Deep tendon reflexes were symmetric throughout, absent in upper extremity and 1+ in the lower extremity. The patient also reported several falls, but denied confusion, sensory changes, or double vision. Also denied difficulty swallowing or choking or incontinence (bowel or bladder).
The patient’s presentation was deemed suspicious for Chronic Inflammatory Demyelinating Polyneuropathy (CIDP). A lumbar puncture and treatment with Intravenous Immunoglobulin (IVIG) was recommended as well as physical therapy. A short course of prednisone was ordered. Other considerations included heritable neuropathies and flail arm syndrome.
The patient continued to live alone. Given that his proximal muscle weakness was so much greater distal (and arms much worse than legs), he was able to complete most of his activities of daily living by swinging his arms to pick desired objects or to bring food to his mouth. This compensation, however, sometimes caused him to lose his balance. Prior to any additional testing or treatment with Neurology, the patient fell at home and was taken to the emergency room. While his injuries were minor at his insistence the patient was admitted for diagnostic work-up.
On presentation the patient’s muscles were visibly atrophied (upper extremity greater than lower extremity) with patient reporting approximately 30-pound weight loss over the past two years. Fasciculations were grossly visible in pec major and rectus femoris. The patient showed a distinctive “man-in-a-barrel” appearance, arms flaccid with relatively intact use of hands. His lower extremities, however, had a similar, though less advanced, appearance.
While admitted to the hospital the patient’s lumbar puncture showed no signs of inflammation and muscle biopsies were normal. Repeat EMG showed diffuse motor predominant axonal loss without clear myogenic units. Patient received a five-day course of IVIG but showed no response. Given that the patient lived alone and had no family nearby, the patient was discharged to a subacute rehabilitation facility. The patient was referred to a nearby ALS clinic affiliated with the Veterans Administration (VA) at a large academic institution. The patient was diagnosed with ALS and his care was coordinated through the VA.
Results and Discussion
This patient’s story, like many others, is evocative of the Indian parable of the blind men and the elephant. As each man approaches the elephant his conclusions are based only on one part of the animal. The man who touches the trunk concludes he is holding a rope, the one at the ear believes he is touching a fan, and so on. This is an alltoo- familiar problem in modern medicine; each specialty seeing and treating select symptoms within their silo.
Furthermore, this patient’s case demonstrates how a slightly lesscommon presentation can result in a diagnosis being missed. This may lead to invasive and unnecessary treatments. Adhesive capsulitis is a common complication of ALS (due to decreased and abnormal joint use) and it is very possible the patient suffered from both conditions. Without the proper diagnosis of ALS, however, the patient’s expectations for recovery were not managed appropriately [12].
This patient was admitted to the hospital at his own insistence. Exasperated after years without answers, he benefited tremendously from the continuity, interprofessional coordination, and testing turnaround time rarely seen in the outpatient setting. For patients requiring a complex diagnostic work-up, navigating the disjointed healthcare system can be especially challenging in the outpatient setting where they run the risk of falling through the cracks.
The culture around and approach to certain diseases, such as cystic fibrosis or ALS, has led to the creation of “one-stop” clinics, where patients can schedule one day with multiple providers and support staff. This level of interdisciplinary communication and coordination is virtually nonexistent for difficult, undifferentiated outpatient diagnostic workups.
This patient’s presentation was particularly unusual. His history is consistent with brachial amyotrophic diplegia, a rare form of ALS that is relatively stable and is typically restricted to the lower motor neurons of the upper extremities [13]. These patients often maintain a high degree of mobility for years many years, as was the case in our patient. His disease predominantly affected the bilateral shoulder girdle; however by the time of presentation his symptoms did involve the pelvic girdle as well as UMN signs (eg. fasciculations). In published case reports, progression to the lower extremities is rare. This patient’s unusual presentation likley complicated his search for answers. So too might the COVID-19 pandemic, which shut down non-urgent, in-person medical appointments for some time. This patient’s exact presentation would have been difficult to appreciate via phone or telehealth.
Conclusion
ALS is the most common form of motor neuron disease and it affects US military veterans at twice the rate as the general population. Most cases are spontaneous though several genetic mutations have been associated with the condition. The progression of the disease (which muscle groups are affected first, the exact mix of upper and lower motor neuron involvement) is heterogeneous, which makes early symptoms difficult to recognize. In patients with a family history of ALS, personal military service, or a significant exposure to heavy metals should be considered at higher risk for ALS. The role of epigenetics in the development ALS is unclear but may play a role in future treatments for the condition.
References
- Swinnen B, Robberecht W (2014). The phenotypic variability of amyotrophic lateral sclerosis. Nat Rev Neurol 10: 661-670.
[Crossref] [Google Scholar] [PubMed]
- Vass R, Ashbridge E, Geser F, Hu WT, Grossman M, et al. (2011). Risk genotypes at TMEM106B are associated with cognitive impairment in amyotrophic lateral sclerosis. Acta Neuropathol 121:373-380.
[Crossref] [Google Scholar] [PubMed]
- The phenotypic variability of amyotrophic lateral sclerosis
- Van Es MA, Hardiman O, Chio A, Al-Chalabi A, Pasterkamp RJ, et al. (2017). Amyotrophic lateral sclerosis. Lancet 390(10107):2084-2098.
[Crossref] [Google Scholar] [PubMed]
- Jawdat O, Statland JM, Barohn RJ, Katz JS, Dimachkie MM (2015). Amyotrophic Lateral Sclerosis Regional Variants (Brachial Amyotrophic Diplegia, Leg Amyotrophic Diplegia, and Isolated Bulbar Amyotrophic Lateral Sclerosis). Neurol Clin 33(4):775-785.
[Crossref] [Google Scholar] [PubMed]
- Swinnen B, Robberecht W (2014). The phenotypic variability of amyotrophic lateral sclerosis. Nat Rev Neurol 10:661-670.
[Crossref] [Google Scholar] [PubMed]
- Mejzini R, Flynn LL, Pitout IL, Fletcher S, Wilton SD, et al. (2019). ALS genetics, mechanisms, and therapeutics: where are we now?. Front Neurosci 13:1310.
[Crossref] [Google Scholar] [PubMed]
- Su FC, Goutman SA, Chernyak S, Mukherjee B, Callaghan BC, et al. (2016). Association of environmental toxins with amyotrophic lateral sclerosis. JAMA neurol 73(7):803-811.
[Crossref] [Google Scholar] [PubMed]
- Re DB, Yan B, Calderón-Garcidueñas L, Andrew AS, Tischbein M, et al (2022). A perspective on persistent toxicants in veterans and amyotrophic lateral sclerosis: identifying exposures determining higher ALS risk. J Neuro 1:1-9.
[Crossref] [Google Scholar] [PubMed]
- Institute of Medicine (2006). Amyotrophic Lateral Sclerosis in Veterans: Review of the Scientific Literature.
- VA News (2008).VA Secretary Establishes ALS as a Presumptive Compensable Illness.
- Burke K, Ellrodt AS, Levine J, Adams T, Allis R, et al (2018). Exploring the use of educational material about shoulder dysfunction: a quality improvement project in people with amyotrophic lateral sclerosis. Am J Phys Med Rehabil. 97(5):379-379.
[Crossref] [Google Scholar] [PubMed]
- Katz JS, Wolfe GI, Andersson PB, Saperstein DS, Elliott JL et al (1999). Brachial amyotrophic diplegia: a slowly progressive motor neuron disorder. Neurology. 1999 Sep 1;53(5):1071-1071.
[Crossref] [Google Scholar] [PubMed]
Citation: Stockton-Brown M (2023) Man-in-A-Barrel: Amytrophic Lateral Sclerosis Misdiagnosed as Rotator Cuff Injury in a Military Veteran. J Alzheimers Dis Parkinsonism 13:573. DOI: 10.4172/2161-0460.1000573
Copyright: © 2023 Stockton-Brown M. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 1789
- [From(publication date): 0-2023 - Oct 21, 2025]
- Breakdown by view type
- HTML page views: 1478
- PDF downloads: 311