Research Article Open Access
Management of Giant Inguinoscrotal Hernia in Resource Limiting Setting
Roger Lebeau*, Kouakou Ibrahim Anzoua, Mamadou Traoré, Ismael Leh BI Kalou, Ahou Bernadette N’Dri, Aka Gérard Kakou and Bamourou DianéGeneral and Digestive Surgery Department, Bouaké Teaching Hospital, Cote D'ivoire
- *Corresponding Author:
- Dr.Roger Lebeau
Medical Doctor, General and Digestive Surgery Department
Bouaké Teaching Hospital, 01 P.O. box 376 Bouaké 01, CoteD'ivoire
Tel: (00225) 49764588
E-mail: lebeauroger@yahoo.fr
Received date: November 15, 2015, Accepted date: December 22, 2015, Published date: January 02, 2016
Citation: Lebeau R, Anzoua KI, Traoré M, Kalou ILBI, N’Dri AB, et al. (2016) Management of Giant Inguinoscrotal Hernia in Resource Limiting Setting. J Gastrointest Dig Syst 6:376. doi:10.4172/2161-069X.1000376
Copyright: © 2016 Lebeau R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Purposes: To describe our experience in the management of giant inguino-scrotal hernia outlining the epidemiological, clinical profil, treatment and outcome after treatment. Methods: A Descriptive and retrospective study was carried out of giant inguino-scrotal hernia seen between 2007 and 2014 at Bouaké teaching hospital in the central part of our country (Côte d’Ivoire) and during free rural medical missions for hernia treatment organized by a non governemental organization. A structured questionnaire was designed including for each patient, socio-demographic data, clinical profil, treatment and outcome after treatment. Results: During the period under study 30 patients with giant inguino-scrotal hernia were taking in charge. The ages of our patients ranged from 15 to 60 years with a mean age of 48.5 years. The duration of symptoms ranged 5 to 25 years with a mean of 10.2 years. Reasons for late presentation were mainly financial constraints (n=11). Hernia was irreducible in four patients. A pre-operative progressive pneumoperitoneum was conducted in those four patients. During operation reduction of the hernia content into the abdominal cavity was impossible in one patient. In this patient a debulking left hemicolectomy with colo-rectal anastomosis was necessary. Hernia repair was conducted in all patients, with Lichtenstein procedure (n=10), Shouldice procedure (n=7) Bassini’s procedure (n=7), Mc Vay’s procedure (n=4) and Stoppa’s procedure (n=2). Abdominal compartment syndrome (ACS) occurred per operatively in three patients. Two of them underwent emergency midline laparotomy followed by an exclusive skin closure and the third patient died on the operating table. In post-operative period scrotal hematoma was found in 12 patients (41.4%), suppuration of the inguinal wound in 3 patients and scrotal seroma in 2 patients. The average length of hospital stay was 4.75 days (3 days to 9 days) and after a mean follow up period of 29.19 months (range 7 months to 53 months), no recurrence was observed.
Keywords
Giant inguino-scrotal hernia; Hernioplasty; Hernioraphy; Abdominal compartement syndrome
Introduction
Inguinal hernia is one of the most common general surgical operation world wide accounting for 10-15% of all surgical procedures [1,2]. In part of Africa the anormal incidence of inguinal hernia is as high as 175% per 100.000 people [3]. However, less than 40% are actually repaired, resulting in many patients developing long standing inguino-scrotal hernia. The long standing evolution of inguino-scrotal hernia can result in the development of giant inguino-scrotal hernia (GISH) whose management poses therapeutic challenges to surgeon in resources limited country [4]. For the purpose of this study we define giant inguino-scrotal hernia as an inguino-scrotal hernia extending below the midpoint of inner thigh of the patient in standing position [5]. Surgical repair is often challenging and difficult because of loss of domain. Reduction of contents in giant inguinal hernia may lead to cardiopulmonary arrest due to elevation of intra-abdominal pressure and elevation of diaphragm [6]. Once the hernia reduced the surgeon has to face the problem of the parietal repair and treatment of residual redundant scrotum which leave room for plastic surgery [6]. Because of poor socio-economic status and non affordability of patient in our country, modern inguinal repair procedure (mesh, laparoscopic) cannot be always used and as a result hernioraphies are still practiced. To our knowledge only one study had deal with the management of giant inguino-scrotal hernia in our country [7]. Thus this study aimed to describe our experience in the management of giant inguino-scrotal hernia outlining the epidemiological, clinical profil, treatment and outcome after treatment.
Patients and Methods
This was a descriptive retrospective study of patients operated on for giant inguino-scrotal hernia between January 1st, 2007 and June 30th, 2014 by the authors at Bouaké teaching hospital in the central part of the country (Côte d’Ivoire) and during free rural medical missions programmes for hernia treatment organized under the auspices of a non governemental organization in various rural communities of central and northern parts of the country. Bouaké Teaching Hospital is a 283-bed urban public hospital. The hospital is a tertiary referral centre and serves urban and rural population from Bouake’s agglomeration but also from the whole central and northern parts of the country. Bouaké city is located in the central part of the country (Ivory Coast). During the free rural medical missions programmes for hernia treatment, our surgical team moved in rural communities. The patients were taking in charge in the hospital of the nearest town. The surgical team of the local hospital was invited to join our team so that the patients were managed together. At the end of the mission the local surgical team ensured the patients follow up.
A structured questionnaire was designed including for each patient, socio-demographic data, (age, occupation), region of residence (rural or urban), whether the hernia impede quality of life, clinical presentation, duration of symptoms prior to presentation, side affected, reason for late presentation, reason why the patient is now presenting, whether primary or recurrence hernia, co-morbidities, if the phallus is completely burried by the mass, if the patient is able to reduce the mass, the local aspect of the skin, ASA status [8], type of anesthesia and surgical procedures, postoperative complications, hospital stay, mortality and follow up. During free rural medical missions programmes for hernia treatment, Giant inguino-scrotal hernia we dealt with were primary reducible hernia with no major trophic changes in the scrotal skin.
Results
During the period under study, a total of 2153 patients with inguinal hernia were taken in charge; ie 403 patients in Bouaké teaching hospital and 1750 patients during the free rural medical missions’ programmes for hernia treatment.
Over the 2153 patients, 30 patients presented with giant inguinoscrotal hernia; fourteen patients (n=14) in Bouaké teaching hospital and 16 patients during the free medical mission. The ages of our patients ranged from 15 to 60 years with a mean age of 48.5 years.
Twenty patients (66.7%) were peasants coming from the rural areas; they were laborer (n=7), farmer (n=10) and fisherman (n=3), the remaining 10 patients were citizen. A history of having lifted heavy weigth was ascertained in 7 of them as they do heavy work. A medical pathology (co-morbidity) was noticed in 19 patients (Table 1). The duration of symptoms ranged 5 to 25 years with a mean of 10.2 years. The reasons for late presentation are shown in Table 2.
| Medical Pathology | Frequency | Percentage |
| Hypertension | 6 | 31.67 |
| Cardiopathy | 4 | 21.05 |
| Diabetes mellitus | 4 | 21.05 |
| Pneumonitis | 2 | 10.52 |
| Mental disorder | 2 | 10.52 |
| HIV infection | 1 | 5.26 |
Table1: Patient’s medical pathology.
| Reasons for late presentation | Frequency | Percentage |
| financial constraints | 11 | 36.67 |
| long distance from health facilities | 5 | 16.67 |
| fear of surgery | 4 | 13.33 |
| treated by traditional healers | 4 | 13.33 |
| relatives advice against surgery | 3 | 10 |
| refusal to undergo surgery | 2 | 6.67 |
| no clear reason | 1 | 3.33 |
Table 2: The reasons for late presentation (n=30).
All patients were referred both for cosmetic reason and also because they were suffering from functional problems affecting their everyday lives. All the patient had difficulty in finding suitable clothes, 40% of patients (n=12) had difficulty in standing, walking, sitting or lying down, 60% of patients (n=18) had difficulty to penetrate their partners during sexual intercourse and five patients had no sex since the last 3 years because of continuous refusal of theirs partners. Nineteen (n=19, 63.3%) patients had right sided hernia and eleven (n=11, 36.7%) had left sided hernia.
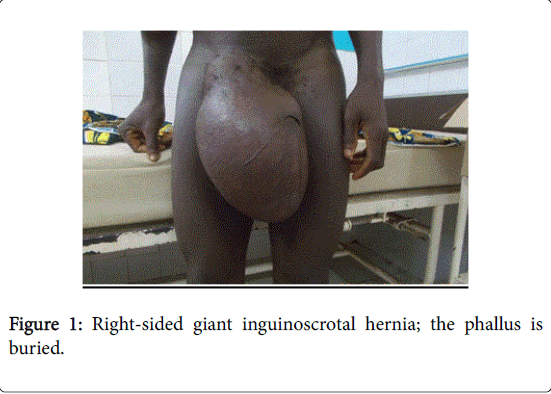
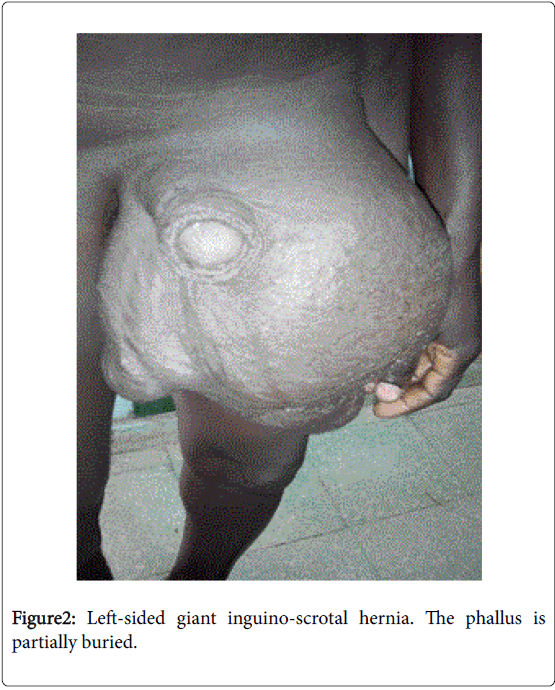
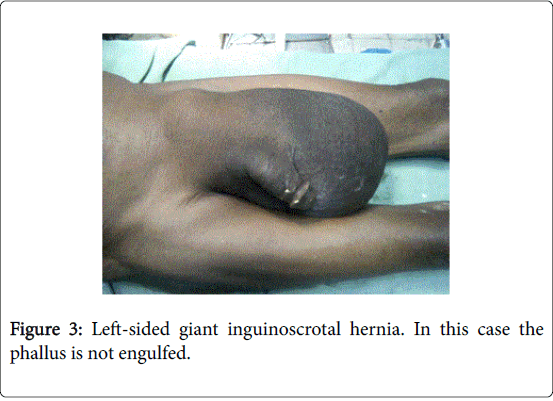
Five patients presented with recurrence of previous open operation. While standing the hernia exceeded mid-thigh (n=24) (Figures 1-3), reached the knee (n=5) (Figure 4) or exceeded it (n=1). Seventeen (n=17 56.7%) patients had dermatitis, candidiasis or excoriation of the scrotum and thirteen patients (n=13 43.3%) had normal scrotum. The penis was buried in 63.3% of cases (n =19) (Figures 1, 3 and 4) and normal in 36.7% of cases (n=11).
Nine patients had bilateral hernia as five giant inguino-scrotal hernia were associated with a left inguinal hernia and four giant inguino-scrotal hernias were associated with a right inguinal hernia (n=5). Two patients had associated umbilical hernia (Figure 4). The hernia was totally reducible in seventeen patients, partially reducible in nine patients and irreducible in the remaining four patients. While urinating, urines were dribbling over the scrotal skin in 19 patients (63.3%).
According to the physical status scale of American Society of Anesthesiologists (ASA class), 14 (46.6%) patients had ASA class I, 8 (26.6%) patients had ASA class II, 5 patients (16.6%) had ASA class III and 3 patients (10%) had ASA class IV . Surgery was preceded by a scrotal skin preparation in seventeen patients and a pre-operative progressive pneumoperitoneum in the four patients who had totally irreducible hernia. Surgery were performed under spinal anesthesia (n=17), general anesthesia (n=8) and local anesthesia (n=5);no shift from spinal or local anesthesia to general anesthesia was recorded. We performed inguinal incision in all patients but two; patients with bilateral inguinal hernia underwent bilateral inguinal incision. The contain of the hernia sac are shown in Table 3. Peroperatively reduction of the hernial content back into the abdominal cavity was easy in 20 patients, necessitated enlargement of internal ring in nine patients and was impossible in one patient. In this patient a debulking left hemicolectomy with colo-rectal anastomosis was necessary to permit hernia reduction. The hernial sac was tied off proximally and the cord structures and testis were spared. The distal part of the sac was left in the scrotum. The previously enlarged internal inguinal ring was closed with interrupted non-absorbable monofilament sutures. Hernia repair was conducted in all patients; Table 4. Redundant scrotum skin was found in all patients and was not resected. It was drained in all cases.
| Contents of the Hernia Sac | Frequency | Percentage |
| Loops of small bowel+cecum+appendix | 11 | 36.67 |
| Loops of small bowel +transverse colon+omentum | 6 | 20 |
| Loops of small bowel +sigmoid colon | 5 | 16.67 |
| Loops of small bowel + transverse colon+sigmoid colon | 4 | 13.33 |
| Loops of small bowel +omentum+ urinary bladder | 4 | 13.33 |
Table 3: The contents of the hernia sac (n=30).
| Hernia repair methods | Frequency | Percentage |
| Lichtenstein procedure | 10 | 33.34 |
| Shouldice procedure | 7 | 23.33 |
| Bassini’s procedure | 7 | 23.33 |
| Mc Vay’s procedure | 4 | 13.33 |
| Stoppa’s procedure | 2 | 6.67 |
Table 4: Hernia repair methods.
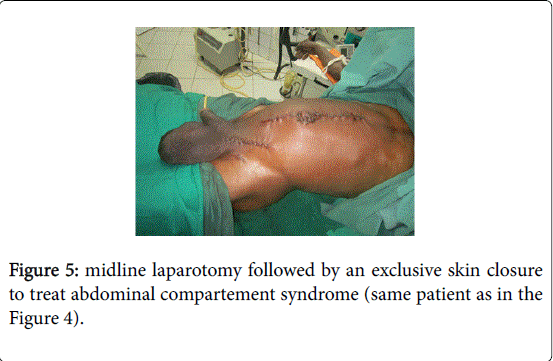
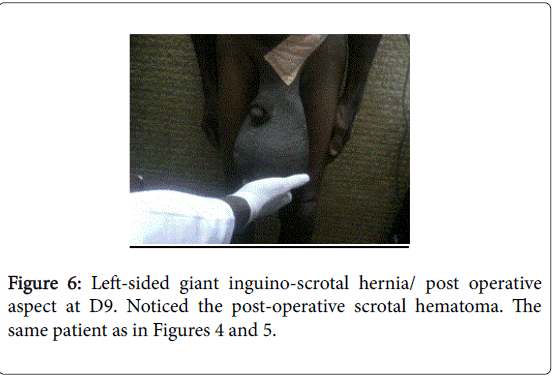
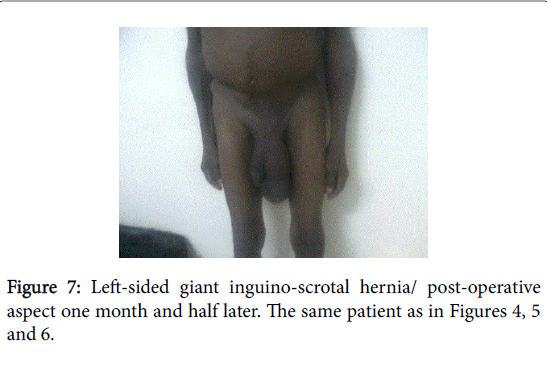
Peroperatively abdominal compartment syndrome (ACS) occurred in three patients. Two of them underwent emergency midline laparotomy followed by an exclusive skin closure (Figure 5) and the remaining patient died on the operating table. In the postoperative period scrotal hematoma was found in 12 patients (41,4%) (Figures 6 and 7), suppuration of the inguinal wound in 3 patients and scrotal seroma in 2 patients. The average length of hospital stay was 4.75 days (range 3 days to 9 days). The mean follow up period was 29.19 months (range 7 months to 53 months); no recurrence was observed. However, the two patients who had laparotomy to treat abdominal compartment syndrom suffered from abdominal incisional hernia and underwent mesh hernioplasty 6 and 8 months later.
Discussion
Inguinal hernia is a public health problem in Africa [9]. However the giant inguino-scrotal hernias are rare but existing entities [10-12]. Their frequency varies in dependence with different factors [13-15]. To the best of our knowledge this is the largest series of GISH ever reported in the medical literature of our country [7]. Our series of 30 cases is linked to the accessibility of care during the free rural medical missions for hernia treatment as we went in the rural area for the recruitment of patients. As matter of fact 16 of our 30 patients were operated on during those medical missions.
The delay in consultation is multifactorial as stated by Mabula [9]. In our series, the main reason for delayed consultation was financial problems. Though such hernia impedes their quality of life patient’s didn’t seek for treatment until family, community and outside financial support allowed them to. Skin manifestation was in the form of scrotal dermatitis, candidiasis or excoriation [10,16]. Such complication are due to the discharge of urine during urination in a tight scrotum [6]. We didn’t found any of scrotal necrosis as stated by Saadi et al. [17]. GISH may be responsible for a "loss of domain [6,18].These hernias accounted for 13.8% of our series as 4 patients had irreducible hernia. In such patient the abdominal cavity has become adapted to being empty. Reintegration of abdominal content can lead to sudden increase of intra-abdominal and thoracic pressures that can cause difficulty in closing the abdomen and lead to respiratory complications [19,20]. To avoid these complications, several techniques and devices have been proposed such as preoperative progressive pneumoperitoneum [21] and visceral or bowel resection [16,22-24]. In our study, despite the progressive preoperative pneumoperitoneum performed over a two weeks period, one patient underwent a debulking hemicolectomy to reduce the amount of viscera reduced back into the abdomen and, abdominal compartement syndrome occurred in the remaining tree patients. This means that when dealing with GISH with abdominal loss of domain pneumoperitoneum does not always lead to re-expansion of the abdominal cavity as some amount of air filled in the hernial sac [23,25]. To address abdominal compartement syndrome in the present study, no bowel resection was performed but emergency midline laparotomy followed by an exclusive skin closure. This technique has been successfully developed by others authors [26,27]. In the others patients of our study who had partially or totally reducible hernia, one can consider that the abdominal cavity is already prepared for the reinstatement of the viscera, and there is no increase in intraabdominal or intrathoracic pressure. The use of prosthetic material is the best method to strengthen the parietal defect. As several patients are unable to afford the cost of prothetic material [7], mesh procedure was used in only one third of our patients [Lichtenstein procedure (n=10), Stoppa’s procedure (n=2)]. Treatment of redundant scrotum is a problem and how to deal with it differs from one author to another [14,22,28]. In our series, all patients had scrotal conservation and evolution has made to scrotal retraction. Scrotal hematoma and seroma are others major postoperative complications in the management of GISH [6,7]. We found 57.14% of scrotal hematoma and 9.52% of seroma. Unlike to Abdul [29] who found 41.6% of post operative hematoma and El - Dessouki [27] who reported 37.5% of postoperative seroma. To deal with those complications various devices such as draining, and the bandage are used by several authors [23,30].
The recurrence rate is variable and may reach 30% of cases [30]. After a mean follow up period of 29.19 months we did not notice any recurrence. The limitation of this study is the short duration of follow up carried out so far considering the high rate of reccurence associated with hernioraphy procedure.
Conclusion
Giant inguino-scrotal hernias are common in Africa and particularly in rural areas. Financial constraint and lack of awareness are responsible for delay in consultation. Surgical repair is challenging and correlated with significant morbidity and mortality due to increased intra-abdominal pressure. Application of appropriate technique for the individual patients is the key to success treatment. Free access health care in rural areas could reduce the occurrence of this condition.
References
- Primatesta P, Goldacre MJ (1996) Inguinal hernia repair: incidence of elective and emergency surgery, readmission and mortality.Int J Epidemiol 25:835–839.
- Schoots IG, van Dijkman B, Butzelaar RM, van Geldere D, Simons MP (2001) Inguinal hernia repair in the Amsterdam region 1994-1996. Hernia 5: 37-40.
- Nordberg EM(1994) Incidence and estimated need of caesarean section, inguinal hernia repair, and operation for strangulated hernia in rural Africa. Br Med J 289:92–93.
- Forrest J (1979) Repair of massive inguinal hernia: with pneumoperitoneum and without using prosthetic mesh. Arch Surg 114: 1087-1088.
- Trakarnsagna A, Chinswangwatanakul V, Methasate A(2014) Giant inguinal hernia: Report of a case and reviews of surgical techniques. International Journal of Surgery Case Reports5: 868–872.
- Coetzee E, Price C, Boutall A (2011) Simple repair of a giant inguinoscrotal hernia. Int J Surg Case Rep 2: 32-35.
- Savoie P-H, Abdalla S, Bordes J et al (2014) Surgical repair of giant inguinoscrotal hernias in an austere environment: leaving the distal sac limits early complications. Hernia 18:113-118
- Keats AS (1978) The ASA classification of physical status--a recapitulation. Anesthesiology 49: 233-236.
- Mabula JB, Chalya PL (2012) Surgical management of inguinal hernias at Bugando Medical Centre in northwestern Tanzania: our experiences in a resource-limited setting. BMC Res Notes 5: 585.
- Akpo EE (2013) Bilateral giant inguinoscrotal Hernia: psychosocial issues and a new classification. Afr Health Sci 13: 166-170.
- Kombo BB, Allison AB (2013) Giant inguino-scrotal hernias seen at the University of Port Harcourt Teaching Hospital. Niger J Med 22: 317-318.
- Bonnet S, Bertani A, Abdalla S (2013) Prise en charge chirurgicale des volumineuses hernies inguinoscrotales avec des ressources limitées en Afrique. Médecine et santé tropicale 23:11-15.
- Fadiran OA, Lawal OO, Jeje J, Bankole O, Oyero T (1992) Giant inguino scrotal hernia: a case report. Cent Afr J Med 38: 127-130.
- Hodgkinson DJ, McIlrath DC (1984) Scrotal reconstruction for giant inguinal hernias. Surg Clin North Am 64: 307-313.
- Vasiliadis K, Knaebel HP, Djakovic N, Nyarangi-Dix J, Schmidt J, et al. (2010) Challenging surgical management of a giant inguinoscrotal hernia: report of a case. Surg Today 40: 684-687.
- Patsas A, Tsiaousis P, Papaziogas B, Koutelidakis I, Goula C, et al. (2010) Repair of a giant inguinoscrotal hernia. Hernia 14: 305-307.
- El Saadi AS, Al Wadan AH, Hamerna S (2005) Approach to a giant inguinoscrotal hernia. Hernia 9:277–279.
- Koontz AR (1958) Hernias that have forfeited the right of domicile: use of pneumoperitoneum as an aid in their operative cure South Med J 51:165-168.
- Trivellini G, Zanella G, Danelli PG, Pratolongo D, Ferri O (1984) [Surgical treatment of large eventrations. Study of a technic adapted to disorders of respiratory compliance]. Chirurgie 110: 116-122.
- Munegato G, Brandolese R (2001) Respiratory physiopathology in surgical repair for large incisional hernias of the abdominal wall. J Am Coll Surg 192: 298-304.
- Goni Moreno I (1975) The rational treatment of hernia and chronic eventrations: preparation with progressive pneumoperitoneum. In: Nyhus LM, Condon RE, editors. Hernia. 2nd edition. Philadelphia: JB Lippincott Co; 5360-5363.
- Mehendal FV, Taams KO, Kingsnorth AN (2000) Repair of a giant inguinoscrotal hernia. Br J Plast Surg 53: 525-529.
- Kovachev LS, Paul AP, Chowdhary P, Choudhary P, Filipov ET (2010) Regarding extremely large inguinal hernias with a contribution of two cases. Hernia 14: 193-197.
- Serpell JW, Polglase AL, Anstee EJ (1988) Giant inguinal hernia. Aust N Z J Surg 58: 831-834.
- Turner EJ, Malhas A1, Chisti I, Oke T (2010) Management of a giant inguinoscrotal hernia with an ulcerated base in a patient with cardiac disease. J Surg Case Rep 2010: 9.
- Merrett ND, Waterworth MW, Green MF (1994) Repair of giant inguinoscrotal inguinal hernia using marlex mesh and scrotal skin flaps. Aust N Z J Surg 64: 380-383.
- El-Dessouki NI (2001) Preperitoneal mesh hernioplasty in giant inguinoscrotal hernias: A new technique with dual benefit in repair and abdominal rooming. Hernia 5: 177-181.
- Tahir M, Ahmed FU, Seenu V (2008) Giant inguinoscrotal hernia: case report and management principles. Int J Surg 6: 495-497.
- Abdul GD, Abdul RS, Sannuallah M(2009) Management of giant inguinal hernia. JLUMHS 8: 29-33.
- Beitler JC, Gomes SM, Coelho ACJ, Manso JEF (2009) Complex inguinal hernia repairs. Hernia 13:61-66.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 13710
- [From(publication date):
February-2016 - Jul 17, 2024] - Breakdown by view type
- HTML page views : 12979
- PDF downloads : 731