Mandibular Sub-Condylar Fractures Conservative Management - Advantages and Disadvantages: A Clinical Study
Received: 04-Dec-2017 / Accepted Date: 28-Dec-2017 / Published Date: 04-Jan-2018 DOI: 10.4172/2376-032X.1000223
Abstract
Background and objective: Mandibular fractures are the most frequent and sub condylar region is a common site of fracture. Proper management of sub condylar fracture is a matter of controversy. Improper management of sub condylar fracture can lead to impaired function and aesthetics. Hence a timely and appropriate management of sub condylar fracture is mandatory. Aim of the study was to evaluate the merits and demerits of conservative management of mandibular sub condylar fractures.
Materials and methods: A total of 430 mandibular fractures were evaluated and out of this 107 had sub condylar fractures. In this study a clinical attempt was made to study comprehensively the conservative management of sub condylar fractures. The factors considered were age, sex, associated fractures of facial bones, treatment and complications.
Results: Among 107 patients 85 males and 22 females had sub condylar fracture. Associated facial bone fractures were seen in 44 cases. There was no complication of ankyloses. Lateral mandibular movement was regained in 82.6% of cases and satisfactory occlusion achieved in all cases.
Conclusion: Based on this study conservative management of mandibular sub condylar fracture gives good results in most of the cases if managed judiciously.
Keywords: Sub-condylar fracture; Conservative management; Inter maxillary fixation; Mouth opening
Introduction
Sub condylar fractures are increasingly seen among trauma victims either alone or in association with other fractures [1]. In contrast to the conventional fracture management, the importance of precise anatomic reduction is unnecessary amongst most of the sub condylar fractures.
Compensations in muscular activity caused by re-education of neural pathways help in restoring good function. This is possible because the condyle is not a load bearing one and is only a joint following a pathway set by articulating surfaces and muscles.
However improper management can lead to trismus, open bite, malocclusion, facial asymmetry, ankyloses etc. hence timely and apt management is necessary.
There is much controversy regarding open reduction and closed reduction in these type of fractures [2,3]. Both have merits and demerits.
The condylar segment is no longer considered to be a growth centre but only a centre of passive growth. In children restitution changes occur to a major degree after condylar fractures but in adults it is mainly remodelling.
The surgical approach of the sub condylar region is also fraught with dangers like facial nerve paralysis, necrosis of the condyle, and a scar.
So fractures of sub condylar region need to be managed differently from fractures elsewhere in the face.
Aims and Objectives
• To evaluate the merits and demerits of conservative management.
• To evaluate the nature and incidence of complications associated with conservative management.
• To evaluate methods by which complications can be reduced.
• To assess the degree of function regained with conservative management.
Materials and Methods
This study was based on the data collected over a period of two years in the department of Oral and Maxillofacial Surgery, Dental College, Thiruvananthapuram.
Total numbers of 430 mandibular fractures were studied and out of these 107 patients had sub condylar fractures.
The data were classified into the following groups.
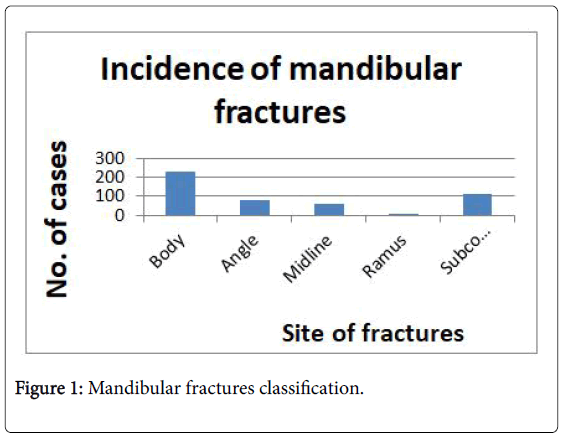
Incidence of mandibular fractures were classified into 5 groups (Figure 1):
• Body
• Angle
• Midline
• Ramus
• Sub condylar
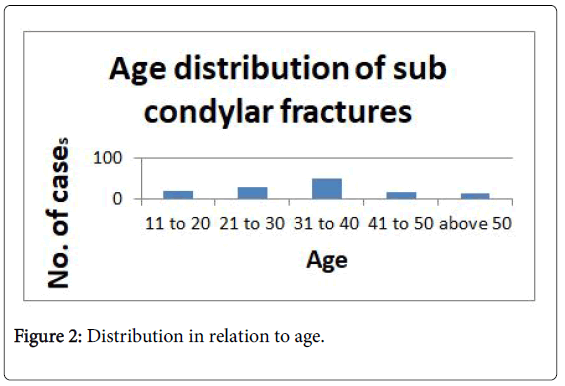
Distribution in relation to age (Figure 2):
• 11 to 20
• 21 to 30
• 31 to 40
• 41 to 50
• Above 50
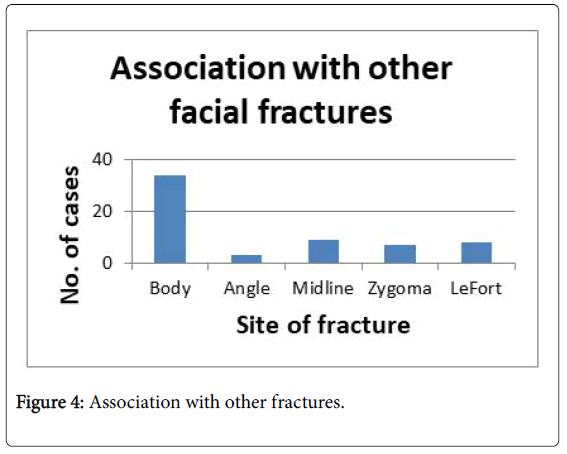
Association with other fractures (Figure 3):
• Body
• Angle
• Midline
• Zygoma
• Le fort
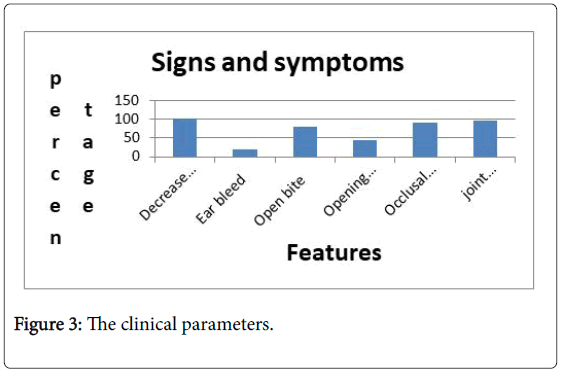
Signs and symptoms
The clinical parameters noted were (Figure 4):
• Open bite
• Reduced mouth opening
• Deviation on opening
• Reduced lateral excursion
• Occlusal derangement
• Bleeding from the ear
Treatment
Patients were divided into 3 groups. Elastic traction to attain occlusion and later IMF followed by functional therapy. Traction with posterior fulcrum to attain occlusion and later IMF followed by functional therapy. Prolonged IMF for associated facial bone fractures followed by intermittent functional therapy.
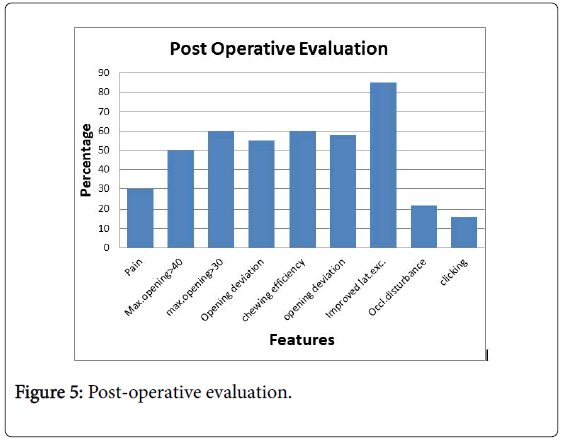
Post-operative evaluation was based on (Figure 5):
• Pain
• Mouth opening >40 mms
• Mouth opening >30 mms
• Chewing efficiency
• Opening deviation
• Improved lateral movement
• Occlusal disturbance
• Clicking
In cases of sub condylar fractures with no displacement simple elastic traction was given to achieve occlusion and was followed by inter maxillary fixation for a period of one week. Depending on the development of occlusal discrepancy selective guiding elastic traction was given which was tapered off.
In fracture displacements posterior bite block and elastic traction were given to achieve occlusion, then followed by IMF for one week and followed up with guiding elastics if necessary.
Associated maxillary or mandibular fractures were reduced either by closed or open reduction methods and occlusion achieved with or without elastic traction and IMF given. The IMF was released every week and mouth opening was done for a few minutes and IMF reapplied. This was carried out for a period of five to six weeks and followed by guiding elastics if deviation on opening was found. In all these cases if post treatment mouth opening deviation was present the patients were taught to give pressure on the side of the mandible to which it is deviating for a few hours per day.
All patients were recalled after treatment at intervals of one week, two weeks and one month and the parameters like mouth opening, deviation on opening, maximum opening, protrusion, lateral excursions, chewing efficacy (nature of diet), pain, presence of open bite, occlusal discrepancy and joint sounds were assessed.
Results
A total number of 430 patients with fractures of mandible were evaluated. Out of this 107 had sub condylar fractures (Figure 1) Males accounted for 85 and females 22. Maximum cases occurred in the age group of 30-40 years (Figure 2).
Associated mandibular fractures were seen in 44 cases. Unilateral body fracture in 21 cases and bilateral fractures in 11 cases. Condylar fractures were associated with angle fractures 1.86%, body 30.89% and 8.4%with midline fractures. Fractures of the midline happened in 2.8% of bilateral sub condylar fractures and in 5.6% of unilateral sub condylar fractures. Zygoma was fractured in 7 cases. Fracture of the midface was associated with 8 cases. Among midface fractures Le Fort II is the commonest (Figure 3).
Signs and symptoms which were helpful in diagnosing fractures are shown in Figure 4. Among 23 cases restriction in mouth opening was seen in all patients. Tenderness over the affected joint in 91.3% of cases. Bleeding from the ear in 17.39%. Open bite in 82.6%. Occlusal discrepancy in 86.95%. Deviation in opening occurred in 56.5%.
Post operatively no incidence of ankyloses. Maximum mouth opening of 40 mm achieved in 43.47% 30 mm or more in 47.82%. Two cases reported clicking sound in the opposite TMJ and one on the same side. However clicking did not prevent movement or caused pain. Pain was present in 26.08% of cases, but not amounting to hinder normal activities of joint. Lateral excursion was regained in 82.6%. Satisfactory occlusion was obtained in all the cases. 21% complained of minor interferences of occlusion on the same side of fracture. Children and teenagers attained perfect occlusion after 2 to 3 months and retained it. They even regained bilateral excursive and protrusive movements. Chewing efficacy was good in 56.53% and moderate in 43.47%. All the associated fractures healed without any issues in spite of frequent mobilization.
Discussion
This study of sub condylar fractures is based on complete evaluation and follow up for 2 years, which is useful for comparative studies based on reports from elsewhere.
In the present study out of 430 patients 107 had sub condylar fractures. This is comparable with the results of the review conducted by Kromer [4]. Majority of fractures occurred in the age group of 30-40 years Carson and Robert [5] reported an average age incidence of 28 years. Carson has reported male to female ration approximately 3:1, which is corroborated by the ratio 4:1 obtained in this study.
Associated fractures of maxillofacial skeleton were seen in 55.1% of sub condylar fractures which is in confirmation with survey conducted by Hall et al. [6]. Unilateral sub condylar fracture were accounted for 75% of the cases. According to Nussbaum ML and Laskin DM [7] 50% of fractures were unilateral. Bilateral sub condylar fracture occurred along with midline in 2.8% of cases. This is far less than 9.6% of cases as reported by Rowe and Killey [8].
Bleeding from the ear was present in 17.3% of fractures. This was due to the laceration of the anterior wall of external auditory meatus produced by the impact of the condyle head against skin in this region.
In bilateral sub condylar fractures where there was an associated fracture of the body, there was no deviation, probably because of the loss of lateral pterygoid muscle activity and because of the muscle spasm which tries to eliminate or minimize movement between fracture ends. All the patients had restriction in mouth opening may be due to pain at the fracture site, reflex muscle spasm, oedema, laceration or mechanical obstruction
The commonest clinical finding in sub condylar fracture in this study were tenderness over the affected joint 91.3%, open bite 82.6% and occlusal discrepancy 86.95%.
In the present study all the cases were treated non-surgical as the displacement of condylar process was not in such a magnitude and direction that was impossible to restore normal occlusion which is in accordance with the study of Lyons CJ [9]. Experiences of various authors like Carson [6], Mac Lennan [10] Gerry [11] etc. have shown that good results can be obtained by conservative management and functional therapy. Secondly surgical treatment in the TMJ region may result in complications resulting in facial nerve as well as other problems. Thirdly open reduction leaves a scar on the face. These all are supported by the results of Chalmer J [9]. Conservative management is preferable in economic point of view and also hospitalisation can be avoided.
Management has long been a matter of controversy. Only a critical unbiased appraisal of on a large series can only indicate any advantage of treatment option over the other. In all studies time plays an important role. The results in this study support Mc Lennan’s [10] statement that there is every justification in treating the vast majority of mandibular condylar fractures by conservative means. Even though many authors had advised surgical reduction in grossly displaced fracture dislocations, elastic traction with posterior bite blocks either unilateral or bilateral as the case requires, and continued guiding elastics were adequate in all cases of fracture dislocation.
We did not assess the growth disturbance caused by the fracture in children because of the short period of study and since we did not have any children in the age group between 1 and 5 years.
After achieving occlusion we gave IMF for a period of one week following Rowe and Killey [8] but against the advice of Dingman and Natvig [12] or Kazangian and Converse [13]. We gave much importance to the functional treatment to eliminate ankyloses, is against the principle of Glineberg [14]. Our aim was to recover the lost function and not precise anatomic reduction. This allowed us to do intermittent exercise even in cases where an associated body fracture was also present. Subjective symptoms in the form of pain occurred in 26.8% of the cases which is comparable with the observation of Niezen ET [15].
If conservative treatment can deliver satisfactory results with minimum complications there is no justification for surgical exploration and reduction in the TMJ area which has too many hazards. None of the patients developed rare complications such as Frey’s syndrome [16], mandibular nerve anaesthesia [17], cervical spine injury [18], facial palsy, causalgia of buccal nerve (Egyedi) [19] etc.
Conclusion
All the patients were treated conservatively with or without elastic traction depending on the degree of discrepancy and open bite followed by rigid inter maxillary fixation for a minimum period of seven days followed by functional therapy.
A significant finding in this study was that in children and teen ages the returns to normal functional movements were outstanding. This study also highlights that the simplest method of treatment which will produce good results is the treatment of choice.
Our study has many limitations since the sample size and period of study is relatively short.
However from this study we can empathetically state that conservative management of mandibular sub condylar fracture gives good results if managed judiciously.
References
- Lindahl L (1977) Condylar fractures of mandible. Int J Oral Surg 6: 12.
- Shiju M, Rastogi S, Gupta P, Kukreja S, Roy T, et al. ( 2015) Fractures of the mandibular Condyle. Open versus closed. A treatment dilemma. J Craniomaxillofac Surg 43: 448-451.
- Rastogi S, Sharma S, Kumar S, Reddy MP, Prasad N (2015) Fractures of mandibular condyle -to open or not to open: An attempt to settle the controversy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 119: 608-613.
- Kromer H (1953) Closed and open reduction of condylar fractures. D record 73: 569.
- Blevins C, Gores RJ (1961) Fractures of the mandibular condyloid process: Results of conservative management in 140 patients. J Oral Surg 19: 392.
- Hall RK, Thomas G (1980) Ten year survey of traumatic injuries to face and jaw of children 1970-1979- a computer analysis. Paper presented at 8th international conference in oral surgery, Berlin.
- Nussbaum ML, Laskin DM (2008) Closed versus open reduction of mandibular condylar fractures in adults. J Oral Maxillofac Surg 66: 1087-1092.
- Rowe NL, Killey HC (1955) Fractures of the facial skeleton. Churchill Livingstone, UK.
- Lyons CJ (1947) Fractures involving the mandibular condyle: A post treatment survey of 120 cases. J Oral Surg 5: 45.
- Lennan WDM (1969) Fractures of the mandibular condyles. Br J Oral Surg 7: 31.
- Kazanjian VH, Converse JM (1974) Surgical treatment of facial injuries. Williams and Wilkins, Baltimore.
- Glineberg RW, Laskin DM (1982) The effects of immobilization on the primate temporomandibular joint. A histological and histochemical study. J Oral Maxillofac Surg 40: 3.
- Niezen ET, Stuive I, Post WJ, Bos RR, Dijkstra PU (2015) Recovery of mouth opening after closed treatment of fracture of the mandibular condyle: A longitudinal study . Br J Oral Maxillofac Surg 53: 170-175.
- Hogemann KE (1951) Surgical orthopaedic correction of mandibular protrusion. Acta Chir Scand 159: 26-28.
- Laws IM (1972) Two unusual complications of fractured condyles. Br J Oral Surg 38: 50.
- Bruce Danoff (1973) Management of condylar fractures in patients with cervical spine injury- report of case. J Oral Surg.
- Fonsica RH, Barber HD, Powers M, Frost DE (2012) Oral and maxillofacial trauma (4th edn.). Saunders Elsevier, Philadelphia.
Citation: Ajithkumar K, Rabi A, Jayakumar K (2018) Mandibular Sub-Condylar Fractures Conservative Management - Advantages and Disadvantages: A Clinical Study. J Interdiscipl Med Dent Sci 6: 223. DOI: 10.4172/2376-032X.1000223
Copyright: ©2018 Ajithkumar K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 5297
- [From(publication date): 0-2018 - Dec 27, 2024]
- Breakdown by view type
- HTML page views: 4564
- PDF downloads: 733