Research Article Open Access
Management and Optimisation of the Dose in Computed Tomography via a Dose Tracking Software
Vasileios Chatzoglou1,2, Sofia Kottou2, Dimitrios Nikolopoulos3*, Michael Molfetas4, Ioannis Papailiou1 and Virginia Tsapaki11Konstantopoulio General Hospital, Nea Ionia, Athens, Greece
2National and Kapodistrian University of Athens, Faculty of Medicine, Medical Physics Laboratory, Athens, Greece
3Piraeus University of Applied Sciences (TEI of Piraeus), Electronic Computer Systems Engineering, Athens, Greece
44Radiation Protection and Quality Assurance Office ├ó┬?┬?M Molfetas├ó┬?┬Ł, Athens, Greece
- *Corresponding Author:
- Dimitrios Nikolopoulos
Piraeus University of Applied Science
Electronic Computer Systems Engineering
Petrou Ralli and Thivon 250
GR-12244, Aigaleo, Greece
Tel: 0030-210-5381560
Fax: 0030-210-5381436
E-mail: dniko@teipir.gr
Received date: May 17, 2016; Accepted date: July 06, 2016; Published date: July 11, 2016
Citation: Chatzoglou V, Kottou S, Nikolopoulos D, Molfetas M, Papailiou I, et al. (2016) Management and Optimisation of the Dose in Computed Tomography via Dose Tracking Software. OMICS J Radiol 5:227. doi: 10.4172/2167-7964.1000227
Copyright: © 2016 Chatzoglou V, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Radiology
Abstract
Introduction: Computed Tomography (CT) produces high quality diagnostic images at the expense of increased radiation dose compared to routine radiographic examinations. The dose from the CT examinations can be reduced by controlling certain scanning parameters and optimising the employed practices. In this study a patient dosetracking software was utilised for the management of the CT doses and the optimisation of the scanning protocols. Material and Methods: DoseWatch from GE® Healthcare is a software for monitoring the radiation dose of patients undergoing CT examinations. It tracks simultaneously relevant technical and patient data. DoseWatch was used for the assessment of the scanning protocols of a Philips Brilliance 64 CT scanner during a period of three months in a large public general hospital of Athens in Greece. The dose dataset was compared with the CT Diagnostic Reference Levels (DRLs) available from the Greek Atomic Energy Commission (GAEC). Results and Conclusion: DoseWatch was deemed as a quick and effective tool for tracking and optimising the doses in CT examinations. It can be utilised as well for the improvement of the related scanning protocols. Through this suitable software, patients were identified with CT doses higher than the corresponding CT DRLs. The scanning parameters of the investigated cases were modified accordingly to achieve reduction of the corresponding CT doses.
Keywords
Computed tomography; Dose management; Dose tracking; Scanning protocol optimisation
Introduction
Computed tomography (CT) is widely used in radiology to obtain high quality diagnostic images, however, at the expense of high medical radiation exposure. The effective dose for the most typical CT examinations is between 1 mSv and 10 mSv [1], and it can be significantly increased, up to three times, in situations were more scans are required. Due to the high radiation doses, which are associated with CT examinations, it is necessary to track patient dose data and CT protocol scanning practices, and also to apply system's optimisation and dose reduction techniques. It is worth to note, that when organ specific cancer risk is adjusted for current levels of CT usage, it can be deduced that 1.5-2% of cancers may eventually be caused by the ionising radiation used in CT [2], although considerable debate exists regarding these assumptions. Note, that the effective dose of 10 mSv is associated with an increased risk of fatal cancer [3].
Up-to-date, the advancements in CT technology have focused on minimising the exposure of the patients undergoing CT examinations, while retaining the image quality at high standards. To attain this, and therefore maintain the balance between dose and image quality, a wide variety of image analysis software and image reconstruction algorithms have been developed along with special mechanical and electronic
components, that modify and improve the beam quality and irradiation procedure. Dose reduction in Computed Tomography examinations is achieved through the use of the automated mA and kV modulation technology, the iterative reconstruction algorithms and the optimisation of the scanning parameters [4-7]. An effective method for the reduction of the related CT doses has been reported to be the systematic monitoring of the radiological procedures and the doses calculated at the sites [8,9].
To reduce the radiation to patients from CT examinations and to facilitate the standardisation of CT dose levels, diagnostic reference levels (DRLs) for the most typical examinations have been recommended in many countries. The Greek Atomic Energy Commission (GAEC) is the responsible Greek Authority which established the corresponding limits on Greek territory. In general, the dose to the patients undergoing CT examinations is usually calculated through two indexes, viz., the CTDIvol (Computed Tomography Dose Index volume) and the DLP (Dose Length Product) values. The establishment of national DRLs in Greece has led to the modification of scanning protocols of many CT scanners in order to keep the CTDIvol and DLP indexes below the corresponding values specified by the established DRLs. Despite however that the GAEC's recommendations provide certain DRL values for the typical CT examinations and the normal sized patients, the meta-analysis of the CT examination data in Greece shows a wide variance between the different CT units. This can be attributed to (a) the variable hardware characteristics among several CT modalities; (b) the differentiations in the practices followed by technologists during operation; (c) the practical use of more than one protocols for some anatomical regions. The main feature included in the previous points that has a significant role in the observed variance is the Tube Current Modulation (TCM). TCM takes into account variations in x, y and z directions and adjusts accordingly the mAs to maintain a predefined image quality or noise level. The data from the scanogram/scout/surview option are used to properly apply this method, which is typically based on attenuation calculations derived from a CT planning radiograph. TCM is important when adjustment for patient size is needed. In fact, TCM adjusts the mAs value for cross section size and shape of the body under examination. This reduces the value of the mAs to be used to small patients but may increase it to large patients, a change that reduces or increases accordingly the CTDIvol and DLP values.
As mentioned before for the estimation of dose to patients from CT, the CTDIvol and DLP values are used. The CTDIvol represents the dose from a single slice and is based on measurements on acrylic phantoms. The DLP is irrelevant of the object scanned and is calculated by multiplying the CTDIvol with the scan length. In order to translate these parameters to dose weighting factors have been introduced to calculate effective doses.
In general, the standardisation and optimisation of the various utilised CT protocols in Greece with the prospect of achieving efficient reduction of the related CT doses, necessitates the analysis of the system's capabilities and the differentiations of the protocol's implementation together with the constant monitoring and evaluation of the followed practices. Until some years ago, the analysis and assessment of all these data were time consuming, complex and tedious tasks that required extensive statistics and long hours of analysis. This is more severe in large hospitals, where a considerable number of examinations are performed. The introduction, however, during the last years of the automated dose tracking softwares, enabled the convenient monitoring and recording of all the scanning information of every CT examination. In this consensus, this paper focused on the assessment of the utilised CT scanning protocols in Greece and the analysis of the CTDIvol and DLP values of several CT examinations in a modern CT scanner in Greece equipped with the patient dose tracking software DoseWatch of GE® Healthcare.
Methods
Data collection and auditing
A total of 2077 patients and 2451 CT examination scans were included in the study. The scans were obtained via 44 different scanning protocols in a Philips Brilliance 64 CT scanner. The scanner was installed in the Konstantopoulio General Hospital in Athens, Greece, which is one of the biggest hospitals of the capital area. The dose data (information of CTDIvol and DLP values, mAs etc. that are contained in the dose report) of all the included scans were tracked by the DoseWatch software connected on-line to the Philips CT scanner. It is significant to note that the 44 scanning protocols were dedicated to 16 different anatomical regions with the related parameters being adjusted according to the examination needs and the circumstances, e.g., contrast on or off, patient setting discrepancies during scans etc.
The DoseWatch software used in this study provided a very friendly user-interface that enabled the convenient discern of the examination dose data, as it offered the possibility of producing comparison diagrams between the calculated CTDIvol and DLP values with the mean values of all the tracked examinations of the same type. The software allowed also the user to monitor these values during preselected periods of time, a feature which can be very useful when trying to identify and track unexpected variations or to observe how they are affected by changes in the scanning protocols or scanning practices. It allowed as well, the determination of dose alarm levels so as to track any excess CTDIvol and DLP values easily and insert informative comments to the examination data where needed. Another characteristic was the ability to output the examination data to an ASCII file for further processing.
As can be audited, the whole set-up allowed the convenient and reliable collection and management of the dose data. The data were then used to assess the overall variations of the CTDIvol and DLP values and to credit the competence of the scanning protocols.
Specific CT dose tracking information
To calculate and compare CT doses to patients the CTDIvol and DLP values are needed. This data was collected from the software and its accuracy was verified by manual measurements. The phantom size used for the CT system CTDIvol value calculation for all scanning protocols was also determined with the measurements performed. The DRLs in Greece are reported for a 16 cm diameter phantom for the Head, Inner Ear and Sinus examinations and for a 32 cm diameter phantom for the Abdomen, Thorax and Lumbar Spine examinations. Therefore it was necessary to confirm that the units used for the analysis and comparison represented the same values.
Note, that in principle, a CTDIvol value provides an estimation of the absorbed dose received by the patient during a single axial slice (it is measured in mGy) while the DLP value gives an estimation of absorbed dose received by the patient during the whole scan (it is measured in mGy*cm). It has to be considered though that the CTDIvol and DLP values are calculated from measurements using 32 cm and 16 cm diameter cylindrical phantoms, which, on the one hand, simulate the body and head region adequately, on the other hand, they are not patient-specific. Therefore, at least in certain cases, the CTDIvol and DLP values may not represent the actual absorbed doses delivered but rather provide rough estimations of these. However, even in these cases, they could be useful since they can serve as a pathway to outline the exposure of the patient. Surely, the reduction of CTDIvol and DLP values renders the decrease of patient dose.
In order to keep the DLP at low levels, the scan range should be restrained to the anatomic region examined and the CTDIvol should have a low value. The main scanning protocol parameters that affect CTDIvol and are easy to change are: a) the X-ray tube current in mAs; b) the detector collimation; c) the Field of View (FOV). Since these parameters are of importance, they were recorded and analysed further to gain useful information for an efficient patient dose monitoring. Most of this information was retrieved by the dose reports that are automatically generated at the end of each examination. These dose reports recorded additionally the number of the acquisitions performed, the scan name and the data from the scanogram/scout/ surview and the bolus tracking (if used). Note that these reports represent the CTDIvol and DLP values per acquisition. All data in the dose reports were further processed so as to credit the competence of the scanning protocols, namely to evaluate the results.
.It should be mentioned here that the manual tracking of the CT dose data by recordings of the generated dose reports, can help the review of the CT examinations dose levels and may also reveal potential overexposures which need care for focused dose reduction techniques. However, this method is not practical since monitoring all the examinations can be difficult due to their large number. The data acquisition process can also lead to mistakes, usually by mistyping the information. Besides the above flaws, it can be very time consuming and thus require, dedicated personnel just for the data acquisition and categorisation. Furthermore, the data contained in the dose reports is limited. Hence, for an efficient dose optimisation process a lot of data should be collected. These difficulties can be overcome with the use of tracking software, which can automatically collect data from the CT examinations and present it in categorised structured data sheets ready to be reviewed and processed. This kind of software is very helpful since it can provide most of the data required fast and accurately.
Results and Discussion
The tracking of the CT dose data and the detection of the overexposures (surpassed CTDIvol or DRL values), were implemented via the available tools of DoseWatch software. The analysis of all the recorded data revealed however several inconsistencies. In specific, in those examinations where different patient body parts were irradiated, the CT system failed to differentiate them correctly. As a result, the system added the total DLP to a Head or Body scan, a fact which rendered noteworthy amount of data to be miss-grouped and, hence, to have to be manually corrected. Furthermore, in cases where the technologist started the examination with a certain protocol and then changed it for some reason, the examination was not grouped according to the final study, but classified according to the study used in opening. To overcome the inconsistencies, DoseWatch was properly adjusted so as to acquire only one practice per protocol. Through this adjustment, every examination was opened and implemented with the proper scanning protocol. In cases of multiple regions scanning, the system was also adjusted so as to acquire each scan with the appropriate protocol.
The analysis revealed transfer data gaps in some recordings with most important being the type of the examination. In this way, the examination purpose was difficult to pinpoint for a large proportion of the collected data. Nevertheless, since the study’s protocol name information was among the transferred data, and along with the information from the CT’s workstation, the examination data was reviewed and categorised properly, with non-significant losses due to the omitted information.
In this study data from single phase and multiphase examinations were recorded. However because the national DRLs refer to CTDIvol and DLP values per scan, every scan was analysed separately whether it belonged to single phase examination or a multiphase one.
The above facts were taken into consideration in the analysis of the statistical tendencies and the uncertainties of the final recorded data. To this end, the whole examination dataset was inspected in regard to the different types of body and sex of the patients. No particular statistical weight was identified for any of the body sizes or sex of the patients of this study, thus, it was considered that the examination scans were sampled from a hypothetical Gaussian distribution. Under this view, the mean value of the recorded CTDIvol and DLP distributions was used as the most adequate dose metric, at least for the typical patients. However, despite the above consideration, the standard deviation (SD) cannot be considered, respectively, as the corresponding adequate metric for the estimation of the total uncertainty, because the different scanning parameters and practices that were followed by the technologists imposed a significant bias to the examination data which could not be neglected. In particular, among many Brain scans, just a small change in mAs value occurred as the absorption in head did not change significantly among adults. Furthermore, in Sinus and Inner ear examinations, the mAs value was constant. In these cases, the discrepancy in the DLP values could be associated with the technologists’ practices and with how close the scanning region was kept to the region of interest. In the CT scans of the body region as well, the deviations of the CTDIvol values could be attributed only to the variation of patient size. In these cases, the corresponding uncertainty of the DLP values would be further increased due to the larger patients’ increased length. To account for the above sources of uncertainty, the partial data per examination was plotted versus the patient identification number, and a proper uncertainty value band was selected in a manner to include all errors of a typical-average patient size.
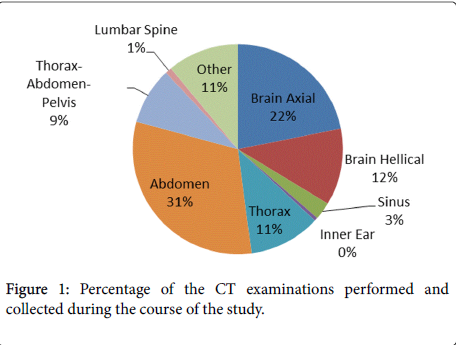
As mentioned before the 44 different scanning protocols studied here were used for 16 different anatomical regions. Because in Greece DRLs exist for the Brain, Sinus, Inner Ear, Thorax, Abdomen, Thorax- Abdomen-Pelvis and Lumbar Spine examinations, only the scanning protocols regarding these examinations were analysed. The national DRLs refer to adult typical patients and they were derived from the information obtained by GAEC from the 25% of total CT scanners in Greece. The appropriate protocols were divided in 8 groups (7 anatomical regions) so as to be able to compare the CTDIvol and DLP values taken from examinations with those proposed by GAEC. The examinations for these 7 anatomical regions constituted the 89% of the scans performed during the course of this study (Figure 1).
The national DRL values were identified as the reference limits for CTDIvol and DLP values of this study. This was because they are the standard for a CT scanner to operate with license and as a first step this was the minimum point wanted to be reached. Table 1 presents these eight groups and contains the Mean, Minimum and Maximum CTDIvol and DLP values from the sample along with the Greek DRLs values.
| Index | Type of value | Anatomical Region | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Brain | Sinus | Inner Ear | Abdomen | Thorax | Thorax-Abdomen-Pelvis | Lumbar Spine | |||
| Axial | Helical | ||||||||
| CTDIvol (mGy) | National DRL | 67 | 67 | 50 | 63 | 16 | 14 | 17 | 35 |
| Mean | 70.3 | 45.2 | 23.2 | 22.6 | 14 | 11 | 14 | 15 | |
| Minimum | 66.5 | 45 | No Value | No Value | 4 | 4 | 5 | 6 | |
| Maximum | 71.3 | 45.2 | No Value | No Value | 34 | 52 | 35 | 36 | |
| DLP (mGy*cm) x10 |
National DRL | 105.5 | 105.5 | 60.5 | 35.5 | 76 | 48 | 102 | 72.5 |
| Mean | 105 | 100 | 42 | 19 | 60 | 38 | 62 | 41 | |
| Minimum | 71 | 50 | 33 | 14 | 12 | 6 | 16 | 20 | |
| Maximum | 160 | 127 | 53 | 32 | 201 | 80 | 247 | 154 | |
Table 1: National DRLs, Mean, Minimum and Maximum CTDIvol and DLP for all the investigated anatomical regions. The brain region contains both axial and helical scans.
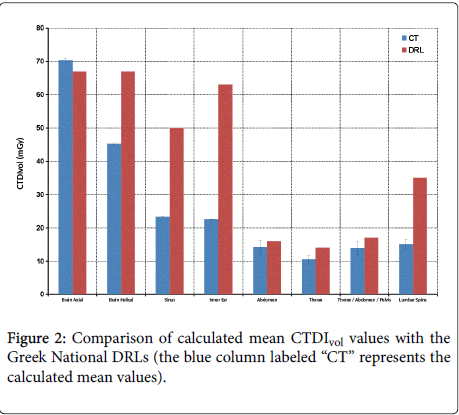
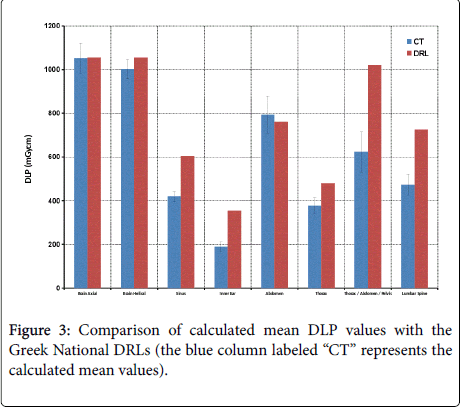
From Table 1 and the graphic presentation of the CTDIvol and DLP values per scanning region, it is clearly observed that the DRL values were surpassed during brain examinations using the axial protocol as far as CTDIvol is concerned (Figure 2) and the abdomen examinations as far as DLP is concerned (Figure 3). The Brain Axial and Brain Helical protocols were not grouped together because the calculated mean CTDIvol would be a biased result, giving falsely a value within the accepted limits.
As was observed from the whole dataset, the Brain CT examinations were implemented by two different scanning protocols, one utilising only axial slices and the other using helical CT only for special cases. Both scanning protocols used TCM but due to the structure of the head the mA value showed minor variations during the examination, thus, not changing significantly the exposure between patients. The average CTDIvol was 45.1 mGy for the Helical Brain CT and 70.3 mGy for the Axial Brain CT. Note that the corresponding national DRL value is 67 mGy. The DLP values for the Helical and Axial Brain CT were 1003 and 1052 mGy*cm respectively. The national DRL value for these cases is 1055 mGy*cm. Although the CTDIvol of the Helical brain CT scanning protocol was found to be lower than the corresponding Axial, the orientation of the slices was different and required extra scan length. The latter led to similar exposures for both practices. Regarding the CTDIvol of the Axial Brain protocol, the high number of mAs used was due to bad protocol creation were the DRLs value were not considered and had no clinical or diagnostic purpose.
The examinations of sinus and inner ear showed that the CTDIvol and DLP were kept steadily at low levels in comparison with the DRLs. In addition, if the mA value was not changed (TCM is not used), there was no fluctuation in the CTDIvol value. On the other hand, the DLP value depended on the scan length, therefore it was not constant. Regarding the body region, the mA value in all cases changed greatly due to the large variance of the weight and size of the patients. The CTDIvol and DLP values reached twice the DRL value in certain cases. This can be attributed to the volumetric data of the patients, namely for large patients the mA value has to be increased in order to keep the noise in predefined levels retaining image quality as needed. These cases were not classified as overexposures because the corresponding DRL values were for the typical weights and sizes. However, during these examinations the dose alert signal was ‘ON’ since the system does not take into account patient size.
A number of acquisitions with small DLP values were also observed indicating unfinished exposures. Investigation of these cases led to the conclusion that these were not due to user mistake or machine error, but rather due to the patient's discomfort which caused the interruption of the acquisition process.
From the findings of the collected data with DoseWatch, it was decided that for the brain CT examinations a larger noise threshold has to be kept and, therefore, the protocol was modified so as the TCM to choose lower mA values. The CTDIvol recorded after this change was below the levels of the national DRLs without any significant loss in image quality.
The dose data for the body region showed a great variance. As the height and weight data of each patient were not among the transferred data, it was decided to also track manually patient data for larger patients separately in order to investigate if the reduction of doses exceeding the DRLs could be made possible. Also the technologists were informed about the recommendation of DoseWatch software to have one practice per protocol so as the inconsistencies in the data categorisation to be reduced. However, in occasions where certain findings during the scan required more acquisitions to be made and this practice was not easy to be followed, it became a practice to report this to the medical physicist in order to review the situation properly.
Conclusion
DoseWatch was used for CT examinations scanning protocol optimisation and dose tracking. It enabled a fast collection of the data. Because of some incompatibility issues the data transfer to DoseWatch was slightly incomplete and therefore some parameters could not be monitored. Moreover examination categorisation was inconsistent due to the differences of the DoseWatch recommended protocol structure and the CT site protocol structure, a problem that maybe could be alleviated with the use of a RIS system [10]. Otherwise before installation of the program, the scanning protocols should be developed and modified with the one practice per protocol recommendation of DoseWatch so as to fully exploit its capabilities.
Manual process of the data fixed the inconsistencies and allowed the scanning protocol reviewing. Analysis of the data revealed examination types and cases where the CTDIvol and DLP values exceeded the national DRLs. The occurrences indicating overexposure were easily detected by the DoseWatch feature to set dose alert levels.
The data also showed that outdated protocols had been mistakenly used.
The actions taken after the data analysis were a) the 7 old protocols erased, b) the axial Brain scanning protocol modified so as to keep a higher noise threshold and lower the maximum mAs value available to this protocol and c) the continuing of dose data tracking for ‘large” patients for the body region examinations in order to specify a different noise threshold depending on the patient’s BMI and d) the collaboration with the department radiologists and technologists in order to change all the protocols and practices towards dose reduction.
Although the problems encountered in the data collection and categorization, the use of DoseWatch for dose data tracking allowed a fast reviewing of the examinations exposures and quick actions to be taken to reduce patient dose. As the familiarity increases decisions about examination doses and practices can be reached faster. It allows also to see the different practices followed by the users and make recommendations where needed. Moreover the ability to obtain large amounts of data fast and easily and to be able to provide a wellstructured statistical presentation of them can enable further and deeper investigation of the CT scanning protocols, which is also reported by other users [11-14]. To conclude the DoseWatch dose tracking software can help in the optimisation of CT dose and examination practices through a dose tracking and auditing procedure performed in any department.
References
- Brenner DJ, Doll R, Goodhead DT, Hall EJ, Land CE, et al. (2003) Cancer risks attributable to low doses of ionizing radiation: assessing what we really know. ProcNatlAcadSci U S A 100:13761-13766.
- Brenner DJ, Hall EJ (2007) Computed tomography-an increasing source of radiation exposure. N Engl J Med 357: 2277-2284.
- Annals of the ICRP (2007) ICRP 2007 International Commission on Radiation Protection The 2007 Recommendations of the International Commission on Radiological Protection.
- Campbell J, Kalra MK, Rizzo S, Maher MM, Shepard JA (2005) Scanning beyond anatomic limits of the thorax in chest CT: Findings, radiation dose, and automatic tube current modulation. Am J Roentgenol 185:1525-1530.
- Kalra MK, Woisetschläger M, Dahlström N, Singh S, Digumarthy S, et al. (2013) Sinogram-affirmed iterative reconstruction of low-dose chest CT: Effect on image quality and radiation dose. Am J Roentgenol 201: W235-W244.
- Lee CH, Goo JM, Ye HJ, Ye SJ, Park CM, et al. (2008) Radiation dose modulation techniques in the multidetector CT era: From basics to practice. Radiographics 28: 1451-1459.
- Tamm EP, Rong XJ, Cody DD, Ernst RD, Fitzgerald NE, et al. (2011) Quality initiatives: CT radiation dose reduction: How to implement change without sacrificing diagnostic quality. Radiographics 31: 1823-1832.
- Seuri R, Rehani MM, Kortesniemi M. (2013) How tracking radiologic procedures and dose helps: Experience from Finland. Am J Roentgenol200: 771-775.
- Duong PA, Little BP (2004) Dose Tracking and Dose Auditing in a Comprehensive Computed Tomography Dose-Reduction Program. Semin Ultrasound CT MRI 35: 322-330.
- Nicol RM, Wayte SC, Bridges AJ, Koller CJ (2015) Experiences of using a commercial dose management system (GE DoseWatch) for CT examinations. Br J Radiol 5: 20150617.
- Hadid L, Waryn MJ, Brillet PY, Sellier N (2013) Impact of a dose-tracking software and iterative reconstruction technique on the optimisation of CT protocols. Application to the radiology department of the hospital group â┬?┬?Avicenne, Jean-Verdier, René Muretâ┬?┬Ł. PhysicaMedica 29: e15.
- Bouëtté A, Dubus L, Menu Y (2012) The impact of a patient oriented automatic dose tracking system on the management and optimisation of a CT unit.
- Wang J, Molvin L, Marsh D, Zorich C, Chan F, et al. (2014) A Management Tool for CT Dose Monitoring, Analysis, and Protocol Review. Med Phys 41: 558.
- Heinrich M, Allgayer B, TreumannaTh, Pasquinia G, Buschmannb U, et al. (201 4) Dose reduction in computed tomography (CT) by the integration of a dose monitoring system. Swiss Medical Informatics.
Relevant Topics
- Abdominal Radiology
- AI in Radiology
- Breast Imaging
- Cardiovascular Radiology
- Chest Radiology
- Clinical Radiology
- CT Imaging
- Diagnostic Radiology
- Emergency Radiology
- Fluoroscopy Radiology
- General Radiology
- Genitourinary Radiology
- Interventional Radiology Techniques
- Mammography
- Minimal Invasive surgery
- Musculoskeletal Radiology
- Neuroradiology
- Neuroradiology Advances
- Oral and Maxillofacial Radiology
- Radiography
- Radiology Imaging
- Surgical Radiology
- Tele Radiology
- Therapeutic Radiology
Recommended Journals
Article Tools
Article Usage
- Total views: 12210
- [From(publication date):
August-2016 - Mar 29, 2025] - Breakdown by view type
- HTML page views : 11219
- PDF downloads : 991