Management of Chronic and Neuropathic Pain in Argentina - Evidence, Gaps and Approach
Received: 25-Jul-2022 / Manuscript No. JPAR-22-71741 / Editor assigned: 27-Jul-2022 / PreQC No. JPAR-22-71741 / Reviewed: 10-Aug-2022 / QC No. JPAR-22-71741 / Revised: 16-Aug-2022 / Manuscript No. JPAR-22-71741 / Published Date: 23-Aug-2022 DOI: 10.4172/2167-0846.1000456 QI No. / JPAR-22-71741
Abstract
Given the different approaches in the management of chronic and neuropathic pain in some developing countries, the present study identified data gaps in patient journey touch-points and proposed solution strategies. The present semi-systematic review included MEDLINE, Embase, and BIOSIS databases and additional sources (Google, Argentine Ministry of Health website and Incidence and prevalence database, and World Health Organization). Fulltext studies on chronic and neuropathic pain in English published from 2010 to 2019 were included. To supplement the data gaps, anecdotal data were provided from local experts. Studies/records without any information on chronic or neuropathic pain, editorials, letters to the editor, thesis abstracts, case studies, or studies regarding patient subgroups or nationally unrepresentative populations were excluded. Weighted or simple means were calculated for the overall data, and the synthesized evidence was represented as an evidence gap map. Of 201 retrieved studies/records, five studies/records met the inclusion criteria. The overall prevalence of patients with chronic pain was low (11%). Despite higher health literacy (62.5%) and patient awareness (70%), treatment accessibility for chronic low back pain (CLBP) was poor. However, the reverse scenario was observed with lower awareness (10%), and a higher number of treated patients (>75%) were found in osteoarthritis (OA). Neuropathic pain-related patient journey mapping indicated alarming values for each touch-point. Patients with chronic pain achieved better pain management than those with neuropathic pain. For better management of patient journey touch-points, adherence to treatment guidelines is warranted. • The patient journey in chronic pain and neuropathic pain in Argentina is non-linear. • There is a great paucity of epidemiology data for both chronic and neuropathic pain in Argentina. • Despite the high degree of health literacy and patient awareness regarding chronic pain, pooled values indicate poor access to diagnostic and therapeutic care in Argentina for such patients. • Neuropathic pain management scenario is even worse than chronic pain with no noticeable positive values from pooled estimates. • As a solution, availability of the latest knowledge, update in the current guidelines, training on differential pain management, continuing medical education, and a multi-sectoral approach in care could be recommended
Keywords: Chronic Pain; Neuropathic Pain; Patient Journey; Prevalence; Management; Non-communicable diseases
Keywords
Chronic Pain; Neuropathic Pain; Patient Journey; Prevalence; Management; Non-communicable diseases
Introduction
Chronic and low back pain has taken a great toll on the global health systems, affecting 20% of the total population globally [1]. According to the published literature, limited information on pain epidemiology is available in developing countries like Argentina. A study by Pierobon A et al. in 2020 reported that the life-time prevalence of low back pain (LBP) was 88.4% (95% CI 82.6-94.5) [2]. However, being a potentially debilitating condition, chronic pain has also serious implications on the quality of life as it coexists with anxiety and depression [3]. Furthermore, chronic pain could result in loss of interest, and interference with the person’s eating ability, sleep, and concentration, thereby resulting in loss of productivity and mobility. It also results in a great reduction of immune system and strength, rendering the patient more vulnerable to various co-morbidities [4].
In low- and middle-income countries like Argentina, chronic pain often remains underreported and underdiagnosed, thus mounting the burden on the health system [5]. From the care provider’s perspective, the availability of expert resources like physiotherapists is not deployed at the primary care level to ascertain first contact with the patients. Chronic pain management in Argentina usually follows both local and Regional clinical practice guidelines [6,7,8].
Even though the rate of physicians per inhabitant is similar (or even higher) to the corresponding rate in other countries (in Latin America and Europe), the total number of pain specialists is still low. Many medical education programs are in place in order to correct this deficiency.
Another challenge lies in the overutilization of imaging resources for the diagnosis of LBP, hampering the safety of the patients [9]. Also, due to poor knowledge of work ergonomics, LBP was the third major cause of work-related injury (similar to what is seen in developed countries, and in other countries in the region) [10]. Although some positive steps and strategies have been adopted to resolve the affordability issues of opioids, there has been little information available on its use impact in the Latin American region [11, 12].
While it is evident that mapping patient journeys would provide meaningful insights into the management of pain, there has been no such research literature available exploring patient journeys [13]. Therefore, the current semi-systematic review aimed to synthesize available data on the prevalence, screening, diagnosis, management, awareness, adherence, and impact of QoL of patients with chronic low back pain (CLBP) and neuropathic pain (NP) in Argentina. The study also aimed to identify gaps across patient journey touch-points that can support decision-making in Argentina.
Methods
Overview
The study used evidence mapping and semi-systematic review approach using a scientific literature database, records from unstructured search and anecdotal evidence from local experts. It is followed by validation, synthesis, and quantitative mapping of the prevalent data and different patient disease journey touch-points including disease awareness, screening, and diagnosis, treatment, adherence and control of patients with chronic and neuropathic pain in Argentina over a period of 10 years. Methods of conducting the review were documented in advance as Mapping the Patient Journey Towards Actionable Beyond the Pill Solutions (MAPS) [14]. Chronic pain was defined as pain lasting for >3 months, including osteoarthritis (OA) and LBP. Neuropathic pain was defined as pain due to lesions or disease of the somatosensory system, including diabetic peripheral neuropathy (DPN) and LBP with a neuropathic component. Six steps were used to construct the evidence map:
i) Developing a comprehensive search strategy;
ii) Establishing the inclusion and exclusion criteria;
iii) Screening and shortlisting;
iv) Supplementing with additional and/or local data;
v) Data extraction and synthesis; and
vi) Evidence mapping.
Structured and unstructured literature search
The structured literature search was conducted using the MEDLINE, Embase, and BIOSIS electronic databases using search terms for chronic pain and DPN, their prevalence, and patient journey touch-points for both conditions. Search was performed for published literature in the English language with full-text and data bases filtered for a search time limit of 10 years, from 01 January 2010 to 20 December 2019 to include all studies related to chronic and NP in Argentina. To address data gaps in structure search, unstructured literature search was conducted in Google Scholar, the World Health Organization (WHO), Incidence and Prevalence Database, and the Ministry of Health of Argentina with no restrictions on date limits identified in the additional searches. Duplicate records were removed and the most recent evidence was retained for inclusion in the analysis. The search strategy is presented in Appendix-1.
Inclusion and exclusion criteria
Studies/records were eligible for inclusion if they were i) systematic review and/or meta-analysis, randomized controlled study, observational study, narrative reviews (both full-texts articles published and conference abstracts), ii) the age of the adult population of patients was ≥18 years old and above with NP, iii) reporting quantitative epidemiological data from patients’ journey touch-points for chronic and NP, including awareness, screening, diagnosis, treatment, adherence and control, iv) studies conducted on patient populations focusing exclusively on chronic pain (CLBP and OA), and neuropathic pain (DNP and LBP). Definitions for chronic pain and NP are provided in Appendices -2 & 3.
Studies/records without any information on chronic and NP, those with data not from the representative country, not describing patient journey, without nationally representative populations, non- English language studies, case studies, letters to the editor, editorials and studies including specific patient subgroups, duplicate records and without full-text and not according to inclusion criteria were excluded.
Study-selection
An independent reviewer conducted a semi-systematic literature search to extract data from both structured and unstructured search. The titles and abstracts of the retrieved publications were screened against the inclusion and exclusion criteria. A second independent reviewer assessed these search results based on study title, article citation, author names, year of publication, abstract, study design, study participants and study setting of the retrieved search publications and excluded the non-relevant publications. Any disagreements were reconciled by discussion among the reviewers. Where nationally representative populations from studies with a sample size of ≥500 were not available, data points from studies that included only a population subgroup, single-centre experience or had a sample size of <500 were considered eligible for inclusion. Furthermore, any identified data gaps were supplemented with publications in local languages and anecdotal data from local clinical experts.
Data extraction and evidence synthesis
The extracted data included epidemiology data, data on patient journey and challenges associated with patients’ and healthcare systems’ perspective. Combined data from the structured and unstructured searches as well as local publications was synthesised by weighted average or simple average to minimise the bias arising from the methodological limitations of different studies. After manual screening, relevant data from the included studies were exported to Microsoft Excel for data extraction and was verified by more than one reviewer to maintain consistency. The synthesised evidence was represented as an evidence gap map followed by synthesis data which were synthesised through weighted mean or simple mean.
Results
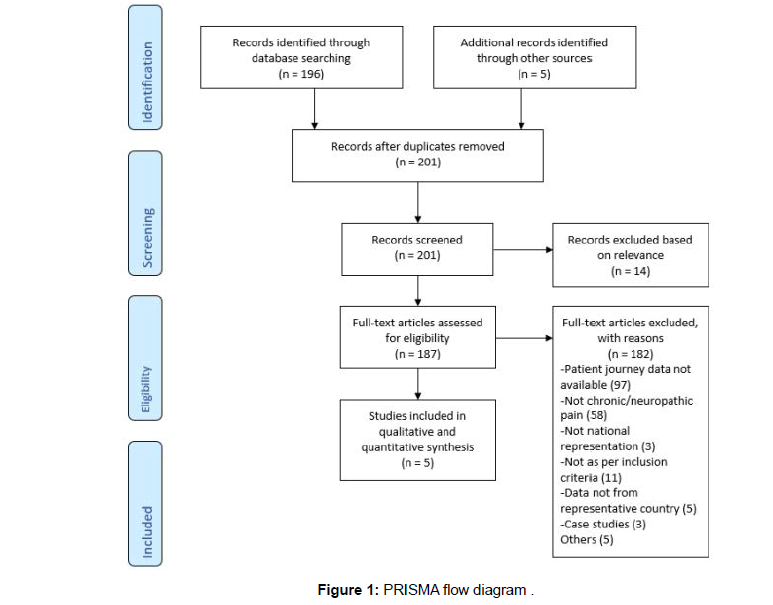
Of the 201 retrieved articles, 196 and 5 studies/records belonged from structured and unstructured search, respectively. Of the 201 studies/records, 14 studies/records were excluded based on relevance followed by 187 studies/records screened for eligibility (Figure 1). Finally, 5 studies/records were included for the main analysis.
Overview of included studies
Chronic pain
2 studies were included, one with patients with rheumatic diseases [15] and the other with psoriatic arthritis [16]. The outcomes of interest in any study did not exclusively focus on the prevalence of the patients with chronic pain. Supplemental data included 2 consensus guidelines [17] and a Spanish report on updates on OA [18], which also contained information on the prevalence of OA. Consensus guidelines were focused on chronic pain and its management. However, only 2 records – a treatment consensus report by Amescua-Gracia et al and a treatment consensus by Baptista et al were found useful. The former reported prevalence data on CLBP, whereas the latter contained information on patient journey touchpoints in CLBP. Detailed study characteristics can be found in Table 1.
| S. No. | Author(s) | Publication Type | Year | Sample Size | Prevalence (%) | Awareness (%) | Screening (%) | Diagnosis (%) | Treatment (%) | Adherence (%) | Control (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Chronic Pain | |||||||||||
| 1 | Garrott15 | Original Research Article | 2019 | 295 | OA: 1.4 | - | - | - | - | - | - |
| 2 | Martire16 | Original Research Article | 2019 | 83 | - | - | - | OA: 18 | - | - | - |
| 3 | Baptista17 | Treatment Consensus Report | 2019 | - | - | - | - | - | - | - | Chronic LBP: 20-50 |
| 4 | Rillo18 | Treatment Update | 2018 | - | OA: <10 | - | - | - | - | - | - |
| 5 | Amescua-Garcia C6 | Treatment Consensus Report | 2018 | 6992 | Chronic LBP: 11 | - | - | - | - | - | |
| 6 | KOL-based | Chronic LBP: 70 OA: 10 |
Chronic LBP: 50-75 OA: <30 |
Chronic LBP: 25-50 OA: 25-50 |
Chronic LBP: 25-50 OA: >75 |
Chronic LBP: 50 OA: >50 |
OA: 50 | ||||
| Neuropathic Pain | |||||||||||
| 7 | KOL-based | DPN: 1.4 LBP: 10 |
DPN: <25 LBP: <10 |
DPN: <25 LBP: <10 |
DPN: 37.5 LBP: 37.5 |
DPN: 37.5 LBP: 37.5 |
DPN: <25 LBP: 10-15 |
DPN: <25 LBP: 20 |
|||
Table 1: Characteristics of included studies.
Abbreviations: DPN: Diabetic Peripheral Neuropathy; LBP: Low Back Pain; OA: Osteoarthritis;
Neuropathic pain
No studies/records were found with any significant data on exclusively NP.
Inference from the pooled estimates
Chronic pain
According to the local experts, except high level of health literacy, awareness and screening regarding CLBP, diagnosis and treatment were received by only 37.5% of the total population. Also, of the limited number of patients that received treatment, only half proportion was found to be adherent to prescribed treatment regimens. Similarly, this declining trend was also observed in the disease control. However, reverse trend with lower awareness, screening and diagnosis with a higher number of patients receiving treatment was found in the case of OA. However, there was no change in the adherence or control in the OA patients.
Neuropathic pain
No noticeable proportion in any stage of the whole patient journey was observed for both DPN and LBP-NP.
Pooled estimates for both chronic pain and neuropathic pain are given in table 2.
| Indication | Population | Health literacy | Prevalence | Awareness | Screening | Diagnosis | Treatment | Adherence | Control |
|---|---|---|---|---|---|---|---|---|---|
| Chronic pain | |||||||||
| Chronic LBP | 44,781,000 | 62.5%ǂc | 11%a | 70%ǂc | 62.5%ǂc | 37.5%ǂc | 37.5%ǂc | 50%ǂc | 35%ǂc |
| OA | <25%ǂc | 5.7%*ǂa | 10%ǂc | <30%ǂc | 27.8%*ǂb | >75%ǂc | >50%ǂc | 50%ǂc | |
| Neuropathic pain | |||||||||
| DPN | 44,781,000 | <25%ǂc | 1.4%ǂc | <25%ǂc | <25%ǂc | 37.5%ǂc | 37.5%ǂc | <25%ǂc | <25%ǂc |
| LBP | <25%ǂc | 10%ǂc | <10%ǂc | <10%ǂc | 37.5%ǂc | 37.5%ǂc | 12.5%ǂc | 20%ǂc | |
Table 2: Pooled Estimates of Patient Journey Touch-points from Included Studies.
*Studies including population subgroups, single-centre studies or sample size <500.
ǂSimple average.
aPeer-reviewed publication; bScientific literature + expert opinion; cExpert opinion only.
Abbreviations: DPN – diabetic peripheral neuropathy; LBP – low back pain, OA - osteoarthritis
Health literacy source: Average of values realised from opinions.
Discussion
Our study provided the prevalence of CLBP and NP using a mix of publicly available literature data and expert opinions. According to the synthesized findings from the data available from treatment consensus by Amescua-Gracia and a congress abstract by Garrott and team, and a treatment update report by Rillo, the prevalence of CLBP and OA was 11% and 5.7%, respectively. This was consistent with the findings shown in a systematic review (10.5%) that explored pain prevalence in the Latin American region [19]. However, a study in Chile reported a slightly higher LBP prevalence of 22.1% [20]. While the prevalence of neuropathic pain and DPN were 10% and 1.4%. Also, there was a great difference between chronic low back pain-neuropathic pain (CLBPNeP) prevalence reported in our study by local experts (<25%) and the study abstract published from the Brazil region (36.5%). This could be justified by the under-recognition of symptoms of neuropathic pain in patients with CLBP. Noticeably, no published literature was available containing epidemiological data on neuropathic pain in our study, indicating a strong need for epidemiological research and publication in indexed and peer-reviewed journals. Secondly, a fragmented patient journey was observed in the study findings.
Our study focused on key patient journey touch-points: awareness, screening, diagnosis, treatment, adherence, and control. There was a huge difference observed in the pooled awareness regarding CLBP (70%) and that of NP(CLBP-NeP) (<25%). The reason behind such discrepancy could be explained by the inherent complexity of the NP. Differential diagnosis is more challenging among primary care providers, and what should be improved as a priority for better patient management. As a result, there is no specific awareness inculcated amongst the patient community about possible co-morbidities with NCDs like diabetes and its dreadful complications. This is also reflected in the poor screening for NP patients (<25%) unlike the case with CLBP patients (62.5%). This could be partially attributable to a non-exhaustive physical examination, under-recognition of verbal descriptors, and scarce use of screening tools for the diagnosis of neuropathic pain.
Surprisingly, despite the high proportion of screened CLBP patients, the diagnosed proportion was drastically lesser (37.5%). A similar trend was observed in the case of patients with NP. Such process gaps highlight the need for integrating advanced technologies for better patient screening and pain diagnosis in Argentina. Another challenge encountered especially in NP is that DPN – a typical manifestation of NP – is accompanied by painful symptoms in approximately 10% to 30% of patients [21]. Hence, it remains underdiagnosed, thereby compromising treatment decisions.
Patient journey mapping in the current study suggested a low awareness and sometimes difficult access to treatment facilities by patients with chronic and NP in Argentina. As seen in other countries, less than half of the patients with chronic and NP adhered to the prescribed treatment. With the spectrum of chronic pain, patients with OA have better access to treatment than those with LBP, which is reflected in better adherence and control. NP, on the other hand, had multiple challenges like lack of awareness, and possibly inadequate screening, diagnosis, and treatment, which could have also contributed to poor adherence.
General practitioners are familiar with patients with somatic or visceral pain, which is different from NP. Considering that the rate of NP is high, early identification and treatment initiation are vital [22]. As a result, despite the availability of medications for pain relief, additional agents are required because of the inadequacy of administered medications depending on several patients’ clinical conditions. Therefore, knowledge regarding various therapies for pain management is essential among pain specialists.
Another factor impacting the pharmacotherapy outcome is the so-called pharmaco-resistant pain in nearly 40% of patients with NP [23]. This could be suggestive of a low effect of present monotherapy. Additional medications place a significant economic burden on the patient. This has been reflected in the increased cases of opioid misuse and abuse, especially in the treatment of non-cancer chronic pain [24]. Owing to the financial constraints and less trained healthcare staff, the facilities for pain management including pain-specific clinics are insufficient for the population. While developed countries have established acute care teams and chronic pain clinics for effective pain control through patient education, evidence-based strategies, and research, these have not been fully adopted in Argentina [25].
From the technology perspective, newer treatment modalities like neuromodulation techniques (transcranial magnetic stimulation [TMS] and transcranial direct current stimulation [tDCS]) have been approved for both regional and national use, however, because of resource constraints and availability issues, they are less practiced. Several advanced treatments such as tDCS and repetitive TMS, which are also followed in Argentina, require longer time for every session (approximately 40 minutes and 1 hour, respectively), which limits the number of patients who can avail these facilities. Therefore, several machines are required to meet the high patient demand, which, in some cases, further increases the economic burden.
Strategies
Such process inconsistencies emerging from the know-do gap imply the need for robust capacity building and increasing community awareness. The Argentinian academy government has initiated several knowledge dissemination activities for increasing patient awareness about timely diagnosis and a rational approach towards self-medication. There still remains an unmet need to avoid incorrect treatment recommendations from healthcare practitioners as well. A survey reported that 53% of practitioners lacked college training for NP and 62% assessed themselves as being incompetently skilled for the same in Argentina [26]. A study of pain should include a holistic approach that not only limits pathophysiology but also psychosocial and economic aspects while aiming to improve the understanding of the pain mechanism and thereby the therapeutic landscape. This may improve the understanding of pain from the holistic care perspective. Unfortunately, currently, such an in-depth approach is not yet seen [27].
Capacity-building programs are a great option in this case which also nurture the physician-patient relationship while up-skilling the healthcare professionals. There is often a high patient load and busy schedules of treating physicians that hinders the detailed consultation with patients, thereby resulting in a transactional approach regardless of empathy. From an emotional perspective, patients could build resilience to withstand chronic pain provided that they are listened to and acknowledged by the clinicians. Failure to engage emotionally with the patient poses challenges to self-management of pain, especially when co-existing with depression and anxiety during flare-ups. Thus, it is imperative that such capacity-building oriented toward patientcentred care is promoted.
Another action area from the study of practice lacunae includes limited adoption of the latest pain management guidelines. Regular updates in currently available treatment guidelines and clear guidance about their contextual adaptations would be certainly a remarkable step toward pain care improvement.
Implications for practice and policy recommendations
Effective pain management in developing countries like Argentina relies on a multi-sectoral approach. In addition, promoting knowledge exchange among pain specialists and primary care physicians, as well as including refresher courses for pain management specialists can improve the practical knowledge of the practitioners [28]. Although there have been several knowledge dissemination events such as pain symposia and workshops as well as academic programs like postgraduate pain clinics, they need intensification to solve the trainingrelated issues [29]. Patients with acute or chronic pain should be systematically evaluated to identify the type of pain, with the possibility of ‘mixed pain’ in case of overlapping symptoms. This would help in the assessment of pain and provide targeted treatment [30]. Patient education programs should be targeted more at suburban areas, which usually comprise a population of low socioeconomic status. Furthermore, customizing these programs for more susceptible populations, such as adults, could increase their reach and impact.
Secondly, innovative patient monitoring and treatment approaches should be incorporated for chronic pain. These provide more realistic data for pain assessment, resulting in improved quality of care and reduced overall healthcare costs [31]. Such monitoring devices would help in both individual-level reporting and mass screening. In some cases, it must be taken into account that medications will have to be made available to all patients by providing subsidized or free-ofcost medications and maintaining the supply-demand chain, it can significantly improve treatment outcomes.
A well-defined treatment algorithm depending on the type of pain should be developed. This includes amitriptyline, gabapentin, and pregabalin as the first line of treatment for NP; duloxetine as the second line of treatment; tramadol, opioids, and topical drugs as the third line of treatment; and serotonin selective reuptake inhibitor antidepressants and other antiepileptic drugs as the fourth-line of treatment. In some circumstances, the first-line treatment could be modified to include, for example, tramadol and opioids for acute NP, carbamazepine, and oxcarbazepine for trigeminal neuralgia, and pregabalin and duloxetine for painful diabetic polyneuropathy. As studied by Duthy and Scholtn, the difference in adequacy consumption measures of Argentina, Canada, and the United States was 6%, 312%, and 229%, respectively [32]. This data highlights the fact that opioid abuse in Argentina is not a public health problem, and it is very rare.
This implies that the need is not to focus on the risk of opioid addiction, but rather on the high consumption of self-administrated non-steroidal anti-inflammatory drugs (NSAIDs) by patients. Also, very low prescription of opioids for both pain from with or without the side-effect of cancer is a matter of concern.
Cost-effective therapies such as non-pharmacological approaches with positive effects on sleep improvement, decrease in pain and reduction in fatigue should be advocated [33]. A combination of pharmacological and non-pharmacological treatments has shown improvements in patients suffering from pain due to fibromyalgia. Adopting these approaches could, therefore, improve patient outcome.
Study limitations
The study could not find supporting literature regarding epidemiological data on NP. Thus, it was not possible to validate the information shared by local experts. Also, due to the unclear definitions and intrinsic subjectivity, it was not possible to determine the proportion of patients who had achieved control from the pain perception. Moreover, there could lie the possibility of potential bias in the patient journey touch-point that estimates regarding chronic pain as they were from local experts, which may not match with peerreviewed evidence quality. Hence, cautious interpretation is warranted.
Conclusion
Chronic and NP management in Argentina has reflected gaps in the patient journey, thereby requiring immediate attention. Given the lack of robust epidemiological data and underreported prevalence of NP, there remains an emergent need for high quality evidence generation to inform the practice stakeholders. Also, the availability and training for advanced diagnostic technologies at primary care settings, up-to-date knowledge management through seamless access to latest clinical guidelines and practical guidance about the contextual adaptations of the guidelines would be the key drivers of quality pain care in Argentina.
Transparency section
Declaration of Funding
Funding for this study was provided by Upjohn – a division of Pfizer company.
Declaration of financial/other relationships
There is not conflict of interest with this paper content.
Authors’ contributions
Roberto Rey, Pierina Bachetti and Analia Procopio were involved in the conception of the review, analysis and interpretation of the data, drafting of the manuscript and revising it critically for intellectual content, and final approval of the version to be published. All the authors are accountable for all aspects of the work.
Acknowledgement
We acknowledge the experts who provided insights for bridging the data gaps. The support provided by the independent reviewer, Aditi Karmarkar from Upjohn – a Pfizer division, is deeply acknowledged. We also thank Kaveri Sidhu from Upjohn – a Pfizer division for critically reviewing the draft. Authors of this paper would like to acknowledge Kapil Khambholja and Indegene team’s support for medical writing and reviewing services for this manuscript which was funded by Upjohn – A legacy Pfizer division.
References
- https://www.iasp-pain.org/publications/iaspnews/?ItemNumber=8340
- Pierobon A, Policastro PO, Soliño S, Andreu M, Novoa G, et al (2020). Beliefs and attitudes about low back pain in Argentina: A cross-sectional survey using social media. Musculoskelet Sci Pract EU 49:1021-1083.
- Sheng J, Liu S, Wang Y, Cui R, Zhang X (2017) The Link between Depression and Chronic Pain: Neural Mechanisms in the Brain. Neural Plast UK 2017:1-10.
- Brennan F, Carr DB, Cousins M (2007) Pain management: a fundamental human right. Anesth Analg UK 105:205–221.
- Tang SP, Yeo ASH, Cardosa MS (2021) Paediatric pain management in low-income and middle-income countries. Lancet Child Adolesc Health EU 5:5–7.
- Amescua G C, Colimon F, Guerrero C, Jreige Iskandar A, Berenguel Cook M, et al (2018). Most Relevant Neuropathic Pain Treatment and Chronic Low Back Pain Management Guidelines: A Change Pain Latin America Advisory Panel Consensus. Pain Med 19:460–470.
- Rey R, Arizaga E, Verdugo R, Vidal O, Jreige A, et al (2011). Recommendations of the Latin-American network for the study and treatment of the neuropathic pain. Drugs Today Barc EU 47:1–33.
- Rey R (2013) Tratamiento del dolor neuropático. Revisión de las últimas guías y recomendaciones. Neurol Argent EU 5:1–7.
- Pierobon A, Villalba F, Ferreira G, Maher CG (2021) Insights into low back pain management in Argentina. Braz J Phys Ther USA 25:659-663.
- Soriano ER, Zingoni C, Lucco F, Catoggio LJ (2002)Consultations for work related low back pain in Argentina.J Rheumatol USA 29:1029-1033.
- Wenk R, Bertolino M, Pussetto J (2000) High opioid costs in Argentina: an availability barrier that can be overcome. J pain symptom manage EU 20:81-82.
- Manjiani D, Paul DB, Kunnumpurath S, Kaye AD, Vadivelu N, et al (2014). Availability and utilization of opioids for pain management: global issues. Ochsner J USA 14:208-215.
- Devi R, Kanitkar K, Narendhar R, Sehmi K, Subramaniam K (2020) A Narrative Review of the Patient Journey Through the Lens of Non-communicable Diseases in Low- and Middle-Income Countries. Adv Ther 37: 4808-4830.
- Bharatan T, Devi R, Huang P H, Javed A, Jeffers B, et al (2021). A Methodology for Mapping the Patient Journey for Noncommunicable Diseases in Low- and Middle-Income Countries. J Healthc Leadersh UK 13:35–46.
- Garrott LGF, Graff C, Recalde MFC, Lucero E, Capozzi N, et al (2019). Sexual activity perception in rheumatic diseases:Conference: 21st Pan American Rheumatology Congress, PANLAR 2019. Ecuador. J Clin Rheumatol 25:1-86.
- Martire MV, Girard Bosch MP, Scarafia S, Cosentino V, Tapia Moreira MJ, et al (2019). Spanish Validation of the GEPARD Questionnaire for the Detection of Psoriatic Arthritis in Argentinian Patients with Psoriasis. Dermatology EU 235:101-106.
- Baptista AF, Fernandes AMBL, Sá KN, Okano AH, Brunoni AR,et al (2019). Latin American and Caribbean consensus on noninvasive central nervous system neuromodulation for chronic pain management (LAC2-NIN-CP). Pain rep US 4:9-92.
- https://www.montpellier.com.ar/Uploads/Separatas/2018%20Osteoartritis.pdf
- Garcia JBS, Hernandez-Castro JJ, Nunez RG, Pazos MA, Aguirre JO, et al (2014). Prevalence of low back pain in Latin America: a systematic literature review. Pain Physician US 17:379–391.
- Bilbeny N, Miranda JP, Eberhard ME, Ahumada M, Méndez L, et al (2018). Survey of chronic pain in Chile – prevalence and treatment, impact on mood, daily activities and quality of life. Scand J Pain. De Gruyter EU 18:449–456.
- Onge EL, Miller SA (2008) Pain Associated with Diabetic Peripheral Neuropathy: a review of available treatments. Pharm Ther EU 33:166–176.
- https://issuu.com/fundacionmedife/docs/dolor-neuropatico-digital
- Lembke, A (2012) Why Doctors Prescribe Opioids to Known Opioid Abusers. N Engl J Med US 367:1580-1581.
- https://ebooks.iasp-pain.org/guide_to_pain_management_in_low_resource_settings
- Blanco GA, Braver JD, Buonanotte F, Ferrari F, Litvak LE, et al (2013). Encuesta sobre educación médica en dolor neuropático en Argentina. Neurol Argent EU 5:16–19.
- https://www.psicooncologia.org/articulos/Bases%20para%20el%20manejo%20del%20dolor.pdf
- Size M, Soyannwo OA, Justins DM (2007) Pain management in developing countries. Anaesthesia US 1:38–43.
- , http://www.sergiopasqualini.com.ar/imgs/merged.pdf
- Freynhagen R, Rey R, Argoff C (2020) When to consider ‘mixed pain’? The right questions can make a difference! Curr Med Res Opin UK 36:2037-2046.
- Rodríguez I, Herskovic V, Gerea C, Fuentes C, Rossel PO, et al (2017). Understanding Monitoring Technologies for Adults With Pain: Systematic Literature Review. J Med Internet Res EU 19:1-364.
- Duthey B, Scholten W (2014) Adequacy of opioid analgesic consumption at country, global, and regional levels in 2010, its relationship with development level, and changes compared with 2006. J Pain Symptom Manage EU 47:283–297.
- Perrot S, Russell IJ (2014) More ubiquitous effects from non-pharmacologic than from pharmacologic treatments for fibromyalgia syndrome: a meta-analysis examining six core symptoms. Eur J Pain Lond Engl EU 18:1067–1080.
- Marchesoni CL, Buonanotte F, Rey R (2013). Fibromialgia para neurólogos. Controversias sobre una consulta frecuente. Neurología Argentina EU 1:8-15.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar,Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar,Crossref
Indexed at, Google Scholar,Crossref
Indexed at, Google Scholar,Crossref
Indexed at, Google Scholar,Crossref
Indexed at, Google Scholar,Crossref
Indexed at, Google Scholar,Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Rey R, Bachetti P, Procopio A (2022) Management of ChronicandNeuropathic Pain in Argentina – Evidence, Gaps and Approach. J PainRelief 11:456. DOI: 10.4172/2167-0846.1000456
Copyright: © 2022 Rey R, et al. This is an open-access article distributedunderthe terms of the Creative Commons Attribution License, which permits unrestricteduse, distribution, and reproduction in any medium, provided the original authorandsource are credited
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4029
- [From(publication date): 0-2022 - Nov 16, 2025]
- Breakdown by view type
- HTML page views: 3417
- PDF downloads: 612