Case Report Open Access
Malignant Gastric Outlet Obstruction
Salih Samo*
Feinberg School of Medicine, Northwestern University, Chicago, USA
- *Corresponding Author:
- Salih Samo
Feinberg School of Medicine, Northwestern University
333 East Ontario Street, Unit 4205, Chicago, IL 60611, USA
Tel: +1 312-503-8194
E-mail: salihsamo@hotmail.com
Received date: March 21, 2016; Accepted date: June 2, 2016; Published date: June 9, 2016
Citation: Samo S (2016) Malignant Gastric Outlet Obstruction. J Gastrointest Dig Syst 6:436. doi:10.4172/2161-069X.1000436
Copyright: © 2016 Samo S. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
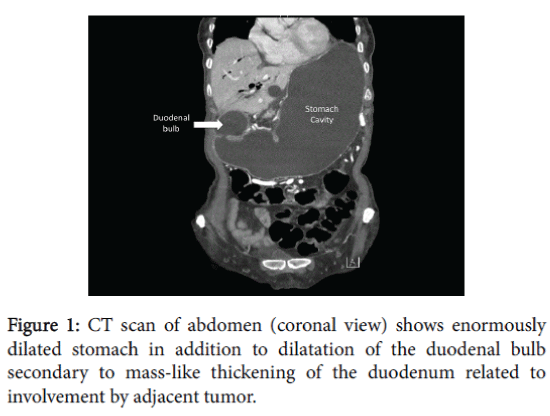
Currently, malignancy is the most common cause of gastric outlet obstruction (GOO) accounting for 50-80% of the cases. Additionally, GOO occurs in 15-25% of patients with pancreatic cancer. This case report is an interesting image of an enormously dilated stomach in a pancreatic cancer patient due to duodenal obstruction secondary to pancreatic cancer.
Keywords
Gastric outlet obstruction; Pancreatic cancer; Malignant
Case Information
A 73-year-old female with metastatic pancreatic adenocarcinoma with biliary stent placement, presented with bilious emesis and fever for one day but without abdominal pain. She had abdominal distention, sluggish bowel sounds and mild epigastric tenderness. Computed tomography (CT) scan showed dilatation of the esophagus, stomach (enormous) and down to the third portion of the duodenum secondary to mass-like thickening of the duodenum related to involvement by adjacent tumor (Figure 1). A nasogastric tube placement yielded 3.5 liters output immediately and drained more than 5 liters within 24 hours. While deploying a duodenal stent, the patient became bradycardic and later asystolic and chest compressions were started. As the abdomen was tense and tympanitic, needle decompression with an angiocatheter revealed air escape and return of spontaneous circulation.
Subsequent CT scan demonstrated a large proximal gastric body perforation. Initial management included intravenous fluid resuscitation, broad-spectrum antibiotics, and mechanical ventilatory support. Laparotomy revealed three tears on the anterior stomach surface (the largest tear measuring 8 cm) and were all repaired. After her discharge, the patient was started on FOLFOX6 chemotherapy regimen. However, due to her poor prognosis and performance status she was enrolled in hospice and expired six months after her presentation.
Discussion
Gastric outlet obstruction (GOO) is a misnomer expression as numerous cases include duodenal or extralunimal disease, rather than an isolated gastric disease. At current time, malignancy is responsible for 50-80% of the cases [1-3]. GOO occurs in 15-25% of patients with pancreatic cancer [4]. Other infrequent etiologies of malignant GOO include gastric lymphoma, gastric carcinoid [5], duodenal and ampullary neoplasms, and cholangiocarcinoma (local or advanced) [6].
Gastrojejunostomy has been the traditional treatment of choice to palliate malignant gastric and duodenal obstruction but with high morbidity and mortality rates [7]. Malignant GOO is the principal indication for gastroduodenal stenting to restore the luminal patency. In a systematic review and meta-analysis of randomized and nonrandomized trials, duodenal endoscopic stenting seemed to be safe and showed better short-term outcomes as compared to operative surgical gastrojejunostomy and therefore should be the preferred method in patients with short-life expectancy [8]. However, gastrojejunostomy have better long-term outcomes (fewer late complications and long patency) and should perhaps be preferred in patients with long prognosis [9].
References
- Johnson CD (1995) Gastric outlet obstruction malignant until proved otherwise. Am J Gastroenterol 90:1740.
- Shone DN, Nikoomanesh P, Sm ith-Meek MM, Bender JS (1995) Malignancy is the most common cause of gastric outlet obstruction in the era of H2 blockers. Am J Gastroenterol 90: 1769-1770.
- Johnson CD, Ellis H (1990) Gastric outlet obstruction now predicts malignancy. Br J Surg 77:1023-1024.
- Tendler DA (2002) Malignant gastric outlet obstruction: bridging another divide. Am J Gastroenterol 97: 4-6.
- Green ST, Drury JK, McCallion J, Erwin L (1987) Carcinoid tumour presenting as recurrent gastric outlet obstruction: a case of long-term survival. Scott Med J 32:54-55.
- Singh B, Kapoor VK, Sikora SS, Kalawat TC, Das BK, et al. (1998) Malignant gastroparesis and outlet obstruction in carcinoma gall bladder. Trop Gastroenterol 19:37-39.
- Dabizzi E, Arcidiacono PG (2016) Update on Enteral Stents. Current treatment options in gastroenterology.
- Nagaraja V, Eslick GD, Cox MR (2014) Endoscopic stenting versus operative gastrojejunostomy for malignant gastric outlet obstruction-a systematic review and meta-analysis of randomized and non-randomized trials. J GastrointestOncol 5:92-98.
- Miyazaki Y, Takiguchi S, Takahashi T, Kurokawa Y, Makino T, et al. (2016) Treatment of gastric outlet obstruction that results from unresectable gastric cancer: Current evidence. World journal of gastrointestinal endoscopy 8:165-172.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 13086
- [From(publication date):
June-2016 - Apr 04, 2025] - Breakdown by view type
- HTML page views : 12173
- PDF downloads : 913