Research Article Open Access
Magnetic Resonance Spectroscopy in Major Depressive Disorder
Mona Adel Mohamed1* MD, PhD, MPH, Ali Sibtain Farooq Sheikh2 MBBS, MD
1Assistant Professor of Radiology, Johns Hopkins University, Maryland, USA
2King Edward Medical University, Nila Gumbad, Anarkali, Lahore, Pakistan
Visit for more related articles at International Journal of Emergency Mental Health and Human Resilience
Abstract
In this paper, we have collected and discussed the current literature on MRS/MRSI techniques used in cases of depression to help understand the pathophysiology of the disease. The literature search using National Institutes of Health’s PubMed database, Scopus, and Google Scholar, provided us with 71 peer-reviewed publications to look at the disease effects amongst adolescent children, adult as well as the elderly population. Metabolite changes in N-acetyl aspartate (NAA), choline (Cho), glutamate (Glu), and Gamma Aminobutyric Acid (GABA) are quite consistent in some brain regions among comparable studies, with a few inconsistencies noted due to the different study designs.
Keywords
Brain Metabolites, MRS, depression
Abbreviations
MDD = major depressive disorder, rMDD = recovered major depressive disorder, HC = healthy control, ADHD = attention deficit hyperactivity disorder, OCD = obsessive compulsive disorder, ODD = oppositional defiant disorder, MRSI = magnetic resonance spectroscopic imaging, MRS = magnetic resonance spectroscopy , H-MRS = proton magnetic resonance spectroscopy, 31P MRS=P-31 magnetic resonance spectroscopy, MRI = magnetic resonance imaging, PET = positron emission tomography, SPECT = single photon emission computed tomography, TE = echo time, TR = repetition time, HPC = hippocampus, Amg = amygdala, AC = anterior cingulate, ACC = anterior cingulate cortex, pgACC = pre-genual anterior cingulate cortex, BG = basal ganglia, PFC = prefrontal cortex, DLPFC = dorsolateral prefrontal cortex, VMPFC = ventromedial prefrontal cortex, DMPFC = dorsomedial prefrontal cortex, OFC = orbitofrontal cortex, OC = occipital cortex, POC = parieto-occipital cortex, AI = anterior insula, WM = white matter, PWM = parietal white matter, GM = gray matter, CC = corpus callosum, AC = anterior commissure, PC = posterior commissure, B/L = bilateral, Glu = glutamate, Gln = glutamine, Glx = glutamate + glutamine, Gluc = glucose, GABA= γ amino-butyric acid, NAA= N-acetyl aspartate, mI= myoinositol, Cho= choline, PCh = phosphocholine, GPC = glycerophosphocholine, tCho = total choline, Cr= creatine, PCr = phosphocreatine, PE = phosphoethanolamine, TRP = tryptophan, KYN = kynurenine, 3-HAA = 3-hydroxyanthranilic acid, PME = phosphomonoester, PDE = phosphodiester, Pi = inorganic phosphate, ATP = adenosine triphosphate, NTP = nucleoside triphosphate, Tx = Treatment, Tr = treatment-resistant, CBT = cognitive behavioral therapy, ECT = electroconvulsive therapy, SSRI = selective serotonin reuptake inhibitor, TCA = tricyclic antidepressant, TSD = Total sleep deprivation, A = Adult, E = Elderly, P = pediatric, M = men, W = women, HAMA = hamilton anxiety scale, HDRS = Hamilton depression rating scale, CGI-S = clinical global impression-severity scale, BDI = beck depression inventory, CDRS-R = children’s depression rating scale-revised, MADRS = Montgomery-Asberg depression rating scale, BOLD = blood oxygenation level-dependent signal changes, NA = not mentioned, DSM = diagnostic and statistical manual of mental disorders, CSI=Chemical shift imaging, GAD = Generalized Anxiety Disorder, LCM= LC model software.
Introduction
Major Depressive Disorder (MDD)
Major depressive disorder poses a major health issue, often presented to and treated by the primary care physician (Shim et al., 2011). According to the world health report 2008, depression continues to be a significant cause of morbidity and mortality worldwide (www.who.int, 2012). Besides being a risk factor of medical illnesses, depression is a disabling disease, causing significant disability, poor quality of life, bad work performance, unstable relationships, and may lead to suicide (Stewart et al., 2003; Bernal et al., 2007). Major depressive disorder (MDD) is common, having one estimate a prevalence of 16.6%, affecting twice as many women as men (Weissman & Olfson, 1995; Kessler et al., 2005; Soleimani et al., 2011) and showing a frequent onset in childhood (Lewinsohn et al., 1986; Lewinsohn et al., 1993; Kessler et al., 1994). It has also been proven that pediatric MDD is in continuum with adult MDD (Lewinsohn et al., 2000). Furthermore, MDD is more common among patients with a medical illness (including cardiovascular disease, diabetes, stroke, HIV and other conditions) and is suggested to increase mortality by up to 4.3 times (Soleimani et al., 2011; Bruce & Leaf, 1989). An association between depression and the risk of cardiovascular disease (Agatisa et al., 2005; Alboni et al., 2008; Fan et al., 2008) as well as diabetes (Grandy et al., 2008) has been demonstrated.
In spite of the concerted efforts of health care workers, depressive symptoms continue to occur at a significantly high rate (Shim et al., 2011). For achieving a better remission rate (Tadic et al., 2011), researchers are constantly working to help diagnose and manage depression more effectively (Shim et al., 2011). Neuroimaging with monitoring of brain metabolites could be a potential tool for understanding the pathophysiology of depression, evaluating treatment response and predicting outcome of MDD patients.
Structural Neuroimaging
Brain areas involved in emotional regulation, including hippocampus (HPC), amygdala (Amg), anterior cingulate cortex (ACC), basal ganglia (BG), as well as prefrontal cortex (PFC) have been studied using magnetic resonance imaging (MRI) and shown to have structural alterations in MDD (Campbell et al., 2004).
The HPC volume was shown to be significantly reduced (Campbell et al., 2004; Videbech & Ravnkilde, 2004; McKinnon et al., 2009; Amico et al., 2011). Frontal and temporal lobes were shrunken with an increase in severity of depression , coinciding with the decline in cognitive performance (Elderkin-Thompson et al., 2003); however, the structural changes noted in the corpus callosum, thalamus and the BG were not consistent (Caetano et al., 2001; Brambilla et al., 2002a; Brambilla et al., 2002b; Lacerda et al., 2003; Brambilla et al., 2004; Lacerda et al., 2005).
Functional Neuroimaging
Functional studies, such as Positron Emission Tomography (PET) and Single Photon Emission Computed Tomography (SPECT), when combined with MRI, can provide an additional value in addressing this serious illness by localizing abnormalities in blood flow, metabolism and neurotransmitter receptors (Amico et al., 2011). The frontal brain regions (ACC, dorsolateral PFC (DLPFC), orbitofrontal cortex (OFC), and medial PFC) demonstrated hypoarousal (Bench et al., 1992; Dolan et al., 1994; Bremmer et al., 1997; Vollmert et al., 2004), whereas the limbic system (Amg, HPC and BG) showed hyperarousal in MDD patients (Ho et al., 1996; Mayberg et al., 1999). The frontal lobe blood flow and metabolism has been most consistently (but not specifically) shown to be affected in patients with depression (Hurwitz et al., 1990; Lesser et al., 1994; Mozley et al., 1996). When combined with magnetic resonance spectroscopy (MRS), functional MRI (fMRI) can provide better understanding of the relation of brain activation and brain chemistry. Blood oxygenation level-dependent signal changes (BOLD), provoked by emotional stimulus, have been studied in the pregenual anterior cingulate cortex (pgACC) of MDD patients, where negative responses correlated with glutamate (Glu) and N-Acetyl Aspartate (NAA); however in healthy controls negative responses of BOLD correlated with Gamma Aminobutyric Acid (GABA) as measured by MRS (Walter et al., 2009).
Magnetic Resonance Spectroscopy (MRS) and Spectroscopic Imaging (MRSI)
Although MRI is a valuable resource for detecting specific brain abnormalities in MDD patients, the neurochemical profiles are not completely studied (Urenjak et al., 1993). MRS can measure brain metabolites and in turn can help understand the metabolic profile in patients with MDD (Chang et al., 2003). Concentrations of metabolites act as tools which can aid in the diagnosis and the preparation of future diagnostic and statistical manual of mental disorders (DSM) (Regier et al., 2009). It can also help relate these metabolites with disease severity especially when it is linked with other functional connectivity imaging techniques (Horn et al., 2010).
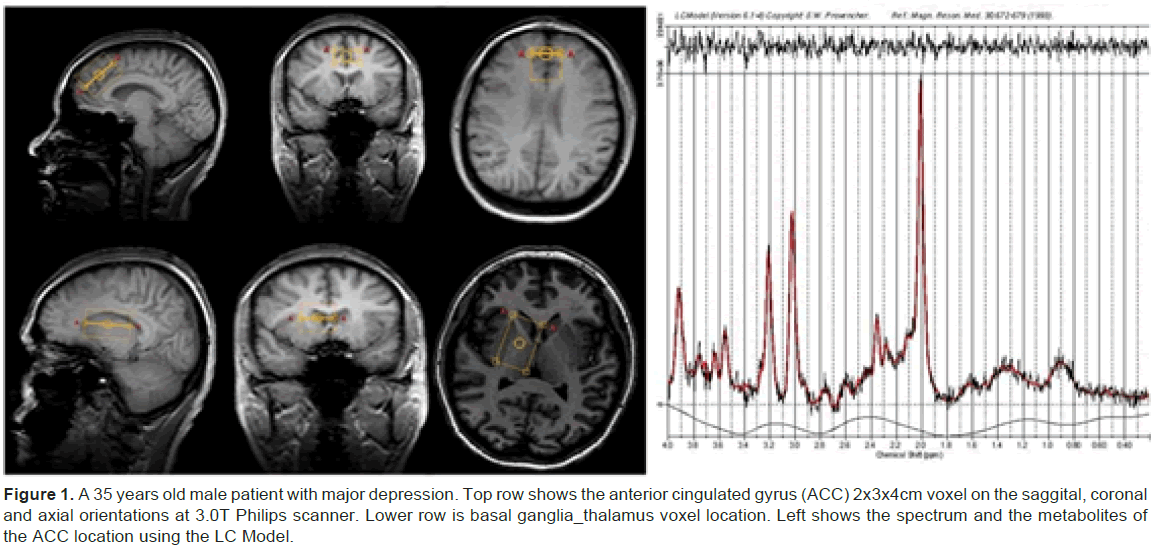
One major advantage of MRS is that it is a non-invasive, safe imaging technique (Stanley et al., 2000; Stanley, 2002; Kondo et al., 2011a). The chemical concentration of different molecules can be measured in living tissues with accuracy and precision (Figure 1). Short scan time with as little as less than 10 minutes and up to a maximum of 30 minutes allows the procedure to be performed in the clinical setting making it feasible and tolerable to the patient (Stanley et al., 2000). MRS is free from radiation hazards (Stanley et al., 2000; Kumar et al., 2002), allowing multiple tests, for taking measurements before and after therapy to check treatment response (Stanley et al., 2000).
Figure 1: A 35 years old male patient with major depression. Top row shows the anterior cingulated gyrus (ACC) 2x3x4cm voxel on the saggital, coronal and axial orientations at 3.0T Philips scanner. Lower row is basal ganglia_thalamus voxel location. Left shows the spectrum and the metabolites of the ACC location using the LC Model.
We found several MRS and magnetic resonance spectroscopic imaging (MRSI) studies that were conducted on depressive patients since 1992 to date (Tables 1 and 2). Most of these studies have utilized a 1.5 T magnetic strength scanner, but recent studies used 3.0 T and higher. Among the brain metabolites that have been studied, the most commonly reported ones in MDD patients include NAA, choline (Cho), creatine (Cr), Glx, and GABA. In our collection, 25 articles evaluated the effect of treatment on metabolite findings in MDD (Table 2). For instance, antidepressant and electroconvulsive therapy (ECT) had shown significant metabolic changes through MRS and MRSI studies in treatment responders (Charles et al., 1994; Sonawalla et al., 1999; Ende et al., 2000; Sanacora et al., 2002; Michael et al., 2003a, Michael et al., 2003b; Pfleiderer et al., 2003; Sanacora et al., 2003; Bhagwagar et al., 2004; Gonul et al., 2006; Ajilore et al., 2007; Merkl, et al., 2010).
| Authors | Nucleus/ Voxel placement | Subjects | Magnet strength/TR(sec)/TE (msec)/ voxel size | Meta-bolites | Findings |
|---|---|---|---|---|---|
| Kato et al.1992 | 31P MRS -Frontal cortex |
-10 Bipolar -12 MDD -22 HC |
1.5T/3.0/NA/NA | -PME -Pi -PDE -PCr -ATP |
Frontal Cortex -PME was higher in bipolars in the depressive state than HC. -PCr was significantly decreased in severely depressed patients compared to mildly depressed ones. |
| Moore et al.1997 | 31P MRS -BG |
-35 MDD -18 HC |
1.5T/3.0/NA/45cm3 | -PME -Pi -PDE -PCr -NTP |
BG -ATP is lower in the BG of depressed patients than HC. |
| Hamakawa et al.1998 | 1H-MRS Single voxel -BG |
-18 Bipolar -22 MDD -20 HC |
1.5T/2.0/135/27cm3 | -Cho | BG -Cho concentration was significantly higher in bipolar patients in the depressive state than HC. -Cho/Cr+PCr and Cho/NAA ratios were significantly higher in bipolar patients in both depressive and euthymic states as compared to HC. -Cho/NAA was significantly higher in MDD patients compared to HC. |
| Frey et al.1998 | 1H-MRS Single voxel Frontal Lobe (B/L) |
-22 MDD -22 HC |
1.5T/3.5/55/12cm3 | -mI | Frontal Lobe (Right) -mI/Cr was decreased in MDD patients than HC. Frontal Lobe (Left) -No significant difference. |
| Volz et al.1998 | 31P MRS -Frontal Lobe |
-14 MDD -8 HC |
1.5T/3.0/NA/NA. | -PME -ATP |
Frontal Lobe -Significantly increased PME and decreased ATP in MDD patients as compared to HC. |
| Sanacora et al.1999 | 1H-MRS Single voxel -OC |
-14 MDD (unmedicated) (8 M,6 W) -18 HC (11 M, 7 W) |
2.1T/3.39/68/13.5cm3 | -GABA | OC -Highly significant (52%) reduction in OC GABA levels compared to HC. -No significant relationship between severity of depression and cortical GABA levels. -GABA levels were higher in women (W) than men (M) and they decreased with age. |
| Auer et al.2000 | 1H-MRS Single voxel -ACC -Parietal white matter (PWM) |
-19 MDD (6 M, 13 W) -18 HC (8 M, 10 W) |
1.5T/2.0/35/ 7.5 to 12 mL (ACC), 6.8 to 9.2 mL (PWM) |
-NAA -Cho -Cr -mI -Glx -Glu |
ACC -Significant decrease of Glx in MDD patients (P=0.013). -Considering only severely depressed patients, both Glx and Glu showed a significant decrease (P=0.03). ACC and PWM -No significant effect for NAA, Cr, Cho, mI. |
| Steingard et al.2000 | 1H-MRS Single voxel -OFC |
-17 MDD (P) -28 HC |
1.5T/2.0/30/3.38cm3 | -Cho -Cr |
OFC -Cho/Cr and Cho/NAA ratios were significantly higher in MDD patients than HC (P=0.032 and P=0.043 respectively). |
| Murata et al.2001 | 1H-MRS Single voxel -Frontal lobe WM (Left) |
-47 MDD (E) i. Early onset group (<50 years) ii. Late onset group (>50 years). |
1.5T/2.0/136/8.0cm3 | -NAA | Frontal Lobe WM (Left) -More severe the deep WM lesions lower the levels of NAA/Cr. -Severity of WM lesions was more pronounced in the late onset group. -Indicator of the cell loss in WM of frontal lobes -Late onset group had lower NAA/Cr as well as lower cognitive function in the Digit Symbol, Trail-Making, and Verbal Associative Fluency tests and exhibited higher HDRS scores reflecting more pronounced clinician rated depressive symptoms compared with those in early onset group. |
| Kusumakar et al.2001 | 1H-MRSI (CSI) -Anterior Medial Temporal (Amg) |
-11 MDD (P) -11 HC |
1.5T/1.5/135/NA | -NAA -Cho -Cr |
Amg (Left) -Cho/Cr ratio significantly decreased in MDD patients than HC (P=0.025). -NAA/Cr ratio did not differ significantly between MDD patients and HC. Amg (Right) -Cho/Cr and NAA/Cr ratios did not differ significantly between MDD patients and HC. |
| Farchione et al.2002 | 1H-MRSI (CSI) -DLPFC (B/L) |
-11 MDD (P) -11 HC |
1.5T/2.3/272/0.84 cm3 | -Cho -NAA -tCr |
DLPFC (Left) -Cho was significantly raised (32.5%) in MDD patients than HC (P=0.039). -Cho/Cr ratio was significantly increased in MDD patients than HC (P=0.049). -Cho/NAA ratio was significantly increased in MDD patients than HC (P=0.027). - No significant difference in NAA or Cr between MDD patients and HC. DLPFC (Right) -No significant difference in Cho, NAA or Cr between MDD patients and HC. |
| Kumar et al.2002 | 1H-MRS Single voxel -DLPFC (Left) -ACC (B/L) |
-20 MDD (E) (6 M, 14 W) -18 HC (5 M, 13 W) |
1.5T/3.0/30/8 cm3 | -NAA -Cho -mI -Cr |
Dorsolateral WM -mI/Cr ratio was significantly higher in MDD patients than HC. -Cho/Cr ratio was significantly higher in MDD patients than HC. -No significant difference in NAA/Cr ratio between the two groups. -No difference in absolute metabolite levels between groups. Frontal Gray Matter -No significant differences in metabolite ratios between MDD patients and HC. -No difference in absolute metabolite levels between groups. |
| Vythilingam et al.2003 | 1H-MRS Single voxel and CSI Cortical gray matter (GM), Subcortical GM, and WM |
-18 MDD -20 HC |
1.5T/1.5/20/2.3cm3 | -Cho -NAA -Cr -mI |
Caudate (particularly right side) -NAA/Cr ratio was significantly lower in MDD patients than HC (P<0.05). -mI/Cr ratio was similar in MDD patients and HC. Putamen (particularly right side) -Cho/Cr was significantly higher in MDD patients than HC. (P<0.05). Whole Brain -No significant findings were observed for Cho/Cr, NAA/Cr, or mI/Cr. Thalamus -No significant effects were observed. |
| Smith et al.2003 | 1H-MRSI (CSI) -Medial Thalamus (B/L) -Lateral Thalamus (B/L) |
-18 MDD (P) -18 HC -27 non-depressed patients with obsessive compulsive disorder (OCD) |
1.5T/2.3/272/0.8mL | -Cho | Medial Thalamus (Right) -Cho concentration was significantly increased in OCD than MDD patients and HC (P=0.005 and P=0.008 respectively). Medial Thalamus (Left) -Cho concentration was significantly increased in OCD than MDD patients and HC (P=0.0000 and P=0.002 respectively). Medial Thalamus (B/L) -Cho concentration did not differ significantly between patients with MDD and HC. Lateral Thalamus (Right) -No significant differences in Cho levels between MDD patients, OCD patients and HC. Lateral Thalamus (Left) -Cho concentration was significantly higher in OCD than MDD patients. (P=0.023). -No significant differences between OCD patients and HC, nor between MDD patients and HC |
| Gruber: et al.2003 | 1H-MRS Single voxel -PFC (B/L) (mainly white matter) |
-17 MDD (8 M, 9 W) -17 HC |
3.0T/6.0/20/8cm3 | -NAA -Cr -Cho -mI |
PFC (B/L) -NAA/Cr ratio was significantly lower in MDD patients than controls (Left: P=0.016, Right: P=0.006). -Cho/Cr ratio was significantly lower in MDD patients than controls (Left: Not significant, Right: P=0.016). -mI/Cr ratio was significantly lower in MDD patients than controls (Left: P=0.022, Right: P=0.026). -Absolute concentrations of Cr were significantly higher in MDD patients than HC (Left: P=0.017, Right: P=0.0004). -No difference in absolute concentrations of NAA, Cho and mI. |
| Elderkin-Thompson et al.2004 | 1H-MRS Single voxel -DLPFC (Left) |
-14 MDD (E) -14 HC |
1.5T/2.0/30/27cm3 | -Cho -PCh -PE -mI |
DLPFC (Left) -Among non-depressed people, cognition was positively correlated with Cho/Cr and mI/Cr and negatively correlated with PCh/Cr in four domains of verbal learning, recognition, recall, and hypothesis generation. -Depressed patients did not have consistent relationships between Cho/Cr, mI/Cr, and PCh/Cr and cognition. |
| Mirza et al.2004 | 1H-MRS Single voxel -ACC -OC (10 patients and controls were studied) |
-13 MDD (P); 8 had comorbid psychiatric disorder {4 with anxiety disorders, 1 with ADHD w/o hyperactivity, 1 with Oppositional Defiant Disorder (ODD), 2 with anxiety and ODD} -13 HC; no comorbid disorders. |
1.5T/3.0/30/ 3 cm3 (ACC), 8 cm3 (OC) |
-Glx -Cr -NAA -Cho -mI |
ACC -Glx concentration was significantly lower in MDD patients than HC (19% decrease) with P=0.000. -Reduced Glx was inversely correlated with increased severity of functional impairment as measured by CGI-S (P=0.021), but was not correlated with depressive symptom score as measured by CDRS-R or with illness duration. -Cr concentrations were significantly decreased in MDD patients as compared to HC (P=0.036). -Cr concentrations were not correlated with functional impairment, depressive symptom severity, or illness duration. -No difference in NAA, Cho, or mI was found between the two groups. OC -Glx and Cr did not differ between MDD patients and HC. -No difference in NAA, Cho, or mI was found between the two groups. |
| Sanacora et al.2004 | 1H-MRS Single voxel -OC |
-33 MDD -38 HC |
2.1T/2.0/68/13.5cm3 | -GABA -Glu -NAA -Cho |
OC -GABA lower in MDD patients (P<0.01). -Glu increased in MDD patients (P<0.001), with no effect of age or sex but a significant effect of NAA (P<0.001). -GABA-Glu ratio was significantly higher in patients with MDD (P=0.002). -NAA concentration was not significantly different between the two groups (P=0.16). -Age was significantly associated with NAA concentrations (P=0.03). -Sex had significant effect on choline level (P=0.01). with W and M having choline levels of 1.48 ± 0.15 and 1.39±0.12 mmol/kg respectively. -Significant reductions in percentage of solid tissue (P=0.009) and percentage of WM (P=0.04). -Percentage of tissue, WM, NAA level, age and sex did not have significant effect on GABA levels. -Subtype effect: GABA levels were significantly lower in patients with melancholic depression compared with HC (P<0.001) and in patients with no subtype than HC (P=0.002), but not in patients with atypical depression. |
| Binesh et al.2004 | 1H-MRS Single voxel -DLPFC |
-15 MDD (E) (3 M, 12 W) -33 HC (17 M, 16 W) |
1.5T/2.0/30/27cm3 | -Cho -Cr -Glx -NAA -PE |
DLPFC -In 33 elderly subjects, Cho/Cr ratio was 10 percent higher in M as compared to W. -Depressed geriatric patients had higher levels of mI, PE, and Glx than controls, but these differences were not significant. |
| Rosenberg et al.2004 | 1H-MRS Single voxel -ACC |
-14 MDD w/o OCD -20 non-depressed patients with OCD -14 HC |
1.5T/NA/NA/3.0mL | -Glx | ACC -Glx concentration was significantly decreased in patients with OCD (15.1% decrease) and those with MDD (18.7% decrease) as compared to HC (P=0.002). |
| Brambilla et al.2005 | 1H-MRS Single voxel -Left DLPFC |
-19 MDD -19 HC |
1.5T/6.0/20/8.0cm3 | -NAA -GPC+PC |
DLPFC -NAA/PCr+Cr and NAA/GPC+PC ratios were significantly lower in chronically-ill than less chronically-ill patients. - NAA/PCr+Cr ratio was significantly lower in chronic than less chronic MDD patients and HC (P=0.038). |
| Coupland et al.2005 | 1H-MRS Single voxel -ACC -DMPFC |
-13 MDD (6 M, 7 W); comorbid diagnosis included current GAD (n=3), social anxiety (n=1), lifetime dysthymic disorder (n=2), past panic disorder concurrent with a depressive episode (n=1). -13 HC (6 M, 7 W) |
3.0T/3.0/168/18cm3 | -mI -Cho -NAA |
ACC -mI/Cr ratio was significantly lower in MDD patients than HC (P=0.016). -This reduction in mI could be due to glial loss or altered glial metabolism. -NAA/Cr ratio was not significantly different between patients and controls. -Cho/Cr ratio was not significantly different between patients and controls. |
| Rosenberg et al.2005 | 1H-MRS Single voxel -ACC |
-14 MDD (P) (5 M, 9 W) -14 HC |
1.5T/3.0/30/3cm3 | -Glu -Gln |
ACC -Reduced Glu was observed in MDD patients than HC (P=0.0002; 23% decrease). -Gln did not differ significantly. |
| Hasler et al.2005 | 1H-MRS Single voxel -VMPFC -DLPFC |
-16 rMDD -15 HC |
3.0T/NA/68/ 18 cm3(VMPFC), 30 cm3 (DLPFC). |
-GABA -Glx -Cho -NAA |
VMPFC -No difference in GABA concentration between rMDD patients and HC. -Negative relationship between Glx/GABA ratio and age of onset of MDD. DLPFC -No difference in GABA concentration between rMDD patients and HC. |
| Caetano et al.2005 | 1H-MRS Single voxel -DLPFC (Left) |
-14 MDD (P) -22 HC |
1.5T/6.0/30/8.0cm3 | -GPC+PCh -mI -Glu |
DLPFC (Left) -GPC+PCh was significantly decreased in MDD patients as compared to HC. -mI concentration was higher in patients with MDD. -Glu level was inversely correlated with duration of illness as well as number of episodes. |
| MacMaster and Kusumakar 2006 | 1H-MRS Single voxel -PFC (Right) |
-12 MDD (P) -11 HC |
1.5T/1.5/135/4.0cm3 | -Cho -Cr |
PFC (Right) -Cho/Cr ratio was significantly increased in MDD patients as compared to HC (P=0.007). |
| Ajilore et al.2007 | 1H-MRS Single voxel -Subcortical nuclei (B/L) -DLPF WM (B/L). |
-20 diabetics with MDD -24 diabetics w/o MDD -21 HC |
1.5T/3.0/30/4.0mL | -NAA -Glx -Cr -Glu -Gln -Cho -mI |
Subcortical Regions -Gln and Glu concentrations were significantly lower in depressed diabetic patients as compared to HC and diabetic control subjects (P<0.001). -A significant difference between hemispheres (P=0.04) with the decrease in Glx concentration found in depressed diabetics more pronounced in left voxel. Frontal WM -mI was significantly increased in diabetic control subjects and depressed diabetic patients as compared to HC. (P<0.05). -No significant hemispheric differences in metabolite concentrations. |
| Ende et al.2007 | 1H-MRS -Putamen (B/L) -HPC (B/L) |
-11 MDD -10 HC |
1.5T/1.5/135/1.04cm3 | -Cho -tCr -NAA |
BG -Cho was significantly higher in MDD patients than HC. HPC -Cho was significantly lower in MDD patients than HC. BG and HPC -No difference between left and right side. |
| Hasler et al.2007 | 1H-MRS Single voxel - DMPFC - VMPFC |
- 20 MDD (unmedicated) - 20 HC |
3.0T/1.5/68/ 30cm3(DMPFC), 18cm3(VMPFC). |
- Glx - GABA -NAA -Cho |
DMPFC - Lower Glx and GABA in MDD patients than HC (P<0.02 and P<0.02 respectively). VMPFC - Lower Glx in MDD patients than HC (P<0.02). - Cho concentration was more in M than W (P<0.007) DMPFC and VMPFC -In this study, difference was more prominent in W than M. -Positive correlation between Glx and GABA (P<0.001 and P<0.04). -No correlation with depression severity. -Negative correlation between age and NAA (P<0.001 and P<0.008). |
| Gabbay et al.2007 | 1H-MRSI (CSI) -Caudate, Putamen and Thalamus (B/L) |
-14 MDD (P) -10 HC |
3.0T/1.6/135/0.75 cm3 |
-Cho -Cr |
Caudate (Left) -Cho concentration was significantly increased in patients with MDD than HC (P<0.03). -Cr concentration was significantly increased in patients with MDD than HC (P<0.04). -No other neurochemical differences were observed. |
| Bhagwagar et al.2007 | 1H-MRS Single voxel -OC |
-15 rMDD -16 bipolar -18 HC |
3.0T/6.0/26/18cm3 | -GABA -Glx -NAA |
OC -GABA/Cr and NAA/Cr were significantly lower in rMDD and bipolar patients than in HC, whereas Glx/Cr was higher. |
| Bhagwagar et al. 2008 |
1H-MRS Single voxel -OC -ACC |
-12 rMDD -11 HC |
3.0T/3.0/68/18cm3 | -GABA | OC -Lower GABA/Cr in rMDD patients than HC. -Glx/Cr significantly higher in patients than HC. ACC -Lower GABA/Cr in rMDD patients than HC. |
| MacMaster et al.2008 | 1H-MRSI (CSI) -Medial Temporal Cortex (B/L) |
-11 MDD (P) -11 HC |
1.5T/2.3/272/0.8mL | -NAA | Medial Temporal Cortex (Left) -NAA was decreased by 27% in MDD patients as compared to HC (P=0.003). |
| Chen et al.2009 | 1H-MRS Single voxel -Frontal WM (Left) -PV WM (Left) -BG (Left) |
-27 MDD (E); 9 on antidepressant -19 HC |
3.0T/1.5/30/8cm3 | -NAA -Cho -mI -Cr |
Frontal WM (Left) -NAA/Cr ratio was significantly lower in un-medicated MDD patients than HC (P<0.02). -No significant difference in Cho/Cr, mI/Cr ratios across the three groups (medicated MDD patients, unmedicated MDD patients, HC). PV WM (Left) -No differences in the metabolite ratios. BG (Left) -Cho/Cr and mI/Cr ratios were significantly higher in MDD patients than HC (P<0.046 and P<0.025). |
| Milne et al.2009 | 1H-MRS Single voxel -HPC |
-14 MDD (first episode) -13 HC for first episode MDD group -14 MDD (recurrent) -14 HC for recurrent MDD |
3.0T/2.0/35/8cm3 | -NAA -mI -Glx -GPC -GPC+PCh |
HPC -GPC+PCh and GPC were significantly elevated in patients with recurrent MDD than controls. -No other metabolite difference was significant between patients with recurrent MDD and HC. -mI levels were significantly increased in first time depression patients as compared to HC. -No other metabolite difference was significant between patients of first time depression and HC. |
| Walter et al. 2009 | 1H-MRS Single voxel -pgACC (Right) |
-19 MDD -24 HC |
3.0T/2.5/31-229/ 17.5mL |
-Gln -Glu -NAA -GABA -Gluc |
pgACC -Gln was decreased (P=0.01), Glu and GABA were normal in highly anhedonic MDD patients. -Glu and NAA correlate with negative BOLD responses induced by emotional stimulus in MDD; in HC negative BOLD responses correlate with GABA instead. -Negative BOLD responses, Glu and NAA correlate with emotional intensity ratings in those with MDD but not in HC. |
| Nery et al.2009 | 1H-MRS Single voxel -DLPFC (Left) |
-37 MDD -40 HC |
1.5T/3.0/30/8.0 cm3 | -NAA -Cr -Cho -mI -Glx |
DLPFC -Metabolite levels did not differ between MDD patients and HC. -NAA levels inversely correlated with length of illness. Effect of gender: -Male MDD patients had lower PCr+Cr than male HC. -Female MDD patients had higher PCr+Cr than female HC. |
| Price et al.2009 | 1H-MRS Single voxel -OC -ACC |
-15 MDD (treatment resistant; Tr) -18 MDD (non-Tr) -24 HC |
3.0T/1.5/68/ 18.0cm3(OC), 18.75 cm3 (ACC). |
-GABA -Glx |
OC -GABA significantly decreased in Tr MDD patients than HC and non-Tr MDD patients. -Glx was not different. -Glx/GABA ratio was significantly elevated in the Tr MDD patients than HC, while no difference was found between non-Tr MDD and Tr MDD patients or HC. ACC -GABA decreased in Tr MDD patients than HC and non-Tr MDD patients, but the difference was not significant. -Glx was not different -Glx/GABA did not differ between Tr MDD patients, non-Tr MDD patients and HC. |
| Venkatraman et al.2009 | 1H-MRS Single voxel -Medial PFC -Medial temporal lobe |
-14 MDD (E) -12 HC |
3.0T/3.0/30/8cm3 | -NAA -Cho -mI -Cr |
PFC -NAA, Cho and Cr decreased in MDD patients compared to HC. Medial Temporal Lobe (Left) -NAA and mI increased in MDD patients compared to HC. Medial Temporal Lobe (Right) -No significant difference in metabolites between MDD patients and HC. |
| Gabbay et al. 2010 | 1H-MRSI (CSI) -BG (Left Putamen and Right Caudate) |
-7 MDD (P); melancholic -7 MDD (reactive); non-melancholic. -6 HC |
3.0T/1.6/135/0.75cm3 | -Cho | BG (Left Putamen, Right Caudate) -No significant correlations were found in the HC group or in the MDD group as a whole. -In Melancholic patients, plasma KYN concentrations were positively correlated with right caudate total choline (P=0.03). -In Melancholic patients, plasma 3-hydroxyanthranilic acid (3-HAA), a neurotoxic intermediate of the KYN Pathway) was positively correlated with left putamen total choline (P=0.006). |
| Horn et al.2010 | 1H-MRS Single voxel -pgACC (B/L) -AI (Left) |
-22 MDD -22 HC |
3.0T/2.0/80/ 4.0ml (pgACC), 3.0ml (AI) |
-Glx -Glu -mI -NAA |
pgACC (B/L) -Glx/Cr and Glu/Cr ratios predicted functional connectivity between the two regions in MDD patients, but not in HC. -Lower Glx/Cr predicted weaker negative correlations i.e. functional connectivity between regions. -Glx/Cr and Glu/Cr were lower in severely depressed than mildly depressed patients and HC. - A significant difference of Glu and Glx levels was found between mildly depressed patients and HC. AI (Left) -Glx/Cr failed to predict connectivity between the two regions. -Significant correlation between HDRS and resting state functional connectivity between the regions. -mI and NAA did not show any significant finding. |
| Olvera et al.2010 | 1H-MRSI (CSI) -Medial PFC -ACC -DLPFC |
-16 MDD (P) -38 HC |
1.5T/1.5/272/1.5cm2 | -NAA -PCr+Cr -GPC+PCh |
DLPFC -No significant difference in GPC+PCh levels between MDD group and HC. -A trend towards decreased NAA noted in the left DLPFC GM and right DLPFC WM. ACC (Right) -A significant reduction in NAA was noted in MDD patients. Medial PFC (Right) -A significant reduction in NAA was noted in MDD patients. |
| Portella et al.2011 | 1H-MRS Single voxel -VMPFC |
-10 MDD (first episode) -16 MDD (remitted-recurrent) -19 MDD (chronic) -15 HC |
3.0T/2.0/38/8.0cm3 | -Glu -Cho -NAA |
VMPFC -Glu significantly decreased in remitted-recurrent and chronic patients compared to first-episode patients and HC. -Cho was increased in patients with chronic depression and showed a positive correlation with duration of illness. -NAA was significantly lower in remitted-recurrent and chronic patients. |
| Gabbay et al.2012 | 1H-MRS Single voxel -ACC |
-20 MDD (P); 10 with anhedonia -21 HC |
3.0T/1.5/68/18.75cm3 | -GABA | ACC -GABA was significantly low in MDD patients as compared to HC (p<0.003). -Only patients with anhedonia had decreased GABA levels (p<0.001). |
| Wang et al.2012 | MRSI (CSI) -Anterior cingulate (AC) GM -DLPF WM |
-24 MDD (10 M, 14 W) -13 HC (6 M, 7 W) |
1.5T/1.0/144/ 0.5625cm3 |
-NAA -Cho -Cr |
DLPF WM (Left) -NAA/Cr and Cho/Cr were significantly lower in MDD patients as compared to HC. DLPF WM (Right) -NAA/Cr was significantly lower in MDD patients as compared to HC. AC GM (B/L) -NAA/Cr and Cho/Cr were not significantly different in MDD patients and HC. No correlation was found between metabolite ratios, HDRS scores, and duration of illness. |
| Sozeri-Varma et al.2013 | 1H-MRS Single voxel -PFC (right) |
-21 mild MDD -18 moderate MDD -16 HC |
1.5T/3.0/35 and 144/8cm3 | -NAA -Cho -Cr |
PFC (Right) -NAA/Cr was significantly lower in moderate MDD patients as compared to HC. -No difference in NAA/Cr between mild MDD sufferers and HC. -No difference in NAA, Cr, Cho, Cho/Cr among mild MDD, moderate MDD and HC. |
Table 1: Literature Review of MRS and MRSI in Depression (arranged in chronological order).
| Authors | Voxel placement | Subjects | Magnet strength/TR(sec)/TE(msec)/ voxel size | Therapy (Tx) | Meta bolites | Findings |
|---|---|---|---|---|---|---|
| Charles et al. 1994 | 1H-MRSI (CSI) cortical and non-cortical GM (e.g. BG, thalamus) as well as WM. |
-7 MDD (E) -10 HC |
1.5T/2.0/NA/ 3.0cm3 |
Anti- depressant |
-NAA -Cho -Cr |
BG/Thalamus/WM (At level of Third Ventricle) -NAA/Cr was not significantly different from pre-therapy to post-therapy, nor was any change significant from control group. -NAA/Cho increased significantly from pre-therapy to post-therapy (P=0.042). -Cho/Cr level fell significantly from pre-therapy to post-therapy (P=0.026). -Pre-therapy Cho/Cr level was elevated in MDD patients as compared to HC (P=0.022) and fell to sub-control levels post therapy (P=0.011). |
| Renshaw et al. 1997 | 1H-MRS Single Voxel -BG |
-41 MDD (18 responders, 23 non-responders) -22 HC |
1.5T/2.0/30/8.0 cm3 | SSRI (8 weeks Flouxetine) |
-Cho -NAA |
BG -Cho/Cr ratio was significantly lower in MDD patients than HC (P=0.037). -This difference was more pronounced in the responders than in the non-responders. -NAA/Cr ratio was not significantly different between MDD patients and HC. |
| Sonawalla et al. 1999 | 1H-MRS Single Voxel -BG (Head of left caudate and putamen) |
-41 MDD before Tx -15 MDD after Tx. |
1.5T/NA/NA/ 8.0 cm3 |
SSRI (Fluoxetine) | -Cho -Cr |
BG -Cho/Cr ratio was increased by 20% in Tx responders than non-responders. -Cho/Cr ratio was decreased by 12% in non-responders. |
| Ende et al. 2000 | 1H-MRSI (CSI) -HPC |
-17 MDD (received ECT) -24 HC plus 6 remitted from MDD w/o ECT. |
1.5T/1.8/135/ 2.4 cm3 |
-ECT | -NAA -Cho -Cr |
HPC -NAA did not show any change after ECT Tx. -Cho was increased by 16% after 5 or more ECT Tx. Despite unilateral ECT in most patients, the increase in Cho was B/L. |
| Sanacora et al. 2002 | 1H-MRS Single Voxel -OC |
-11 MDD (7 M, 4 W) |
2.1T/3.39/68/ 13.5 cm3 |
-SSRI (2 months) | -GABA | OC -GABA concentration was significantly increased in patients after treatment with SSRI (P<0.03). |
| Pfleiderer et al. 2003 | 1H-MRS Single Voxel -ACC (Left) |
-17 (severe) MDD before and after ECT. -17 HC |
1.5T/2.5/20/ 3.375 cm3 |
-ECT | -Glx | ACC (Left) -Glx levels were significantly reduced in patients with MDD than HC. -Glx levels normalized (P=0.04) in ECT responders as compared to non-responders and then did not differ statistically from controls. |
| Kaufman et al. 2003 | 1H-MRSI (CSI) -ACC |
-13 MDD (stabilized on fluoxetine) -13 MDD (stabilized on paroxetine) |
1.5T/2.0/65/ 1.28 cm3 |
-SSRI discontinuation (MRSI done 3 days after medicine substitution with active SSRI and placebo. |
-Cho -Cr |
ACC -Cho/Cr ratio was decreased in 4 ‘paroxetine group’ and 2 ‘flouxetine group’ subjects as compared to asymptomatic subjects. |
| Michael et al. 2003b |
1H-MRS Single Voxel -Amygdalar region (Left) (Amg, GM and Anterior 1/3rd of HPC) |
-28 Tr MDD (being referred for ECT) -28 HC |
1.5T/2.5/20/ 3.375 cm3 |
-ECT | -NAA -Cho -Cr |
Amygdalar region (Left) -NAA, Cho and Cr concentrations did not differ between controls and patients before receiving ECT. Only Glx showed a trend towards reduction (P=0.056). Glx reduction was significant only in patients with unipolar depression (P=0.049). -NAA and Glx levels were increased after successful ECT in all patients compared to the baseline values before ECT. (P=0.019 and P=0.049 respectively). |
| Michael et al. 2003a |
1H-MRS Single Voxel -DLPFC (Left) |
-12 MDD (episode with melancholic features). -12 HC |
1.5T/2.5/20/ 3.375 cm3 |
-ECT | -Glx | DLPFC (Left) -Glx levels were decreased in pre-ECT patients compared to HC (P=0.002); Glx levels correlated negatively with severity of depression. -Glx levels significantly increased after Tx with ECT, and levels no longer differed from those of HC. (P=0.016 and P=0.90 respectively). |
| Sanacora et al. 2003 | 1H-MRS Single Voxel -OC |
-8 MDD (before and after a course of ECT) |
2.1T/3.39/68/ 13.5cm3 |
-ECT | -GABA | OC -GABA concentration was significantly increased after ECT Tx (P<0.02). -A significant decrease in seizure duration was seen. -Significant decrease in level of depression severity following ECT was noticed. |
| Obergriesser et al. 2003 | 1H -MRSI -HPC |
-12 out of 17 with MDD who were once treated with ECT. | 1.5T/1.8/135/2.4 cm3 | -ECT | -Cho -NAA |
HPC -ECT has no influence on NAA. -The significant increase in Cho seen earlier during ECT was reversed at long-term follow up. |
| Bhagwagar et al. 2004 | 1H-MRS Single Voxel -OC |
-10 healthy volunteers (9 M, 1 W) |
3.0T/3.0/68/ 27cm3 |
-SSRI (10 mg citalopram) | -GABA -Cr |
OC GABA/Cr ratio was increased by 34.5% in subjects who were given SSRI (P<0.04). |
| Gonul et al. 2005 | 1H-MRS Single Voxel -Medial Frontal Cortex |
-20 MDD -18 HC |
1.5T/1.5/135/ 8.0 cm3 |
-Anti- depressant |
-NAA | Medial Frontal Cortex -NAA/Cr was lower pre-treatment in MDD patients than HC but this difference was not significant. -Antidepressants had significant effect on NAA/Cr ratio (P=0.03). -NAA/Cr ratio increased significantly post-treatment compared to pre-treatment levels (P=0.004). -No significant difference observed between post-treatment NAA/Cr value of patients and HC. |
| Sanacora et al. 2006 | 1H-MRS Single Voxel -OC |
-8 MDD (Before and after course of CBT) |
2.1T/3.39/80/20.475cm3 | -CBT | -GABA | OC -No significant changes in GABA after treatment with CBT. -HDRS scores significantly decreased after CBT. |
| Taylor et al. 2008 | 1H-MRS Single Voxel -OC |
-30 Healthy volunteers | 3.0T/3.0/26/ NA |
-SSRI | -Glx | OC -Glx levels were significantly increased in healthy volunteers receiving citalopram for 7 days as compared to both volunteers receiving reboxetine and placebo. |
| Block et al. 2009 | 1H-MRS Single Voxel -HPC |
-18 MDD (13 got a 2nd test after 8 weeks of Tx with citalopram or nortryptyline -10 HC |
3.0T/2.0/ 140 and 30/ 6.0mL |
-SSRI or TCA | Short TE -Glu+Gln+GABA -Gln -mI Long TE -NAA -Cho |
HPC -Glu+Gln+GABA/Cr and Gln/Cr were significantly reduced in MDD patients. -Gln/Glu+Gln+GABA also showed a trend towards significant reduction. -Tx caused a rise in NAA and Cho. -Low baseline NAA and Cho levels predicted positive treatment effects. |
| Kaymak et al. 2009 | 1H-MRS Single Voxel -DLPFC (Left) |
-17 MDD (first episode) -13 HC (All female subjects) |
3.0T/3.0/30/3.375cm3 | -Antidepressant (8 weeks) | -mI -Cho -NAA |
DLPFC (Left) -No difference in pre-treatment levels of NAA/Cr, mI/Cr, Cho/Cr between MDD and controls. -Significant differences in mI/Cr between pre- and post-treatment. -No difference in NAA/Cr and Cho/Cr ratios. |
| Murck et al. 2009 | 1H-MRS Single Voxel -DLPFC -POC |
-13 MDD {Before and after 24 hours of total sleep deprivation (TSD)}. | 1.5T/4.0/35/ 5.8mL (DLPFC), 17.5mL (POC). |
-TSD | -Glu+Gln+GABA -Cho -Cr |
DLPFC -TSD did not change Glu+Gln+GABA or its elements (overall). -Cr and Cho increased marginally with TSD. -TSD leads to increase in Glu+Gln+GABA and Gln in male patients only. POC -No change observed. |
| Merkl et al. 2010 | 1H-MRS Single Voxel -DLPFC (Left) -ACC (Left) |
-25 MDD -27 HC |
3.0T/0.02053/3.8/ 8 cm3 (DLPFC), 20 cm3 (ACC) |
-ECT (9 sessions, right ultrabrief pulse ECT) | -NAA -Cho -tCr -Glu |
DLPFC (Left) -Baseline concentrations of metabolites were not significantly different between MDD patients and HC. -After ECT, NAA levels were significantly decreased in responders compared to non-responders (P=0.04). ACC (Left) -Baseline Glu (P<0.001) and NAA (P=0.005) levels were significantly decreased in all MDD patients compared to HC. -Baseline Glu and NAA differences were significant between HC and responders only (P=0.02 and P=0.002 respectively). -High Glu at baseline predicted a greater treatment response. -After ECT, increased NAA levels were observed in responders and tCr levels were significantly decreased across all depressive patients. DLPFC and ACC -No significant differences were found in baseline metabolites between responders and non-responders. |
| Taylor et al. 2010 | 1H-MRS Single Voxel -ACC |
-23 volunteers (11 M, 12 W) | 3.0T/3.0/26/8.0cm3 | -SSRI (7-10 days of citalopram/placebo) | -Glu -Glx |
ACC No effect of treatment. |
| Valentine et al. 2011 | 1H-MRS Single Voxel -OC |
-10 MDD | 4.0T/2.5/68/ 13.5 cm3 |
-Ketamine | -Glu -GABA -Gln |
OC -Changes in Glu, Gln and GABA were not significantly associated with changes in depressive symptoms. -No evidence that baseline metabolite levels can serve as a predictive biomarker for clinical response. -Significant decrease in BDI and HDRS scores after ketamine treatment. -Antidepressant effect persisted for up to one week. |
| Kondo et al. 2011b | 31P MRS -Corpus Callosum (CC) -Anterior Commissure (AC) -Posterior Commissure (PC) |
-5 MDD (P); SSRI-resistant -6 HC (All female subjects) |
3.0T/2.0/ 3.37/15.6 cm3 |
-Cr (4g oral) | -PCr | CC/AC/PC -Significant increase in PCr concentration (p=0.02). |
| Salvadore et al. 2011 | 1H-MRS Single Voxel -VMPFC -DMPFC |
-14 MDD (9 M, 5 W) |
3.0T/1.5/68/ 18.0 cm3 (VMPFC), 30.0 cm3 (DMPFC) |
-Ketamine | -GABA -Glu -Glx/Glu |
VMPFC -Pre-treatment GABA did not correlate with improved depressive symptoms after ketamine infusion. -Pre-treatment Glu did not correlate with improved depressive symptoms after ketamine infusion. -Pre-treatment Glu was positively correlated with improvement in anxiety symptoms. DMPFC -Pre-treatment GABA did not correlate with improved depressive symptoms after ketamine infusion. -Pre-treatment Glu did not correlate with improved depressive symptoms after ketamine infusion. -Pre-treatment Glx/Glu was negatively correlated with improvement in depressive symptoms. |
| Jarnum et al. 2011 | 1H-MRS Single Voxel -ACC |
-23 MDD (7 M, 16 W) -26 HC (13 M, 13 W) |
3.0T/2.0/30/8.0cm3 | -Antidepressant | -NAA -mI -Glu -Glx -GPC -Cr |
ACC -Low levels of NAA, mI, and Glu have been found in MDD patients as compared to HC at baseline. -Increase in mI was seen after 6 months of antidepressant Tx. |
| Kalkan Oguzhanoglu et al. 2014 | 1H-MRS Single Voxel -PFC (right) |
-18 MDD (W) -10 HC (W) |
1.5T/3.0/85/8.0cm3 | -Antidepressant -Psychotherapy |
-NAA -Cho -Cr -NAA/Cr -Cho/Cr |
PFC (Right) -No significant change in metabolites in MDD patients and HC at baseline, after antidepressant therapy or after therapy with antidepressant combined with psychotherapy. |
Table 2: Treatment of Depression: Changes in Brain Metabolites (arranged in chronological order).
N-Acetyl Aspartate (NAA) Findings
The NAA resonance has the highest peak in a normal human brain spectrum (Ende et al., 2006; Maddock & Buonocore, 2012). NAA is a marker for neuronal integrity. A decrease in NAA level represents reversible or irreversible affection of neuronal viability or function (Ende et al., 2006; Maddock & Buonocore, 2012; Moffett et al., 2007).
NAA level is decreased in the medial temporal region of pediatric depression patients (MacMaster et al., 2008), the ACC of pediatric (Olvera et al., 2010) and adult patients (Järnum et al. 2011), as well as the PFC of pediatric (Olvera et al., 2010) and elderly patients (Venkatraman et al., 2009). In elderly patients, NAA is reported to be increased in the left medial temporal lobe (Venkatraman et al., 2009). The NAA/Cr ratio was also found lower in the BG (Vythilingam et al., 2003), frontal white matter (WM) (Chen et al., 2000), DLPF WM (Wang et al., 2012), and PFC of MDD patients (Gruber et al., 2003; Sözeri-Varma et al., 2013); however, this ratio was shown to be normal in ACC (Wang et al., 2012; Coupland et al., 2005), the right PFC (O√?¬?uzhano√?¬?lu et al., 2014) and the left DLPFC by another study (Kaymak et al., 2009). Nery et al., (2009) also showed normal value for NAA in the DLPFC. In the pgACC, NAA correlates with negative BOLD responses and emotional intensity ratings in MDD patients (Walter et al., 2009). The NAA concentrations in the HPC showed a significant increase after treatment with antidepressants (Block et al., 2009) but not with ECT (Obergriesser et al., 2003; Ende et al., 2000). Low pre-treatment levels of NAA in HPC also predict a favorable response to antidepressants (Block et al., 2009). In the BG, NAA/Cr does not change significantly after antidepressant therapy (Renshaw et al., 1997; Charles et al., 1994). Michael et al. (2003a) has shown increased concentration of NAA in the Amg after successful ECT, and yet another study has documented decreased NAA/Cr in the occipital cortex (OC) of fully recovered MDD (rMDD) patients (Bhagwagar et al., 2007).
The age of onset is an important variable affecting the level of NAA. It has been shown that NAA/Cr is negatively related to the severity of deep WM lesions in the frontal lobe. WM is more severely affected in those with a late age of onset as compared to patients who have an early onset. Late onset is correlated with lower NAA/Cr, as well as lower cognitive function as seen in Digit Symbol, Trail-Making, and Verbal Associative Fluency tests. People with an advanced age of depression onset also have higher Hamilton depression rating scale (HDRS) scores reflecting more severe symptoms (Murata et al., 2001).
One study has evaluated the differences in NAA values between chronically ill patients and those suffering since lesser duration. The NAA/phosphocreatine plus creatine (NAA/PCr+Cr) and NAA/ glycerophosphocholine plus phosphocholine (NAA/GPC+PCh) ratios were found significantly lower in left DLPFC of chronic MDD patients (Brambilla et al., 2005a). Furthermore, significantly decreased NAA in the ventromedial PFC (VMPFC) has been seen in chronically ill patients and in those with remitting-recurrent pattern than first time sufferers or healthy individuals (Portella et al., 2011).
Since brain metabolites are dependent variables, NAA/Cr ratio might represent a better indicator of internal milieu than absolute NAA concentration as it takes into account the level of Cr in that condition. Although the absolute value of NAA has been shown to decrease in the ACC of MDD patients (Järnum et al. 2011), the ratio NAA/Cr only follows a decreasing trend with no significant difference reported (Wang et al., 2012; Sözeri-Varma et al., 2013). Similarly the discrepancies noted in the PFC could be accounted for. Nery et al. (2009) report no significant difference in NAA concentration in the PFC whereas several other studies report a significant decrease in NAA/Cr ratio in the DLPFC (Wang et al., 2012; Sözeri-Varma et al., 2013). Although, Kaymak et al. (2009) report no difference in NAA/Cr ratio between MDD sufferers and controls, they have used a large region of interest, including both gray and white matters, which cannot negate the findings of other researchers focusing mainly on the WM.
Choline (Cho) Findings
The Cho peak in the MRS spectrum is a result of a number of compounds containing the choline molecule (Ende et al., 2006; Maddock & Buonocore, 2012; Yildiz-Yesiloglu & Ankerst, 2006). GPC and PCh are the main compounds recorded in the peak (Ende et al., 2006; Maddock & Buonocore, 2012; Yildiz-Yesiloglu & Ankerst, 2006; Boulanger et al., 2000; Kusumakar et al., 2001). Membrane bound phospholipids are not well captured in the MRS signal (Maddock & Buonocore, 2012; Yildiz-Yesiloglu & Ankerst, 2006); however, the MRS signal is influenced by the number of cell membranes in the studied voxel, and the turnover rate of these membranes (Maddock & Buonocore, 2012; Yildiz-Yesiloglu & Ankerst, 2006; Glitz et al., 2002; Moore & Galloway, 2002; Yue et al., 2009). The higher the membrane turnover, the higher the Cho concentration level (Maddock & Buonocore, 2012; Yildiz-Yesiloglu & Ankerst, 2006; Ende et al., 2000; Ende et al., 2006; Boulanger et al., 2000; Glitz et al., 2002; Geddes et al., 1997; Danielsen & Ross 1999).
The concentration of Cho has been found higher in the BG of unipolars and bipolars in depressive state (Hamakawa et al. 1998; Ende et al., 2007; Gabbay et al., 2007), as well as in the left DLPFC; but alike in the right DLPFC (Farchione et al., 2002), Amg (Michael et al., 2003b), medial and lateral thalamus (Smith et al., 2003), and ACC of MDD patients and healthy individuals (Coupland et al., 2005; Auer et al., 2000; Mirza et al., 2004). One study, however, reported no significant metabolite difference between the left DLPFC of MDD and healthy individuals (Nery et al., 2009). Similarly the ratio Cho/Cr was detected significantly higher in BG (Charles et al., 1994; Vythilingam et al., 2003; Chen et al., 2009), particularly on the right side (Vythilingam et al., 2003), the OFC (Steingard et al., 2000) and the left DLPFC (Kumar et al., 2002; Farchione et al., 2002); lower in left Amg (Kusumakar et al., 2001); and similar in right DLPFC (Farchione et al., 2002), right Amg (Smith et al., 2003), and ACC of patients and matched-controls (Coupland et al., 2005; Auer et al., 2000; Mirza et al., 2004). Low levels of Cho/Cr have been found in the WM of left sided DLPF area (Wang et al., 2012). Discontinuing antidepressants in patients taking medicines have manifested with a decrease in Cho/Cr in the ACC (Smith et al., 2003). In DLPFC of healthy individuals, the Cho/Cr concentration correlates positively, whereas the PCh/Cr relates negatively with cognition; however no such association has been found in depressed patients (Elderkin- Thompson et al., 2004). Antidepressant therapy has been shown to significantly drop the Cho/Cr in the BG (Charles et al., 1994). Different measurement techniques or other variables could account for contradicting findings of low Cho/Cr in the BG (Sonawalla et al., 1999; Renshaw et al., 1997), which rise significantly after antidepressant therapy (Sonawalla et al., 1999). Some studies have also calculated Cho/NAA ratio and found raised values in the BG (Hamakawa et al., 1998), OFC (Steingard et al., 2000), and left DLPFC; yet identical in the right DLPFC (Farchione et al., 2002). Elevated Cho/PCr+Cr ratio has been appreciated in the BG of MDD sufferers (Hamakawa et al., 1998). An interesting difference was found in the right PFC. Pediatric MDD population showed increased Cho/Cr ratio (MacMaster & Kusumakar, 2006); however, the adult subjects demonstrated a decreased Cho/Cr ratio on the right side, with no difference on left (Gruber et al., 2003). Furthermore, since greater than 60% of MDD patients are at a risk of recurrence (Soleimani et al., 2011), it is also pertinent to see metabolite changes in this patient population. One study has shown an elevated level of GPC+PCh and GPC alone in the HPC of patients with recurrent MDD (Milne et al., 2009). ECT has been shown to affect the Cho levels in brain significantly. Ende et al. (2000) conducted a study which showed bilateral hippocampal increase of 16% in Cho levels after 5 or more ECT treatments. Long-term follow-up of patients treated with ECT has, however, revealed a reversal of the increased HPC Cho amount post-ECT to levels seen before giving ECT (Obergriesser et al., 2003). Cho, which was found lower in the HPC (Ende et al., 2000; Ende et al., 2007), also increased after treatment with antidepressants, with lower levels of Cho predicting better therapy results (Block et al., 2009). GPC+PCh value has been found decreased in the DLPFC of MDD individuals (Caetano et al., 2005). Cho also shows a positive correlation with duration of illness; increased levels have been detected in the VMPFC of chronically ill patients in comparison to those with a shorter duration (Portella et al., 2011).
Changes in glial density have been documented in MDD and the total choline (tCho) is particularly relevant to this (Hercher et al., 2009). tCho has been repeatedly shown to be abnormal in MDD patients (Tables 1 and 2). Increased activity of the enzyme indoleamine 2,3-dioxygenase is reported in MDD. This enzyme is responsible for the breakdown of tryptophan (TRP) into kynurenine (KYN); decreasing TRP and serotonin levels in the brain (Catena- Dell'Osso et al., 2011; Kurz et al., 2011; Maes, 2011; Müller et al., 2011). Positive correlations have been found between plasma KYN and tCho in the right caudate of patients with melancholic depression. Plasma 3-hydroxyanthranilic acid (3-HAA-an intermediate of KYN pathway) and the tCho in left putamen are also shown to be positively correlated in melancholic MDD patients (Gabbay et al., 2010).
Out of 12 papers on adult population (Block et al., 2009; Ende et al., 2007; Sonawalla et al., 1999; Renshaw et al., 1997; Michael et al., 2003b; Vythilingam et al., 2003; Gruber et al., 2003; Coupland et al., 2005; Nery et al., 2009; Hamakawa et al. 1998; Auer et al., 2000; Milne et al. 2009), two noted decreased Cho in the HPC (Block et al., 2009; Ende et al., 2007), two noted decreased Cho in the BG (Sonawalla et al., 1999; Renshaw et al., 1997), one noted decreased Cho in the PFC (Gruber et al., 2003), three noted raised Cho in the BG (Vythilingam et al., 2003; Hamakawa et al. 1998; Ende et al., 2007), two noted normal Cho in the ACC (Coupland et al., 2005; Auer et al., 2000), and one noted normal Cho in the Amg (Michael et al., 2003b) and another noted normal Cho in the DLPFC (Nery et al., 2009). One study on the adults experiencing recurrent episodes of MDD found increased levels of Cho in the HPC (Milne et al. 2009). Eight papers focused on Cho in the pediatric population (Kusumakar et al., 2001; Gabbay et al., 2007; Farchione et al., 2002; Smith et al., 2003; Mirza et al., 2004; Steingard et al., 2000; MacMaster & Kusumakar, 2006; Caetano et al., 2001). Four found increased concentrations of Cho (MacMaster & Kusumakar, 2006; Steingard et al., 2000; Gabbay et al., 2007; Farchione et al., 2002), three found normal concentrations (Farchione et al., 2002; Smith et al., 2003; Mirza et al., 2004), one found decreased concentrations in the DLPFC (Caetano et al., 2001), and one study found normal Cho in the right Amg but decreased Cho in the left Amg (Kusumakar et al., 2001). Out of the 5 papers on elderly patients (Kumar et al., 2002; Ende et al., 2007; Charles et al., 1994; Chen et al., 2009; Obergriesser et al., 2003), two found increased Cho in the BG (Charles et al., 1994; Chen et al., 2009), two found decreased Cho in the HPC (Ende et al., 2007; Obergriesser et al., 2003), and one found increased Cho in the DLPFC (Kumar et al., 2002). Antidepressants were shown to rectify the Cho levels in the BG as well as the HPC of both adults and elder patients (Charles et al., 1994; Block et al., 2009), whereas ECT was shown in elderly patients to initially increase the Cho levels in the HPC followed by a fall in levels (Ende et al., 2007).
Summarizing the above findings, there appears to be a great controversy between results of different studies. This is because a lot of factors play a role in regulating Cho concentration in the brain, and most studies have followed different agendas. For example, most studies have failed to categorize their measurements of Cho from WM or GM. White matter seems to be more representative of Cho variations pertinent to MDD disease activity (Wang et al., 2012). In the adult population, Cho/Cr has been found decreased in the WM of DLPFC, suggesting compromised signal transduction and decreased myelination (Wang et al., 2012); whereas, in elderly subjects it has been shown to increase (Kumar et al., 2002). Kaymak et al. (2009) found normal Cho concentrations in the DLPFC of adult patients, which could simply be due to their large region of interest comprising of both GM and WM of DLPFC. On the other hand, although Wang et al. (2012) reported decreased Cho/Cr in the WM of DLPFC, there study population excluded patients with a first degree relative having depression. This could explain the discrepancy as two studies reported increased Cho concentrations in patients having an affected first degree relative, when compared to those without a positive family history (Farchione et al., 2002; Steingard et al., 2000). Duration and severity of illness could also affect the results. For example, another study on patients having a longer duration and milder severity of illness, along with a positive family history reported decreased Cho concentrations in the DLPFC (Caetano et al., 2005). Furthermore, as left hemisphere is more strongly believed to be affected in MDD (Farchione et al., 2002), right hemispheric metabolites have been shown to be normal (Michael et al., 2003b; Sözeri-Varma et al., 2013; O√?¬?uzhano√?¬?lu et al., 2014; Kusumakar et al., 2001).
Glutamate (Glu) Findings
Glu is the primary excitatory neurotransmitter of the brain. Glu, glutamine (Gln) and GABA are inseparable at low magnetic field strengths (Stanley, 2000; Ende et al., 2006; Maddock & Buonocore, 2012; Yildiz-Yesiloglu & Ankerst, 2006; Glitz et al., 2002; Malhi et al., 2002). High field strengths, short echo time, long acquisition times, or special editing methods are needed to differentiate these components apart (Ende et al., 2006; Maddock & Buonocore, 2012). 3.0T provides better separation for these metabolites as compared to 1.5T (Gussew et al., 2008). Many to date studies fail to separate out the individual constituents and refer to the calculated peak as Glx.
A number of studies, on pediatric, adult as well as elderly patient population, have recorded altered levels of metabolites in the glutamatergic system. Decreased Glx has been found in the ACC (Gussew et al., 2008; Rosenberg et al., 2004; Pfleiderer et al., 2003; Auer et al., 2000; Mirza et al., 2004), Amg (Michael et al., 2003b), dorsomedial PFC (DMPFC), VMPFC (Rosenberg et al., 2004), DLPFC (Michael et al., 2003a), and BG; left side more significant; of MDD patients (Ajilore et al., 2007). Controversial evidence, however, exists for the DLPFC, showing no significant difference between patients and normal people (Nery et al., 2009). A negative correlation has been found between Glu levels in VMPFC and the duration of illness (Portella et al., 2011). Decreased Glu levels in ACC of patients (Auer et al., 2000; Merkl, et al., 2010; Järnum et al. 2011; Rosenberg et al., 2005) further provide evidence towards the pathogenesis of depression. An 18.7% decrease in Glx has been recorded in the ACC (Rosenberg et al., 2004). The low Glx levels in DLPFC correlate negatively with the severity of depression (Michael et al., 2003a), whereas these reduced levels in ACC correlate negatively only with the severity of functional impairment measured by clinical global impression-severity scale (CGI-S) and not with depressive symptom score or the duration of illness (Mirza et al., 2004). Furthermore, the Glu levels in DLPFC have been shown to correlate negatively with the duration of illness and the number of episodes (Caetano et al., 2005). However, no correlation could be found between depression severity and Glx levels in DMPFC and VMPFC (Hasler et al., 2007). ECT has been successful in increasing the levels of Glx in ACC (Pfleiderer et al., 2003), Amg (Michael et al., 2003b) and DLPFC (Michael et al., 2003a). Glx levels are also significantly increased in OC after the administration of a selective serotonin reuptake inhibitor (SSRI) (Taylor et al., 2008); however there fails to be any demonstrable change in Glx or Glu level in the ACC (Taylor et al., 2010). The Glx/Cr ratio was also found higher in the OC of rMDD patients (Bhagwagar et al., 2007; Bhagwagar et al., 2008).
No difference has been found in the Glx concentration in HPC (Milne et al., 2009) or OC (Mirza et al., 2004) of patients and healthy matched-controls; however, the Glx/Cr and glutamine/ Cr (Gln/Cr) ratios have been found significantly decreased in HPC (Block et al., 2009), the Glu concentration and GABA/Glu ratio increased in OC of MDD patients (Sanacora et al. in 2004). One study noticed a decreased Gln, but normal Glu level in the pgACC (Walter et al., 2009). Glx/Cr and Glu/Cr were found significantly decreased in the pgACC of severely depressed patients than those with mild depression and healthy volunteers; while the Glu and Glx levels were significantly different in mildly depressed individuals and healthy matched-controls (Horn et al., 2010). In the pgACC, Glu correlates with negative BOLD responses and emotional intensity ratings in MDD patients (Walter et al., 2009).
These metabolite differences are worthy noting to understand the different aspects of disease development and progression. For example, a negative relationship has been found between the Glx/ GABA ratio and age of disease onset while measuring concentrations in the VMPFC of MDD patients (Hasler et al., 2005). Glx/GABA ratio has also been found significantly raised in the OC of treatmentresistant (Tr) MDD patients than healthy volunteers (Price et al., 2009).
Reduced number of glial cells found on post-mortem examinations of MDD patients (Ongür et al., 1998; Rajkowska et al., 2001), could be accountable for the decreased amount of Glx in the ACC, PFC, Amg, HPC, and the BG (Yildiz-Yesiloglu & Ankerst, 2006; Pfleiderer et al., 2003). This decrease in glutamatergic metabolites is thought to be state-dependent; improving with clinical improvement (Maddock & Buonocore, 2012).
Ketamine is a drug that acts on NMDA receptors and causes an increase in Glx and Gln, and has been used to treat depression successfully (Berman et al., 2000; Zarate et al., 2006). Pretreatment Glx/Glu in the DMPFC correlate negatively with depression symptoms as evidenced by change in Montgomery-Asberg Depression Rating Scale (MADRS) scores, and pretreatment Glu levels in VMPFC correlate positively with improved anxiety symptoms as noted by Hamilton Anxiety Scale (HAMA) scores (Salvadore et al., 2012). Studying the OC has, however, revealed that these changes seen in Glu, Gln and GABA are not significantly related to the improvement of depressive symptoms as evidenced by the decreased Beck Depression Inventory (BDI) and HDRS scores (Valentine et al., 2011). Total sleep deprivation (TSD) affects the metabolite levels in a similar fashion and can be used to improve depressive symptoms in some patients (Landsness et al., 2011). TSD leads to an increase in Glx and Gln in the DLPFC of male patients with major depression. Patients who experience early morning awakening and weight loss have also demonstrated an increase in Gln in the DLPFC after TSD (Murck et al., 2003).
In adults, eight out of 12 papers found reductions in glutamatergic metabolites in MDD (Block et al., 2009; Rosenberg et al., 2004; Auer et al., 2000; Ajilore et al., 2007; Merkl, et al., 2010; Hasler et al., 2007; Walter et al., 2009; Horn et al., 2010), while two found Glu to be increased in the OC (Sanacora et al. in 2004; Price et al., 2009), one found Glx to be normal in the DLPFC (Nery et al., 2009) and one study found Glx to be normal in the HPC (Milne et al., 2009). Two studies found decreased Glx in the ACC (Mirza et al., 2004; Rosenberg et al., 2004) and one study found normal Glx in the OC of children suffering from MDD (Mirza et al., 2004). Three studies noted decreased Glx in elderly MDD population, which responded well to ECT (Michael et al., 2003a; Michael et al., 2003b; Pfleiderer et al., 2003).
The altered milieu of glutamatergic metabolites has been consistently similar for most studies in this review. Since Glx represents an excitatory neurotransmitter, it appears fairly reasonable to believe its decreased amount in depressed patients, as noted by most of the studies. One study found increased GABA/Glu ratio in MDD patients (Sanacora et al. in 2004), implying the increase of inhibitory neurotransmitter GABA and the relative decrease of excitatory neurotransmitter Glu. Mirza et al. in 2004 found normal levels of Glx in the OC of MDD patients (Mirza et al., 2004). Similarly Sanacora et al. (2004) initially found higher levels of Glu in the OC of MDD patients, but on further confirmation of GABA/Glu ratio, they reported a significantly greater increase in GABA levels. Nery et al. in 2009 did not find altered Glx levels in the DLPFC of mildly depressed MDD patients (Nery et al., 2009); however, a significant correlation between disease severity and metabolite levels in DLPFC has been shown (Michael et al., 2003a).
Gamma Aminobutyric Acid (GABA) Findings
GABA is the primary inhibitory neurotransmitter of the brain. GABA levels are found to be significantly decreased in the OC (Sanacora et al., 2004; Sanacora et al., 1999) and DMPFC, including the pgACC (Hasler et al., 2007) of depression patients. A 52% reduction has been documented in the OC (Sanacora et al., 1999), with no significant relationship found between GABA levels and the severity of depression (Hasler et al., 2007; Hasler et al., 2007; Sanacora et al., 1999). It is also noteworthy that the GABA values in OC revealed significantly lower in patients with melancholic depression (P<0.001) and in those having depression with no subtype (P=0.002) when compared to healthy subjects, but not in patients with atypical depression (Sanacora et al., 2004). Comparing treatment resistant (Tr) MDD with non-Tr MDD and healthy volunteers, a significant reduction in GABA has been found in the OC, while a trend towards reduction noted in the ACC of Tr MDD (Price et al., 2009). Despite the earlier findings noted in pgACC, another study has shown normal GABA levels in this region in highly anhedonic MDD patients, and a correlation with negative BOLD responses in healthy adults (Walter et al., 2009). In a latest case-control cross-sectional study, anhedonic adolescents with MDD have significantly lower GABA in ACC as compared to healthy controls; with GABA levels negatively correlating to anhedonia scores (Gabbay et al., 2012). In the OC, a rise in GABA concentration after a successful course of SSRI (Sanacora et al., 2002), as well as a 34.5% increase in GABA/Cr ratio has been observed (Bhagwagar et al., 2004). Electroconvulsive therapy (ECT) also raised GABA levels in the OC of MDD sufferers, as well as decreased the severity of depression (Sanacora et al., 2003). Nevertheless, a significant change in OC metabolite levels has not been seen after cognitive behavioral therapy (CBT) (Sanacora et al. in 2006). Decreased GABA/Cr value is noted in the OC (Block et al., 2009; Bhagwagar et al., 2007) and ACC of recovered MDD (rMDD) patients (Bhagwagar et al., 2008). It is also interesting to find no difference in the GABA concentration, in both VMPFC and DLPFC, of MDD patients in remission and healthy subjects (Hasler et al., 2005). This might mean that brain GABA levels are only temporarily altered and do not represent markers for long-term disease detection.
In adults, eight out of 10 papers found decreased concentrations of GABA in MDD (Sanacora et al., 2004; Sanacora et al., 1999; Price et al., 2009; Sanacora et al., 2006; Hasler et al., 2007; Bhagwagar et al., 2008; Sanacora et al., 2003; Sanacora et al., 2002); whereas, one study focusing on patients with severe anhedonia reported normal GABA and decreased Gln levels in the pgACC (Walter et al., 2009). Low GABA was also found by one study on children (Gabbay et al., 2012). Rise in GABA have been noted after the use of SSRI as well as ECT (Sanacora et al., 2002; Sanacora et al., 2003; Bhagwagar et al., 2004), but not with CBT (Sanacora et al., 2006).
Myo-Inositol (mI) Findings
mI was originally defined as a marker of glial cells (Frey et al., 1998). However, later it has been shown to be present in high concentrations in certain types of neurons as well (Moore & Galloway, 2002). It is difficult to generalize the changes in mI observed in depression, due to several interplay factors which limit the results of currently available studies (Yildiz-Yesiloglu & Ankerst, 2006).
mI is raised in the DLPFC (Caetano et al., 2005), left medial temporal lobe (Venkatraman et al., 2009) and the HPC of MDD patients (Milne et al., 2009). mI/Cr ratio has also been found elevated in DLPFC (Kumar et al., 2002; Binesh et al., 2004) and BG (Chen et al., 2009), but decreased in PFC bilaterally (Gruber et al., 2003), the right frontal lobe (Frey et al., 1998), and ACC, with the decrease attributed to loss of glial tissue or changed metabolism (Järnum et al. 2011; Coupland et al., 2005). Other papers focusing on ACC show no significant difference in mI value in patients and matched-controls (Auer et al., 2000; Mirza et al., 2004). Since mI cannot be properly recorded using long echo time (Maddock & Buonocore, 2012), it is fair to rely on the findings of Auer et al. in 2000 and Mirza et al. in 2004, which detect normal values in the ACC. Similarly Nery et al. in 2009 showed no significant difference in the DLPFC (Nery et al., 2009). One study also found no difference in mI/Cr quantity in the caudate of patients and healthy subjects (Vythilingam et al., 2003). The mI/Cr has been shown to increase significantly in the DLPFC after treatment with an antidepressant (Kaymak et al., 2009). Furthermore, in the DLPFC of non-depressed, mI/Cr correlates positively with cognition, whereas such correlation does not exist in the depressed individuals (Elderkin-Thompson et al., 2004). A significant reduction in mI has been seen in the CSF of depressed patients (Barkai et al., 1978). Inositol intake has been shown to improve depression (Levine et al. 1995).
In adults, two studies noted normal mI in the DLPFC (Nery et al., 2009), one noted normal mI in the BG (Vythilingam et al., 2003), one noted normal mI in the ACC (Auer et al., 2000), one noted decreased mI in the ACC (Coupland et al., 2005), one noted decreased mI in the PFC (Gruber et al., 2003), one noted decreased mI in the right frontal lobe (Frey et al., 1998), and one noted increased mI in the HPC (Frey et al., 1998). In elder patients, three studies noted increased concentrations of mI (Kumar et al., 2002; Chen et al., 2009; Binesh et al., 2004). One study in children noted normal mI in the ACC (Mirza et al., 2004), whereas another study noted increased mI in the DLPFC (Caetano et al., 2005).
Creatine (Cr) Findings
In the normal human brain, the concentration of Cr or phosphocreatine (PCr) is considered quite uniform as compared to the other brain metabolites and thus, it is used as an internal standard for measuring other metabolites (Malhi et al., 2002; Maddock & Buonocore, 2012). However, the concentration of Cr varies considerably in conjunction with brain activity (Ke et al., 2002), and various other factors. Thus, it is not always a useful reference (Ross & Michaelis 1994). Further, Cr and PCr are primarily manufactured in the liver and kidney. An organ dysfunction invariably lowers the amount of these metabolites measured in the brain (Ende et al., 2006). This could account for some inter-study differences in findings of other metabolites.
Kato et al. (1992) have studied changes in phosphorus concentration in the frontal cortex. They have found significantly higher phosphomonoester (PME) in bipolar patients in the depressive state as compared to normal individuals. PCr turned out to be lower in severely depressed individuals when comparing them to mildly ill ones (Kato et al., 1992). The significant increase in PME has been confirmed later through another study which also documented decreased ATP (Volz et al., 1998). Further, a significant increase in PCr concentration along with a 56% decrease in Children’s Depression Rating Scale-Revised (CDRS-R) score has been demonstrated in adolescent patients after treatment with oral creatine for 8 weeks (Kondo et al., 2011b). ATP levels have also been found significantly reduced in the BG of MDD patients (Moore et al., 1997).
Cr concentration has been found higher in PFC (Gruber et al., 2003) and left caudate (Gabbay et al., 2007), but lower in ACC (Mirza et al., 2004) of MDD patients. A preliminary effect of gender has been found on PCr+Cr in the DLPFC. Male patients have lower value as compared to healthy male subjects; whereas female patients have higher value when compared to healthy female subjects (Nery et al., 2009). The effect of TSD on Cr has also been studied and it has shown to slightly increase this metabolite in DLPFC (Murck et al., 2009).
The current research is limited to make conclusions with conviction about the energy status of different brain areas in depression. According to Fattal et al. (2007), 54 % of people with mitochondrial disorders suffer from MDD. Several other studies support this finding. Low energy levels are reported in the BG and frontal cortex. Low level of Cr measured in the ACC, point towards impaired brain function or structure. 31P MRS has a strong role in studying the in-vivo patterns of energy metabolism and reveal insights.
Weakness, Future Perspectives and Conclusion
The information gathered so far is very useful in understanding depression. Broadly summarizing the results we found that Glu, Glx and GABA are decreased, NAA and mI remain unchanged, and Cho concentration varies according to area of voxel in MDD.
Our knowledge is, however, restricted by a number of variables which limit the validity of each study. It is important to look at these aspects so that future researches can take them into account and allow for maximum validity.
Most studies utilize DSM-IV criteria diagnosed MDD patients as study subjects. A few older ones using DSM-III make comparison difficult. Another important variable which makes comparison difficult is the small number of test subjects, making the power small. Although the use of ratios in interpreting concentration differences control for partial volume averaging, it decreases the sensitivity of findings. This altered sensitivity makes it difficult in understanding contradicting results of different research designs and, hence, some findings need to be analyzed and revalidated through further exploration.
Patient populations from all age groups have been studied, but the depth and amount of work done over one group varies widely from one another. For example only a handful of articles note changes in the elderly and those who have achieved full remission. Depression can be a lot worse in old age and requires due attention. There are very few publications on children with depression, which use 3.0T scanners. Because of the continuum of pathology found between younger and older age, a more thorough evaluation of childhood depression can help understand the disease better. Comparison between chronic and less chronic (acute) illness is only superficial.
Use of 1.5T scanners by majority of the authors further limits the sensitivity of the test. Recently 3.0 T has come into vogue and higher magnetic strengths can prove a very sophisticated means of increasing credibility of the results. In the research setting, highest magnetic strengths, such as 7.0 T, help better resolution of those metabolites which are in small concentrations. Lower strengths like 3.0 T, can prove economical and beneficial in the clinical setting; however care will have to be exercised in maintaining a fine balance when correlating 7.0 T deductions in research setting to 3.0 T findings in the clinical scenario.
Voxel placement and voxel size also do not overlap exactly between different studies focusing on the same brain region. This could be of significant importance in interpreting the results and drawing conclusions thereof. A much tighter control of voxel size and area definition might have to be exercised for comparison.
PET/MRI combination has been used by some authors but more work is needed in order to understand the pathophysiology of the illness in depth. Combining spectroscopic techniques with functional MRI increases the sensitivity in diagnosing depression. PET is a reliable method of assessing regional blood flow.
The neurobiological basis for the action of antidepressants used in MDD is poorly understood (Brambilla et al., 2003; Manji et al., 2003; Brambilla et al., 2005b; Sala et al., 2006; Sala et al., 2009; Verdoux et al., 2009). Some studies have delineated a few important effects of antidepressants, but we believe that the work is limited. With more extensive scrutinizing, it might be possible to suggest appropriate therapy, for example, antidepressants or ECT or CBT, for different patient populations. Also, a uniform battery of neuropsychological tests can prove very helpful in standardizing the variables.
In conclusion, MRS and MRSI are safe and useful techniques both in research and clinical setting for detecting disease onset, monitoring progression, instituting treatment and ensuring good prognosis through longitudinal follow-up.
References
- Shim RS, Baltrus P, Ye J, Rust G (2011) Prevalence, treatment, and control of depressive symptoms in the united states: results from the national health and nutrition examination survey (NHANES), 2005-2008. J Am Board Fam Med 24(1): 33-38
- WHO.int [homepage on the internet] World Health Organization: The world health report—primary health care (now more than ever); 2008. Available from: http://www.who.int/whr/2008/en/.
- Stewart W, Ricci J, Chee E, Hahn SR, Morganstein D (2003) Cost of lost productive work time among US workers with depression. JAMA 289(23): 3135-3144
- Bernal M, Haro JM, Bernert S, Brugha T, de Graaf R, et al. (2007) Risk factors for suicidality in Europe: results from the ESEMED study. J Affect Disord 101(1-3): 27-34
- Weissman MM, Olfson M (1995) Depression in women: implications for health care research. Science 269(5225): 799–801
- Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE (2005) Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 62(6): 617-627
- Soleimani L, Lapidus KA, Iosifescu DV (2011) Diagnosis and treatment of major depressive disorder. NeurolClin 29(1): 177-193
- Lewinsohn PM, Fenn DS, Stanton AK, Franklin J (1986) Relation of age at onset to duration of episode in unipolar depression. Psychol Aging 1(1): 63-68
- Lewinsohn PM, Hops H, Roberts RE, Seeley JR, Andrews JA (1993) Adolescent psychopathology: I. Prevalence and incidence of depression and other DSM-III-R disorders in high school students. J AbnormPsychol 102(1): 133-144
- Kessler RC, McGonagle KA, Nelson CB, Hughes M, Swartz M, et al. (1994) Sex and depression in the National Comorbidity Survey. II: Cohort effects. J Affect Disord 30(1): 15-26
- Lewinsohn PM, Rohde P, Seeley JR, Klein DN, Gotlib IH (2000) Natural course of adolescent major depressive disorder in a community sample: Predictors of recurrence in young adults. Am J Psychiatry 157(10): 1584-1591
- Bruce ML, Leaf PJ (1989) Psychiatric disorders and 15-month mortality in a community sample of older adults. Am J Public Health 79(6): 727-730
- Agatisa PK, Matthews KA, Bromberger JT, Edmundowicz D, Chang YF, et al. (2005) Coronary and aortic calcification in women with a history of major depression. Arch Intern Med 165(11): 1229-1236
- Alboni P, Favaron E, Paparella N, Sciammarella M, Pedaci M (2008) Is there an association between depression and cardiovascular mortality or sudden death? J Cardiovasc Med (Hagerstown) 9: 356-362
- Fan A, Strine T, Jiles R, Mokdad AH (2008) Depression and anxiety associated with cardiovascular disease among persons aged 45 years and older in 38 states of the United States, 2006. Prev Med 46: 445-450
- Grandy S, Chapman R, Fox K (2008) Quality of life and depression of people living with type 2 diabetes mellitus and those at low and high risk for type 2 diabetes: findings from the Study to Help Improve Early Evaluation and Management of Risk Factors Leading to Diabetes (SHIELD). Int J ClinPract 2: 562-568
- Tadic A, Wagner S, Gorbulev S, Dahmen N, Hiemke C, et al. (2011) Peripheral blood and neuropsychological markers for the onset of action of antidepressant drugs in patients with Major Depressive Disorder. BMC Psychiatry 11(1): 16
- Campbell S, Marriott M, Nahmias C, MacQueen GM (2004) Lower hippocampal volume in patients suffering from depression: a meta-analysis. Am J Psychiatry 161: 598-607
- Videbech P, Ravnkilde B (2004) Hippocampal volume and depression: a meta-analysis of MRI studies. Am J Psychiatry 161: 1957-1966
- McKinnon MC, Yusel K, Nazarov A, MacQueen GM (2009) A meta-analysis examining clinical predictors of hippocampal volume in patients with major depressive disorder.J Psychiatry Neurosci 34: 41-54
- Amico F, Meisenzahl E, Koutsouleris N, Reiser M, Moller HJ, et al. (2011) Structural MRI correlates for vulnerability and resilience to major depressive disorder. J Psychiatry Neurosci 36(1): 15-22
- Elderkin-Thompson V, Kumar A, Bilker WB, Dunkin JJ, Mintz J, et al. (2003) Neuropsychological deficits among patients with late-onset minor and major depression. Arch ClinNeuropsychol 18(5): 529-549
- Caetano SC, Sassi R, Brambilla P, Harenski K, Nicoletti M, et al. (2001) MRI study of thalamic volumes in bipolar and unipolar patients and healthy individuals. Psychiatry Res 108(3): 161-168
- Brambilla P, Barale F, Caverzasi E, Soares JC (2002) Anatomical MRI findings in mood and anxiety disorders. EpidemiolPsichiatrSoc 11(2): 88-99
- Brambilla P, Nicoletti MA, Harenski K, Sassi RB, Mallinger AG, et al. (2002) Anatomical MRI study of subgenual prefrontal cortex in bipolar and unipolar subjects. Neuropsychopharmacology 27(5): 792-799
- Lacerda AL, Nicoletti MA, Brambilla P, Sassi RB, Mallinger AG, et al. (2003) Anatomical MRI study of basal ganglia in major depressive disorder. Psychiatry Res 124(3): 129-140
- Brambilla P, Nicoletti M, Sassi RB, Mallinger AG, Frank E, et al. (2004) Corpus callosum signal intensity in patients with bipolar and unipolar disorder. J NeurolNeurosurg Psychiatry 75(2): 221-225
- Lacerda AL, Brambilla P, Sassi RB, Nicoletti MA, Mallinger AG, et al. (2005) Anatomical MRI study of corpus callosum in unipolar depression. J Psychiatr Res 39(4): 347-354
- Bench CJ, Friston KJ, Brown RG, Scott LC, Frackowiak RS, et al. (1992) The anatomy of melancholia–focal abnormalities of cerebral blood flow in major depression. Psychol Med 22(3): 607-615
- Dolan RJ, Bench CJ, Brown RG, Scott LC, Frackowiak RS (1994) Neuropsychological dysfunction in depression: the relationship to regional cerebral blood flow. Psychol Med 24(4): 849-857
- Bremner JD, Innis RB, Salomon RM, Staib LH, Ng CK, et al. (1997) Positron emission tomography measurement of cerebral metabolic correlates of tryptophan depletion-induced depressive relapse. Arch Gen Psychiatry 54(4): 364-374
- Vollmert C, Tost H, Brassen S, Jatzko A, Braus DF (2004) Depression and modern neuroimaging. FortschrNeurolPsychiatr 72(8): 435-445
- Ho AP, Gillin JC, Buchsbaum MS, Wu JC, Abel L, et al. (1996) Brain glucose metabolism during non-rapid eye movement sleep in major depression. A positron emission tomography study. Arch Gen Psychiatry 53(7): 645-652
- Mayberg HS, Liotti M, Brannan SK, McGinnis S, Mahurin RK, et al. (1999) Reciprocal limbic-cortical function and negative mood: converging PET findings in depression and normal sadness. Am J Psychiatry 156(5): 675-682
- Hurwitz TA, Clark C, Murphy E, Klonoff H, Martin WR, et al. (1990) Regional cerebral glucose metabolism in major depressive disorder. Can J Psychiatry 35(8): 684-688
- Lesser IM, Mena I, Boone KB, Miller BL, Mehringer CM, et al. (1994) Reduction of cerebral blood flow in older depressed patients. Arch Gen Psychiatry 51(9): 677-686
- Mozley PD, Hornig-Rohan M, Woda AM, Kim HJ, Alavi A, et al. (1996) Cerebral HMPAO SPECT in patients with major depression and healthy volunteers. ProgNeuropsychopharmacolBiol Psychiatry 20(3): 443-458
- Walter M, Henning A, Grimm S, Schulte RF, Beck J, et al. (2009) The relationship between aberrant neuronal activation in the pregenual anterior cingulate, altered glutamatergic metabolism, and anhedonia in major depression. Arch Gen Psychiatry 66(5): 478-486
- Urenjak J, Williams SR, Gadian DG, Noble M (1993) Proton nuclear magnetic resonance spectroscopy unambiguously identifies different neural cell types. J Neurosci 13(3): 981-989
- Chang L, Cloak CC, Ernst T (2003) Magnetic resonance spectroscopy studies of GABA in neuropsychiatric disorders. J Clin Psychiatry 64(3): 7-14
- Regier DA, Narrow WE, Kuhl EA, Kupfer DJ (2009) The conceptual development of DSM-V. Am J Psychiatry 166(6): 645-650
- Horn DI, Yu C, Steiner J, Buchmann J, Kaufmann J, et al. (2010) Glutamatergic and resting-state functional connectivity correlates of severity in major depression - the role of pregenual anterior cingulate cortex and anterior insula. Front SystNeurosci 4: 33
- Stanley JA, Pettegrew JW, Keshavan MS (2000) Magnetic resonance spectroscopy in schizophrenia: methodological issues and findings-part I. Biol Psychiatry 48(5): 357-368
- Stanley JA (2002) In vivo magnetic resonance spectroscopy and its application to neuropsychiatric disorders. Can J Psychiatry 47(4): 315-326
- Kondo DG, Hellem TL, Sung YH, Kim N, Jeong EK, et al. (2011a) Review: magnetic resonance spectroscopy studies of pediatric major depressive disorder. Depress Res Treat 2011: 650450
- Kumar A, Thomas A, Lavretsky H, Yue K, Huda A, et al. (2002) Frontal white matter biochemical abnormalities in late-life major depression detected with proton magnetic resonance spectroscopy. Am J Psychiatry 159(4): 630-636
- Charles HC, Lazeyras F, Krishnan KR, Boyko OB, Payne M, et al. (1994) Brain choline in depression: in vivo detection of potential pharmacodynamic effects of antidepressant therapy using hydrogen localized spectroscopy. ProgNeuropsychopharmacolBiol Psychiatry 18(7): 1121-1127
- Sonawalla SB, Renshaw PF, Moore CM, Alpert JE, Nierenberg AA, et al. (1999) Compounds containing cytosolic choline in the basal ganglia: a potential biological marker of true drug response to fluoxetine. Am J Psychiatry 156(10): 1638-1640
- Ende G, Braus DF, Walter S, Weber-Fahr W, Henn FA (2000) The hippocampus in patients treated with electroconvulsive therapy: a proton magnetic resonance spectroscopic imaging study. Arch Gen Psychiatry 57(10): 937-943
- Sanacora G, Mason GF, Rothman DL, Krystal JH (2002) Increased occipital cortex GABA concentrations in depressed patients after therapy with selective serotonin reuptake inhibitors. Am J Psychiatry 159(4): 663-665
- Michael N, Erfurth A, Ohrmann P, Arolt V, Heindel W, et al. (2003a) Metabolic changes within the left dorsolateral prefrontal cortex occurring with electroconvulsive therapy in patients with treatment resistant unipolar depression. Psychol Med 33(7): 1277-1284
- Michael N, Erfurth A, Ohrmann P, Arolt V, Heindel W, et al. (2003b) Neurotrophic effects of electroconvulsive therapy: a proton magnetic resonance study of the left amygdalar region in patients with treatment-resistant depression. Neuropsychopharmacology 28(4): 720-725
- Pfleiderer B, Michael N, Erfurth A, Ohrmann P, Hofmann U, et al. (2003) Effective electroconvulsive therapy reverses glutamate/glutamine deficit in the left anterior cingulum of unipolar depressed patients. Psychiatry Res 122(3): 185-192
- Sanacora G, Mason GF, Rothman DL, Hyder F, Ciarcia JJ, et al. (2003) Increased cortical GABA concentrations in depressed patients receiving ECT. Am J Psychiatry 160(3): 577-579
- Bhagwagar Z, Wylezinska M, Taylor M, Jezzard P, Matthews PM, et al. (2004) Increased brain GABA concentrations following acute administration of a selective serotonin reuptake inhibitor. Am J Psychiatry 161(2): 368-370
- Gonul AS, Kitis O, Ozan E, Akdeniz F, Eker C, et al. (2006) The effect of antidepressant treatment on N-acetyl aspartate levels of medial frontal cortex in drug-free depressed patients. ProgNeuropsychopharmacolBiol Psychiatry 30(1): 120-125
- Ajilore O, Haroon E, Kumaran S, Darwin C, Binesh N, et al. (2007) Measurement of brain metabolites in patients with type 2 diabetes and major depression using proton magnetic resonance spectroscopy. Neuropsychopharmacology 32(6): 1224-1231
- Merkl A, Schubert F, Quante A, Luborzewski A, Brakemeier EL, et al. (2010) Abnormal cingulate and prefrontal cortical neurochemistry in major depression after electroconvulsive therapy. Biol Psychiatry 69(8): 772-779
- Ende G, Demirakca T, Tost H (2006) The biochemistry of dysfunctional emotions: proton MR spectroscopic findings in major depressive disorder. Prog Brain Res 156: 481-501
- Maddock RJ, Buonocore MH (2012) MR Spectroscopic Studies of the Brain in Psychiatric Disorders.Curr Top BehavNeurosci 11: 199-251
- Moffett JR, Ross B, Arun P, Madhavarao CN, Namboodiri AM (2007) N-Acetylaspartate in the CNS: from neurodiagnostics to neurobiology.ProgNeurobiol 81(2): 89-131
- MacMaster FP, Moore GJ, Russell A, Mirza Y, Taormina SP, et al. (2008) Medial temporal N-acetyl-aspartate in pediatric major depression. Psychiatry Res 164(1): 86-89
- Olvera RL, Caetano SC, Stanley JA, Chen HH, Nicoletti M, et al. (2010) Reduced medial prefrontal N-acetyl-aspartate levels in pediatric major depressive disorder: a multi-voxel in vivo(1)H spectroscopy study. Psychiatry Res 184(2): 71-76
- Järnum H, Eskildsen SF, Steffensen EG, Lundbye-Christensen S, Simonsen CW, et al. (2011) Longitudinal MRI study of cortical thickness, perfusion, and metabolite levels in major depressive disorder.ActaPsychiatrScand 124(6): 435-446
- Venkatraman TN, Krishnan RR, Steffens DC, Song AW, Taylor WD (2009) Biochemical abnormalities of the medial temporal lobe and medial prefrontal cortex in late-life depression. Psychiatry Res 172(1): 49-54
- Vythilingam M, Charles HC, Tupler LA, Blitchington T, Kelly L, et al. (2003) Focal and lateralized subcortical abnormalities in unipolar major depressive disorder: an automated multivoxel proton magnetic resonance spectroscopy study. Biol Psychiatry 54(7): 744-750
- Chen CS, Chiang IC, Li CW, Lin WC, Lu CY, et al. (2009) Proton magnetic resonance spectroscopy of late-life major depressive disorder. Psychiatry Res 172(3): 210-214
- Wang Y, Jia Y, Xu G, Ling X, Liu S, et al. (2012) Frontal white matter biochemical abnormalities in first-episode, treatment-naive patients with major depressive disorder: a proton magnetic resonance spectroscopy study. J Affect Disord 136(3): 620-626
- Gruber S, Frey R, Mlynárik V, Stadlbauer A, Heiden A, et al. (2003) Quantification of metabolic differences in the frontal brain of depressive patients and controls obtained by 1H-MRS at 3 Tesla. Invest Radiol 38(7): 403-408
- Sözeri-Varma G, Kalkan-Oguzhanoglu N, Efe M, Kiroglu Y, Duman T (2013) Neurochemical metabolites in prefrontal cortex in patients with mild/moderate levels in first-episode depression. Neuropsychiatr Dis Treat 9: 1053-1059
- Coupland NJ, Ogilvie CJ, Hegadoren KM, Seres P, Hanstock CC, et al. (2005) Decreased prefrontal myo-inositol in major depressive disorder. Biol Psychiatry 57(12): 1526-1534
- Oguzhanoglu NK, Sözeri-Varma G, Karadag F, Tümkaya S, Efe M, et al. (2014) Prefrontal Cortex Neurochemical Metabolite Levels in Major Depression and the Effects of Treatment: An HMRS Study. Turk PsikiyatriDerg 25(2): 75-83
- Kaymak SU, Demir B, Oguz KK, Sentürk S, Ulug B (2009) Antidepressant effect detected on proton magnetic resonance spectroscopy in drug-naïve female patients with first-episode major depression. Psychiatry ClinNeurosci 63(3): 350-356
- Nery FG, Stanley JA, Chen HH, Hatch JP, Nicoletti MA, et al. (2009) Normal metabolite levels in the left dorsolateral prefrontal cortex of unmedicated major depressive disorder patients: a single voxel (1)H spectroscopy study. Psychiatry Res 174(3): 177-183
- Block W, Träber F, von Widdern O, Metten M, Schild H, et al. (2009) Proton MR spectroscopy of the hippocampus at 3 T in patients with unipolar major depressive disorder: correlates and predictors of treatment response. Int J Neuropsychopharmacol 12(3): 415-422
- Obergriesser T, Ende G, Braus DF, Henn FA (2003) Long-term follow-up of magnetic resonance-detectable choline signal changes in the hippocampus of patients treated with electroconvulsive therapy. J Clin Psychiatry 64(7): 775-780
- Renshaw PF, Lafer B, Babb SM, Fava M, Stoll AL, et al. (1997) Basal ganglia choline levels in depression and response to fluoxetine treatment: an in vivo proton magnetic resonance spectroscopy study. Biol Psychiatry 41(8): 837-843
- Bhagwagar Z, Wylezinska M, Jezzard P, Evans J, Ashworth F, et al. (2007) Reduction in occipital cortex gamma-aminobutyric acid concentrations in medication-free recovered unipolar depressed and bipolar subjects. Biol Psychiatry 61(6): 806-812
- Murata T, Kimura H, Omori M, Kado H, Kosaka H, et al. (2001) MRI white matter hyperintensities, (1)H-MR spectroscopy and cognitive function in geriatric depression: a comparison of early- and late-onset cases. Int J Geriatr Psychiatry 16(12): 1129-1135
- Brambilla P, Stanley JA, Nicoletti MA, Sassi RB, Mallinger AG, et al. (2005) 1H Magnetic resonance spectroscopy study of dorsolateral prefrontal cortex in unipolar mood disorder patients. Psychiatry Res 138(2): 131-139
- Portella MJ, de Diego-Adeliño J, Gómez-Ansón B, Morgan-Ferrando R, Vives Y, et al. (2011) Ventromedial prefrontal spectroscopic abnormalities over the course of depression: A comparison among first episode, remitted recurrent and chronic patients. J Psychiatr Res 45(4): 427-434
- Yildiz-Yesiloglu A, Ankerst DP (2006) Review of 1H magnetic resonance spectroscopy findings in major depressive disorder: a meta-analysis. Psychiatry Res 147(1): 1-25
- Boulanger Y, Labelle M, Khiat A (2000) Role of phospholipase A(2) on the variations of the choline signal intensity observed by 1H magnetic resonance spectroscopy in brain diseases. Brain Res Brain Res Rev 33(2-3): 380-389
- Kusumakar V, MacMaster FP, Gates L, Sparkes SJ, Khan SC (2001) Left medial temporal cytosolic choline in early onset depression. Can J Psychiatry 46(10): 959-964
- Glitz DA, Manji HK, Moore GJ (2002) Mood disorders: treatment-induced changes in brain neurochemistry and structure. SeminClin Neuropsychiatry 7(4): 269-280
- Moore GJ, Galloway MP (2002) Magnetic resonance spectroscopy: neurochemistry and treatment effects in affective disorders. Psychopharmacol Bull 36(2): 5-23
- Yue Q, Shibata Y, Isobe T, Anno I, Kawamura H, et al. (2009) Absolute choline concentration measured by quantitative proton MR spectroscopy correlates with cell density in meningioma. Neuroradiology 51(1): 61-67
- Geddes JW, Panchalingam K, Keller JN, Pettegrew JW (1997) Elevated phosphocholine and phosphatidylcholine following rat entorhinal cortex lesions.Neurobiol Aging 18(3): 305-308
- Danielsen ER, Ross B (1999) Magnetic resonance spectroscopy diagnosis of neurological diseases: MR Spectroscopy of the Brain. Marcel Dekker, New York
- Hamakawa H, Kato T, Murashita J, Kato N (1998) Quantitative proton magnetic resonance spectroscopy of the basal ganglia in patients with affective disorders. Eur Arch Psychiatry ClinNeurosci 248(1): 53-58
- Ende G, Demirakca T, Walter S, Wokrina T, Sartorius A, et al. (2007) Subcortical and medial temporal MR-detectable metabolite abnormalities in unipolar major depression. Eur Arch Psychiatry ClinNeurosci 257(1): 36-39
- Gabbay V, Hess DA, Liu S, Babb JS, Klein RG, et al. (2007) Lateralized caudate metabolic abnormalities in adolescent major depressive disorder: a proton MR spectroscopy study. Am J Psychiatry 164(12): 1881-1889
- Farchione TR, Moore GJ, Rosenberg DR (2002) Proton magnetic resonance spectroscopic imaging in pediatric major depression.Biol Psychiatry 52(2): 86-92
- Smith EA, Russell A, Lorch E, Banerjee SP, Rose M, et al. (2003) Increased medial thalamic choline found in pediatric patients with obsessive-compulsive disorder versus major depression or healthy control subjects: a magnetic resonance spectroscopy study. Biol Psychiatry 54(12): 1399-1405
- Auer DP, Putz B, Kraft E, Lipinski B, Schill J, et al. (2000) Reduced glutamate in the anterior cingulate cortex in depression: an in vivo proton magnetic resonance spectroscopy study. Biol Psychiatry 47(4): 305-313
- Mirza Y, Tang J, Russell A, Banerjee SP, Bhandari R, et al. (2004) Reduced anterior cingulate cortex glutamatergic concentrations in childhood major depression. J Am Acad Child Adolesc Psychiatry 43(3): 341-348
- Steingard RJ, Yurgelun-Todd DA, Hennen J, Moore JC, Moore CM, et al. (2000) Increased orbitofrontal cortex levels of choline in depressed adolescents as detected by in vivo proton magnetic resonance spectroscopy. Biol Psychiatry 48(11): 1053-1061
- Kaufman MJ, Henry ME, Frederick B, Hennen J, Villafuerte RA, et al. (2003) Selective serotonin reuptake inhibitor discontinuation syndrome is associated with a rostral anterior cingulate choline metabolite decrease: a proton magnetic resonance spectroscopic imaging study. Biol Psychiatry 54(5): 534-539
- Elderkin-Thompson V, Thomas MA, Binesh N, Mintz J, Haroon E, et al. (2004) Brain metabolites and cognitive function among older depressed and healthy individuals using 2D MR spectroscopy. Neuropsychopharmacology 29(12): 2251-2257
- MacMaster FP, Kusumakar V (2006) Choline in pediatric depression.Mcgill J Med 9(1): 24-27
- Milne A, MacQueen GM, Yucel K, Soreni N, Hall GB (2009) Hippocampal metabolic abnormalities at first onset and with recurrent episodes of a major depressive disorder: a proton magnetic resonance spectroscopy study. Neuroimage 47(1): 36-41
- Caetano SC, Fonseca M, Olvera RL, Nicoletti M, Hatch JP, et al. (2005) Proton spectroscopy study of the left dorsolateral prefrontal cortex in pediatric depressed patients. Neuroscilett 384(3): 321-326
- Hercher C, Turecki G, Mechawar N (2009) Through the looking glass: examining neuroanatomical evidence for cellular alterations in major depression. J Psychiatr Res 43(11): 947-961
- Catena-Dell'Osso M, Bellantuono C, Consoli G, Baroni S, Rotella F, et al. (2011) Inflammatory and neurodegenerative pathways in depression: a new avenue for antidepressant development? Curr Med Chem 18(2): 245-255
- Kurz K, Schroecksnadel S, Weiss G, Fuchs D (2011) Association between increased tryptophan degradation and depression in cancer patients. CurrOpinClinNutrMetab Care 14(1): 49-56
- Maes M (2011) Depression is an inflammatory disease, but cell-mediated immune activation is the key component of depression. ProgNeuropsychopharmacolBiol Psychiatry 35(3): 664-675
- Müller N, Myint AM, Schwarz MJ (2011) Inflammatory biomarkers and depression. Neurotox Res 19(2): 308-318
- Gabbay V, Liebes L, Katz Y, Liu S, Mendoza S, et al. (2010) The kynurenine pathway in adolescent depression: preliminary findings from a proton MR spectroscopy study. ProgNeuropsychopharmacolBiol Psychiatry 34(1): 37-44
- Malhi GS, Valenzuela M, Wen W, Sachdev P (2002) Magnetic resonance spectroscopy and its applications in psychiatry. Aust N Z J Psychiatry 36(1): 31-43
- Gussew A, Rzanny R, Scholle HC, Kaiser WA, Reichenbach JR (2008) Quantitation of glutamate in the brain by using MR proton spectroscopy at 1.5 T and 3 T. Rofo 180(8): 722-732
- Rosenberg DR, Mirza Y, Russell A, Tang J, Smith JM, et al. (2004) Reduced anterior cingulate glutamatergic concentrations in childhood OCD and major depression versus healthy controls. J Am Acad Child Adolesc Psychiatry 43(9): 1146-1153
- Rosenberg DR, Macmaster FP, Mirza Y, Smith JM, Easter PC, et al. (2005) Reduced anterior cingulate glutamate in pediatric major depression: a magnetic resonance spectroscopy study. Biol Psychiatry 58(9): 700-704
- Hasler G, van der Veen JW, Tumonis T, Meyers N, Shen J, et al. (2007) Reduced prefrontal glutamate/glutamine and gamma-aminobutyric acid levels in major depression determined using proton magnetic resonance spectroscopy. Arch Gen Psychiatry 64(2): 193-200
- Taylor M, Murphy SE, Selvaraj S, Wylezinkska M, Jezzard P, et al. (2008) Differential effects of citalopram and reboxetine on cortical Glx measured with proton MR spectroscopy. J Psychopharmacol 22(5): 473-476
- Taylor MJ, Norbury R, Murphy S, Rudebeck S, Jezzard P, et al. (2010) Lack of effect of citalopram on magnetic resonance spectroscopy measures of glutamate and glutamine in frontal cortex of healthy volunteers. J Psychopharmacol 24(8): 1217-1221
- Bhagwagar Z, Wylezinska M, Jezzard P, Evans J, Boorman E, et al. (2008) Low GABA concentrations in occipital cortex and anterior cingulate cortex in medication-free, recovered depressed patients. Int J Neuropsychopharmacol 11(2): 255-260
- Sanacora G, Gueorguieva R, Epperson CN, Wu YT, Appel M, et al. (2004) Subtype-specific alterations of gamma-aminobutyric acid and glutamate in patients with major depression. Arch Gen Psychiatry 61(7): 705-713
- Hasler G, Neumeister A, van der Veen JW, Tumonis T, Bain EE, et al. (2005) Normal prefrontal gamma-aminobutyric acid levels in remitted depressed subjects determined by proton magnetic resonance spectroscopy. Biol Psychiatry 58(12): 969-973
- Price RB, Shungu DC, Mao X, Nestadt P, Kelly C, et al. (2009) Amino acid neurotransmitters assessed by proton magnetic resonance spectroscopy: relationship to treatment resistance in major depressive disorder. Biol Psychiatry 65(9): 792-800
- Ongür D, Drevets WC, Price JL (1998) Glial reduction in the subgenual prefrontal cortex in mood disorders.ProcNatlAcadSci U S A 95(22): 13290-13295
- Rajkowska G, Halaris A, Selemon LD (2001) Reductions in neuronal and glial density characterize the dorsolateral prefrontal cortex in bipolar disorder. Biol Psychiatry 49(9): 741-752
- Berman RM, Cappiello A, Anand A, Oren DA, Heninger GR, et al. (2000) Antidepressant effects of ketamine in depressed patients. Biol Psychiatry 47(4): 351-354
- Zarate CA Jr, Singh JB, Carlson PJ, Brutsche NE, Ameli R, et al. (2006) A randomized trial of an N-methyl-D-aspartate antagonist in treatment-resistant major depression. Arch Gen Psychiatry 63(8): 856-864
- Salvadore G, van der Veen JW, Zhang Y, Marenco S, Machado-Vieira R, et al. (2012) An investigation of amino-acid neurotransmitters as potential predictors of clinical improvement to ketamine in depression. Int J Neuropsychopharmacol 15(8): 1063-1072
- Valentine GW, Mason GF, Gomez R, Fasula M, Watzl J, et al. (2011) The antidepressant effect of ketamine is not associated with changes in occipital amino acid neurotransmitter content as measured by [(1)H]-MRS. Psychiatry Res 191(2): 122-127
- Landsness EC, Goldstein MR, Peterson MJ, Tononi G, Benca RM (2011) Antidepressant effects of selective slow wave sleep deprivation in major depression: A high-density EEG investigation. J Psychiatr Res 45(8): 1019-1026
- Murck H, Schubert MI, Schmid D, Schüssler P, Steiger A, et al. (2009) The glutamatergic system and its relation to the clinical effect of therapeutic-sleep deprivation in depression - an MR spectroscopy study. J Psychiatr Res 43(3): 175-180
- Sanacora G, Mason GF, Rothman DL, Behar KL, Hyder F, et al. (1999) Reduced cortical gamma-aminobutyric acid levels in depressed patients determined by proton magnetic resonance spectroscopy. Arch Gen Psychiatry 56(11): 1043-1047
- Gabbay V, Mao X, Klein RG, Ely BA, Babb JS, et al. (2012) Anterior Cingulate Cortex γ-Aminobutyric Acid in Depressed Adolescents: Relationship to Anhedonia. Arch Gen Psychiatry 69(2): 139-149
- Sanacora G, Fenton LR, Fasula MK, Rothman DL, Levin Y, et al. (2006) Cortical gamma-aminobutyric acid concentrations in depressed patients receiving cognitive behavioral therapy. Biol Psychiatry 59(3): 284-286
- Frey R, Metzler D, Fischer P, Heiden A, Scharfetter J, et al. (1998) Myo-inositol in depressive and healthy subjects determined by frontal 1H-magnetic resonance spectroscopy at 1.5 tesla. J Psychiatr Res 32(6): 411-420
- Binesh N, Kumar A, Hwang S, Mintz J, Thomas MA (2004) Neurochemistry of late-life major depression: a pilot two-dimensional MR spectroscopic study. J MagnReson Imaging 20(6): 1039-1045
- Barkai AI, Dunner DL, Gross HA, Mayo P, Fieve RR (1978) Reduced myo-inositol levels in cerebrospinal fluid from patients with affective disorder. Biol Psychiatry 13(1): 65-72
- Levine J, Barak Y, Gonzalves M, Szor H, Elizur A, et al. (1995) Double-blind, controlled trial of inositol treatment of depression. Am J Psychiatry 152(5): 792-794
- Ke Y, Cohen BM, Lowen S, Hirashima F, Nassar L, et al. (2002) Biexponential transverse relaxation (T(2)) of the proton MRS creatine resonance in human brain. MagnReson Med 47(2): 232-238
- Ross B, Michaelis T (1994) Clinical applications of magnetic resonance spectroscopy. MagnReson Q 10(4): 191-247
- Kato T, Takahashi S, Shioiri T, Inubushi T (1992) Brain phosphorous metabolism in depressive disorders detected by phosphorus-31 magnetic resonance spectroscopy. J Affect Disord 26(4): 223-230
- Volz HP, Rzanny R, Riehemann S, May S, Hegewald H, et al. (1998) 31P magnetic resonance spectroscopy in the frontal lobe of major depressed patients. Eur Arch Psychiatry ClinNeurosci 248(6): 289-295
- Kondo DG, Sung YH, Hellem TL, Fiedler KK, Shi X, et al. (2011b) Open-label adjunctive creatine for female adolescents with SSRI-resistant major depressive disorder: a 31-phosphorus magnetic resonance spectroscopy study. J Affect Disord 135(1-3): 354-361
- Moore CM, Christensen JD, Lafer B, Fava M, Renshaw PF (1997) Lower levels of nucleoside triphosphate in the basal ganglia of depressed subjects: a phosphorous-31 magnetic resonance spectroscopy study. Am J Psychiatry 154(1): 116-118
- Fattal O, Link J, Quinn K, Cohen BH, Franco K (2007) Psychiatric comorbidity in 36 adults with mitochondrial cytopathies. CNS Spectr 12(6): 429-438
- Brambilla P, Perez J, Barale F, Schettini G, Soares JC (2003) GABAergic dysfunction in mood disorders. Mol Psychiatry 8(8): 721-737
- Manji HK, Quiroz JA, Sporn J, Payne JL, Denicoff K, et al. (2003) Enhancing neuronal plasticity and cellular resilience to develop novel, improved therapeutics for difficult-to-treat depression. Biol Psychiatry 53(8): 707-742
- Brambilla P, Cipriani A, Hotopf M, Barbui C (2005) Side-effect profile of fluoxetine in comparison with other SSRIs, tricyclic and newer antidepressants: a meta-analysis of clinical trial data. Pharmacopsychiatry 38(2): 69-77
- Sala M, Coppa F, Cappucciati C, Brambilla P, d'Allio G, et al. (2006) Antidepressants: their effects on cardiac channels, QT prolongation and Torsade de Pointes. CurrOpinInvestig Drugs 7(3): 256-263
- Sala M, Lazzaretti M, De Vidovich G, Caverzasi E, Barale F, et al. (2009) Electrophysiological changes of cardiac function during antidepressant treatment. TherAdvCardiovasc Dis 3(1): 29-43
- Verdoux H, Tournier M, Bigaud B (2009) Pharmacoepidemiology of psychotropic drugs: examples of current research challenges on major public health issues. EpidemiolPsichiatrSoc 18(2): 107-113.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 16285
- [From(publication date):
March-2015 - Apr 06, 2025] - Breakdown by view type
- HTML page views : 11540
- PDF downloads : 4745