Research Article Open Access
Magnetic Resonance Imaging in Complete Denture Treated Edentulous Patients with Obstructive Sleep Apnea Syndrome-A Preliminary Study
Biljana Milosevic1*, Ljiljana Tihacek Sojic2, Ivica Stancic2, Zanka Cerovic3, Elvir Zvrko4 and Goran Nikolic3
1Dental Department, University of Montenegro, Podgorica, Montenegro
2Prosthetic Department, University of Belgrade, Serbia
3Clinical Center of Montenegro, Radiology Department, Podgorica, Montenegro
4Clinical Center of Montenegro, Otorhinolaryngology Department, Podgorica, Montenegro
- *Corresponding Author:
- Biljana Milosevic
Dental Department
University of Montenegro, Montenegro
Tel: +382 69 026 026
E-mail: biljana.m13@gmail.com
Received Date: October 26, 2016; Accepted Date: November 22, 2016; Published Date: November 28, 2016
Citation: Milosevic B, Sojic LT, Stancic I, Cerovic Z, Zvrko E, et al. (2016) Magnetic Resonance Imaging in Complete Denture Treated Edentulous Patients with Obstructive Sleep Apnea Syndrome-A Preliminary Study. J Oral Hyg Health 4: 212. doi: 10.4172/2332-0702.1000212
Copyright: © 2016 Milosevic B, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Oral Hygiene & Health
Abstract
Background: Complex clinical presentation of obstructive sleep apnea syndrome (OSAS) is increasingly present in modern dentistry. In this research, we have been assumed that the reconstruction of optimal vertical dimension of occlusion (VDO) with complete dentures could reduce symptoms of mild to moderate sleep apnea in edentulous patients who have not worn dentures or have used inadequate ones. The aim of this study was to determine how the prosthetic treatment of edentulous patients with OSAS can extend the upper airways, reduce the accompanying day and night symptoms of sleep apnea and reduce the value of apnea-hypopnea index (AHI/h).
Methods: The study comprised 9 edentulous patients with OSAS (AHI/h 5.70 to 26.30). The complete dentures with optimal VDO reconstruction were made for all patients. For the purposes of this study, the following were used: Epworth sleepiness scale (ESS) polysomnographic registration (PSG) of AHI/h, the diagnosis of the diameter of the upper respiratory tract by magnetic resonance imaging (MRI) before and 3 months after the prosthetic rehabilitation.
Results: Prosthetic treatment of edentulous patients reduces day and night time symptoms of OSAS. Sagittal and axial tomograms of the pharynx in edentulous patients with OSAS before and 3 months after the treatment indicate significant differences in the diameter of the upper airways, which are correlated with reduced AHI/h (49.93%).
Conclusion: The complete dentures prosthetic rehabilitation of edentulous patients, with optimal VDO reconstruction, increases the diameter of the upper respiratory tract which is reflected in a significant reduction of OSAS symptoms and AHI/h.
Keywords
Obstructive sleep apnea syndrome; Complete denture, Vertical dimension of occlusion, Polysomnography, Magnetic resonance imaging
Introduction
Obstructive sleep apnea syndrome (OSAS) is a sleep disorder characterized by recurrent episodes of total or partial upper airway obstruction during sleep [1]. In addition to day and night symptoms of the disease, the American Academy of Sleep Medicine [1] recommended the presence of apnea/hypopnea index (AHI/h) of greater than 5 per hour of sleep as a mandatory criterion for the diagnosis of sleep apnea. OSAS prevalence increases with age, and it affects approximately 2-5% of population and the proportion between males and females is 2:1 [2,3].
Pathophysiological mechanisms of OSAS are confirmed by predisposing risk factors such as: orofacial and pharyngeal abnormalities, nasal problems, the volume increase of soft tissue, the reduction of pharyngeal dilator muscle activity, the reduction of lung volume, instability of ventilatory control, surface tension, obesity [4]. Studies which applied magnetic resonance imaging (MRI) in the diagnosis of upper airway patency, showed that the volume of soft tissue structures of the tongue, of the soft palate and of lateral pharyngeal walls increased in patients with OSAS [5]. Thus, patients with OSAS have anatomically compromised upper airways incurred as a result of skeletal abnormalities, soft tissue abnormalities or a combination of these factors.
The leading therapy for OSAS includes the use of continuous positive airway pressure (CPAP). If patients with OSAS do not accept CPAP therapy, other forms of treatment such as oral appliances or surgical procedures [6-8] can be used.
Complex clinical presentation of OSAS is increasingly present in modern dentistry, which allows the treatment of this respiratory disorder using various types of oral appliances (OA). Many studies have indicated that patients with mild to moderate sleep apnea have a 52% chance to improve sleep apnea using oral appliances [9-14].
A special entity represents edentulous patients with symptoms of OSAS. In modern literature there are few data on the incidence of this appearance in edentulous patients and on the treatment possibilities. Heidsieck et al. indicate that currently there are only 20 studies, among which are only 4 clinical trials [15]. Also, there is no consensus in the literature about the effects of nocturnal denture wearing in edentulous patients with OSAS. Heidsieck et al. also point out that there are a small number of effective evidence-based treatment strategies for edentulous OSA patients, and they indicate further need for clinical research [15].
Our study is based on the assumption that reduced vertical dimension of occlusion (VDO) in edentulous patients can lead to the reduction in size of velopharynx and oropharynx, which may be one of the causes of sleep disorders. According to this, the reconstruction of optimal VDO with complete dental restorations could reduce symptoms of mild to moderate sleep apnea, or the value of the index AHI/h in edentulous patients who previously did not wear dentures or who wore inadequate complete dentures.
The main purpose of this study was to determine the effects of the prosthetic treatment with complete dentures in edentulous patients with mild to moderate sleep apnea by using the magnetic resonance imaging (MRI) and polysomnographic registration (PSG).
Materials and Methods
The study was performed at the Faculty of Medicine University of Montenegro in Podgorica and included edentulous patients with sleep apnea symptoms who were not denture wearers, who have been wearing complete dentures for ten or more years or those with inadequate abraded dental restorations.
This study included 9 patients (5 female and 4 male) aged 50-65 years. The main criteria in the selection of patients were the diagnosis of mild (AHI/h=5-15) to moderate sleep apnea (AHI/h=15-30) and the state of tooth loss. Also, all patients included in this study, showed a reduced VDO, tongue hypertrophy, low uvula position and an inclination of the soft palate.
Data collection consisted of the application of questionnaires, the performance of PSG tests and MRI before and 3 months after prosthetic treatment with complete dentures. The Epworth Sleepiness Scale (ESS) was applied to assess the likelihood of sleep disorders and to evaluate the quality of sleep in edentulous patients [16]. Based on the ESS [16] every patient`s sleepiness was assessed with the following characteristics: bad, good, very good or excellent. This questionnarie involved eight questions related to sleepiness. Also, for the purposes of this study it was used a questionnaire designed by the researcher herself. This questionnaire has enabled the impact assessment of the toothless and reduced VDO on signs and symptoms of sleep apnea in the patients, as well as to what extent properly crafted dentures can eliminate this disorder. The questionnaire included 8 questions such as: Q1- how many times do you wake up at night? Q2-do you wake up when you feel your breathing is interrupted? Q4-when did you have your last tooth extracted? Q6-do you wear complete dentures and how long? Q8-do you sleep with complete dentures?
The polysomnographic registrations during sleep were performed for each patient before and 3 months after the prosthetic treatment with complete dentures, in the sleep-laboratory of The Hospital for lung diseases and tuberculosis "Dr Jovan BulajiÄÂ?" in NikšiÄÂ?, Montenegro, after receiving positive opinion of Ethics Committee (decision number 03/01-12120/1).
According to the American Academy of Sleep Medicine [1] the frequency of apnea and hypopnea per hour of sleep is measured with the AHI. The severity of OSAS was determined using the AHI, which consisted of the sum of the mixed obstructive apneas and hypopneas per hour of sleep, when the patient was in the PSG period. OSAS is divided into mild (AHI=5-15), moderate (AHI=15-30) and severe (AHI ≥ 30).
MRI has been performed for 8 patients at the Clinical Center of Montenegro, before and 3 months after the prosthetic treatment with complete dentures. The investigation was done on the machine for magnetic resonance (Siemens, Munchen, Germany), with magnetic field strength 1.5 Tesla, in the T1 sequence. This diagnosis included the orofacial region and the upper respiratory tract (velopharynx and oropharynx). The dimensions of the upper respiratory tract were analyzed in the sagittal and axial planes. The following parameters were evaluated:
a) In the sagittal plane
1 - The diameter of the velopharynx before and after treatment
2 - The diameter of the oropharynx before and after treatment
3 - The diameter of the airway at the border of the velopharynx and of the oropharynx (at the level of the tip of the uvula)
b) In the axial plane
1- The anteroposterior diameter of the pharynx at the level of the tip of the uvula
2 -The laterolateral diameter of the pharynx at the level of the tip of the uvula
Computed tomography (CT) was performed for one patient with pace-maker contraindication for magnetic resonance. The examination of this patient was performed on a 64-slice scanner, a section thickness of 0.6 mm with multiplanar reconstruction, and the dimensions in the axial and sagittal planes were also analyzed before and after prosthetic treatment.
For the purpose of this research, new complete dentures in the upper and lower jaw with optimal reconstruction of occlusion were made for each patient. During the stage of determining intermaxillary relationships, optimal VDO reconstruction was performed in accordance with the established clinical procedures.
The control examinations of the patients were carried out in the first and second month after the application of complete dentures, when the patients filled in the questionnaires mentioned before.
In order to carry out the necessary statistical tests, a statistical software package IBM Statistics for Windows (20.0) was used. At the start of the study, all the characteristics were described by descriptive statistics methods. Numerical characteristics are described by the common measures of central tendency and a measure of dispersion: arithmetic mean, standard deviation and median. The results obtained are presented in tables and figures. P-values <0.01 are considered as statistically significant.
Results
Polysomnographic testing showed that the index values of AHI/h before the prosthetic rehabilitation with removable dentures were from 5.70 to 26.30. After the treatment the value of AHI/h was with the range from 1.60 to 15.70. The average value of AHI/h at the group level before the treatment was 14.84 ± 7.54. The average value of AHI/h three months after the treatment with complete dentures was 7.43 ± 4.92. i.e., reduced for 49.93% compared to the values of the index before the prosthetic treatment (Table 1).
| Gender | AHI/h | Sag. | Oropharynx | (mm) | Sag. | PharynxA-P | (mm) | ||
|---|---|---|---|---|---|---|---|---|---|
| B.th | A.th | Imp. (%) | B.th | A.th | Imp. (%) | B.th | A.th | Imp. (%) | |
| F | 24.6 | 10.2 | 58.54 | 9 | 11.5 | 27.78 | 4.9 | 7.3 | 121.2 |
| F | 14.5 | 10.3 | 28.97 | 12.5 | 14.6 | 16.8 | 8.7 | 8.6 | 17.81 |
| F | 6.6 | 1.6 | 75.76 | 6.3 | 7 | 11.11 | 2.8 | 5.5 | 205.6 |
| F | 5.7 | 3.4 | 55.26 | 6.3 | 11.3 | 79.37 | 5.7 | 6.3 | 10.83 |
| F | 26.3 | 15.7 | 40.3 | 8.7 | 12.2 | 40.23 | 4.5 | 5.8 | 163.6 |
| M | 14.4 | 6.7 | 53.47 | 8.7 | 16.3 | 87.36 | 4 | 7.3 | 121.2 |
| M | 9.6 | 2.4 | 75 | 13.3 | 14 | 5.26 | 4.7 | 13.7 | 50.55 |
| M | 11.1 | 4.3 | 61.26 | 10.6 | 10.9 | 2.83 | 5.4 | 12.5 | 140.4 |
| M | 20.8 | 12.3 | 40.87 | 8.4 | 10 | 19.05 | 6 | 9.4 | 46.88 |
| Velopharynx | (mm) | Sag. | Uvula level | (mm) | Ax. | Ax. | Pharynx L-L | (mm) | |
| A.th | Imp. (%) | B.th | A.th | Imp. (%) | B.th | B.th | A.th | Imp. (%) | |
| F | 9 | 83.67 | 4.9 | 6.6 | 34.69 | 3.3 | 15.3 | 16.8 | 9.8 |
| F | 12.5 | 43.68 | 5.2 | 8.7 | 67.31 | 7.3 | 10.1 | 11.6 | 14.85 |
| F | 4.9 | 75 | 2.1 | 4.4 | 109.5 | 1.8 | 13.2 | 17.5 | 32.58 |
| F | 10.3 | 80.7 | 4.3 | 8 | 86.05 | 5.7 | 14.7 | 21.6 | 46.94 |
| F | 7.3 | 62.22 | 0 | 8.3 | 2.2 | 18.6 | 21.5 | 15.59 | |
| M | 9 | 125 | 0 | 9.3 | 3.3 | 13.7 | 21 | 53.28 | |
| M | 7 | 48.94 | 7.7 | 10 | 29.87 | 9.1 | 17.4 | 20.2 | 16.09 |
| M | 9.9 | 83.33 | 6.1 | 10.2 | 67.21 | 5.2 | 19.5 | 20.6 | 5.64 |
| M | 7 | 16.67 | 4.7 | 8.5 | 80.85 | 6.4 | 25.6 | 24.6 | -3.91 |
B.th - Before therapy; A.th – After therapy; Imp. - Improvement
Table 1: Polysomnography and magnetic resonance parameters before and after prosthetic rehabilitation of edentulous patients.
The analysis of data obtained from the questionnaires before the prosthetic treatment showed that the patients, with the values of the index AHI/h 24.60, 26.30 and 20.80 belong to a high risk group for sleep apnea, and based on the Epworth sleepiness scale their dream was assessed as bad. The quality of sleep in patients with the index values of AHI/h 9.60, 11.10, 14.50 and 14.40 was estimated as good, whereas in patients with the index values of AHI/h 6.60 and 5.50 was very good.
The analysis of data obtained from those questionnaires after the prosthetic treatment showed that the prosthetic rehabilitation in four patients eliminated sleep apnea (AHI/h 2.40, 4.30, 3.40, and 1.60), and their dream was assessed as excellent. The dream of one patient with the values of AHI/h 6.70 was assessed as very-good, while of four subjects with the index values of AHI/h 12.30, 15.70, 10.20 and 10.30 was estimated as good.
The diagnosis by magnetic resonance showed differences in the diameter of upper airways before and 3 months after the treatment with complete dentures in edentulous patients with mild to moderate sleep apnea.
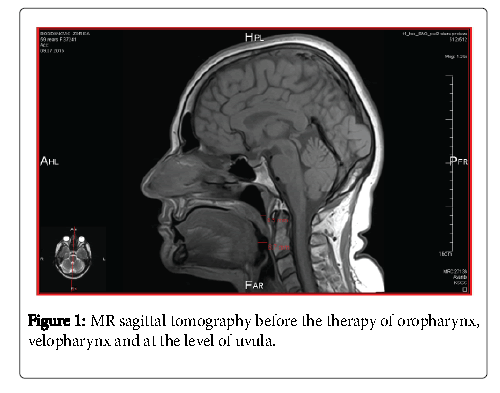
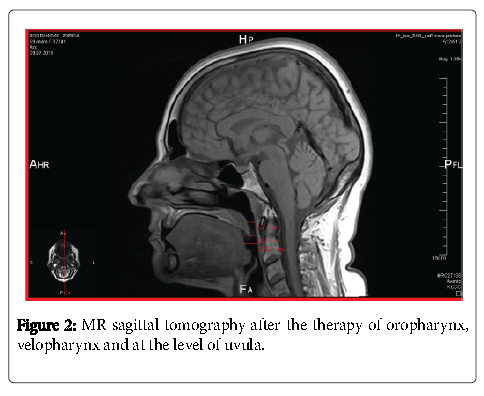
The sagittal tomogram of the oropharynx
The diameter of the oropharynx before the prosthetic rehabilitation of edentulous patients ranged from 6.30 mm to 13.30 mm, and after therapy from 7.00 mm to 16.30 mm (Table 1). The average value of the diameter of the oropharynx was 9.31 ± 2.44 before the treatment. Three months after the treatment with complete dentures the diameter amounted to 11.97 ± 2.74 i.e., it increased to 28.57% compared to the value before the prosthetic treatment (Figures 1 and 2).
The sagittal tomogram of the velopharynx
The average value of the diameter of the velopharynx before the treatment with complete dentures was 5.18 ± 1.62 and after therapy 8.54 ± 2.25 (Table 1). The prosthetic rehabilitation increased the velopharynx to 64.86% compared to the average value of the diameter before the treatment (Figures 1 and 2).
The sagittal tomogram at the level of the uvula
The average value of the diameter at the level of the uvula before the treatment with complete dentures was 3.88 ± 2.66 and after the treatment 8.22 ± 1.80 (Table 1). The prosthetic rehabilitation increased the segment of the upper airway at the level of the uvula to 111.33% compared to the average value of the diameter before the treatment (Figures 1 and 2).
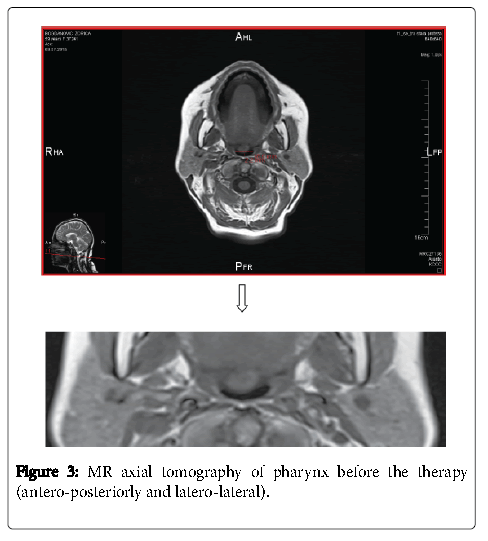
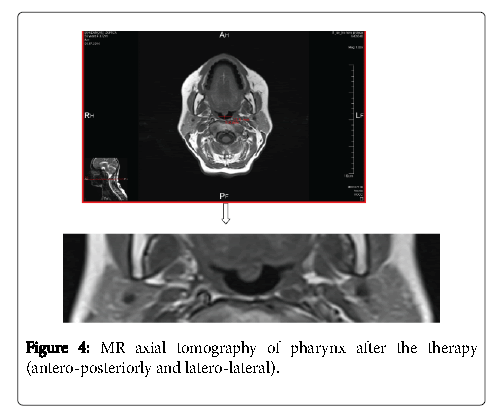
The axial tomogram of the pharynx at the level of the uvula anteroposterior
The diameter of the pharynx at the level of the uvula in the axial plane anteroposterior before the prosthetic rehabilitation with complete dentures ranged from 1.80 mm to 9.10 mm, after the treatment it ranged from 5.50 mm to 13.70 mm. The average value of the diameter of the pharynx at the level of the uvula in the anteroposterior position before the treatment was 4.92 ± 2.46 (Table 1). Three months after the treatment with complete dentures the diameter amounted to 8.49 ± 2.91, i.e., it increased to 72.36% compared to the value before the prosthetic treatment (Figures 3 and 4).
The axial tomogram of the pharynx at the level of the uvula laterolateral
The average value of the diameter at the level of the uvula laterolateral in the axial level was 16.46 ± 4.49 before the treatment and 19.48 ± 3.74 after the treatment with complete dentures (Table 1). The prosthetic rehabilitation increased the diameter of the pharynx at the level of the uvula in the axial plane laterolateral to 18.35% compared to the average value of the diameter before the treatment (Figures 3 and 4).
Discussion
Many studies have suggested that morphological changes caused by tooth loss result in a decrease in the vertical dimension of occlusion, reduction of the lower face height and anterior rotation of the mandible [17]. Furthermore, many studies have confirmed that the lowered soft palate, uvula, and tongue hypertrophy are predisposing factors for the occurrence of sleep apnea [18].
OSAS treatment includes several therapeutic measures from simple changes in habits to the use of CPAP and oral appliances. The goal of oral appliances is to increase the upper airway dimension during sleep by repositioning the mandible in a forward and downward position [19]. Oral appliances and CPAP therapies have similar results in treating mild to moderate sleep apnea, but the fact is that CPAP is more effective [20].
In this study, the modality of treatment of mild to moderate sleep apnea consisted of making complete dentures in edentulous patients. The patients did not meet the criteria for making oral appliances and it was considered that the application of CPAP had to be aggressive and less comfortable treatment method for such patients. The edentulous patients in this study were found to have tongue hypertrophy, an inclination of the soft palate and a lower position level of the uvula, indicating that reduced VDO changes the position of the soft-tissue structures and decreases the diameter of the upper air ways in the sagittal and axial planes. This is the reason why the basic idea of this research was that the adequate prosthetic treatment which optimally corrects VDO could significantly reduce mild to moderate sleep apnea in edentulous patients.
Bucca et al. compared the PSG results of edentulous individuals while sleeping with and without dentures [21]. It showed that the AHI/h was significantly worse in the edentulous patients who slept without dentures than when they slept with them. According to these findings careful attention should be paid to edentulous individuals who sleep with their dentures in order to prevent appearance of OSAS [21]. Furthermore, Arisaka et al. indicate that complete dentures wear during sleep reduces AHI/h in the majority of patients [22]. These results support our study because our edentulous patients were undergone to PSG while wearing dentures.
In this study, the prosthetic treatment of edentulous patients with complete dentures significantly increased the velopharynx and thus allowed a higher airflow, which is reflected in the reduction of the index AHI/h for 49.93%. After the prosthetic rehabilitation the incidence of dramatic wakening episodes was significantly reduced which influenced the quality of sleep.
The definition which is considered as the most stringent criterion for the success of therapy in patients with sleep apnea is to reduce respiratory problems at <5 per hour of sleep [1]. This study showed that the use of prosthetic rehabilitation in four patients reduced the value of AHI/h <5 and thus eliminated OSA and accompanying day and night time symptoms.
Many studies showed the similar results of a mandible repositioning device (MRD) therapy in treating patients with mild to moderate sleep apnea [23-25]. Its therapeutic success was confirmed in the reduction of AHI/h less than 5 or reduction in number of respiratory disorders per hour of sleep, with an average success rate from 29% [25] to 57% [24]. Also, these results are achieved by Tripathi et al. by using mandibular advancement devices (MAD) in the treatment of 10 edentulous OSA patients [26]. These results indicate that MAD can be effective in reducing sleep apnea by lowering the AHI/h and improving sleep quality after 6 months of its use [26].
According to the differences in treatment modalities of sleep apnea, various assessments of the therapy success and differences in the interpretation of results, it is very complex to perform a comparison of this study research results with the results of other studies that focused on the treatment of mild to moderate sleep apnea. This is far more difficult because of the fact that this study investigates the frequency and intensity of sleep apnea in edentulous patients and treatment options of this disorder by making complete dentures.
Consequently, many authors confirm the positive effects of prosthetic rehabilitation in edentulous patients with moderate and severe sleep apnea [27,28]. Emami et al. show that the effects of prosthetic rehabilitation in edentulous patients with moderate and severe sleep apnea may have a preventive approach to the improvement of sleep characteristics of the older population and their quality of life [27]. Erovigni et al. show that wearing complete dentures changes the position of tongue, jaw and esophagus which causes the reduction of apneic episodes [28].
MRI showed significant differences in the dimensions of velopharynx and oropharynx before and 3 months after the prosthetic treatment of edentulous patients, both in the sagittal and the axial planes. The prosthetic rehabilitation with complete dentures increased the diameters of the velopharynx and oropharynx in the sagittal plane as well as at the uvula level. Axial tomograms after the treatment showed an increase of the pharynx at the uvula level, anteroposterior and laterolateral.
These findings correlates with the results of some authors [5,29]. Gao et al. investigated the upper airway changes after wearing dental appliances in 11 patients with OSA [5]. MRI before and after the dental appliance treatment confirmed its effect of enlarging upper airway. Also, using the MRI of the upper airway during sleep, Ishida et al. showed a significant increase of velopharynx in 9 patients who were treated with prosthetic mandibular advancement (PMA) [30].
Absolute confirmation of the hypothesis that launched this research proves the justification, appropriateness and applicability of the prosthetic therapy with complete dentures as a treatment modality of obstructive sleep apnea.
Conclusion
The results of this study have indicated that the complete dentures prosthetic therapy with an optimal VDO reconstruction contributed to an increase in the diameter of the upper respiratory tract, a significant increase of velopharynx and it allowed a greater airflow reducing obstructive sleep apnea symptoms and accordingly a better quality of life. Magnetic resonance imaging and polysomnographic registration during sleep can be used as a reliable and non-invasive method in the diagnosis and monitoring the effects of sleep apnea treatment by the application of complete dentures in edentulous patients.
References
- American Academy of Sleep Medicine (2005) The international classification of sleep disorders diagnostic & coding manual.American Academy of Sleep Medicine, Westchester.
- Tufik S, Silva SR, Taddei JA, Bittencourt LR (2010) Obstructive sleep apnea syndrome in the Sao Paulo epidemiologic sleep study. Sleep Med 11:441-446.
- Bixler EO, Vgontzas AN, Ten Have T, Tyson K, Kales A (1998) Effects of age on sleep apnea in men: I. Prevalence and severity. Am JRespirCrit Care Med 157:144-148.
- Pham LV, Schwartz AR (2015) The pathogenesis of obstructive sleep apnea. J Thorac Dis 7:1358-1372.
- Gao XM, Zeng XL, Fu MK, Huang XZ (1999) Magnetic resonance imaging of the upper airway in obstructive sleep apnea before and after oral appliance therapy. Chin J Dent Res 2:27-35.
- McArdle N, Douglas NJ (2001) Effect of continuous positive airway pressure on sleep architecture in the sleep apnea-hypopnea syndrome: a randomized controlled trial. Am J RespirCritCare Med 164:1459-1463.
- McDaid C, Griffin S, Weatherly H, Duree K, van der Burgt M, etal. (2009) Continuous positive airway pressure devices for the treatment of obstructive sleep apnoea-hypopnoea syndrome: a systematic review and economic analysis. Health Technol Assess 13: 143-274.
- Kushida CA, Littner MR, Hirshkowitz M(2006) Practice parameters for the use of continuous and bilevel positive airway pressure devices to treat adult patients with sleep-related breathing disorders. An American Academy of Sleep Medicine Report. Sleep29:375-380.
- Barthlen GM, Brown LK, Wiland MR, Sadeh JS, Patwari J, et al. (2000) Comparison of three oral appliances for treatment of severe obstructive sleep apnea syndrome. Sleep Medicine 1:299-305.
- Gotsopoulos H, Chen C, Qian J, Cistulli PA (2002) Oral appliance therapy improves symptoms in obstructive sleep apnoea: a randomized, controlled trial. Am J RespirCrit Care Med 166:743-748.
- Hoekema A, Stegenga B, De Bont LG (2004) Efficacy and comorbidity of oral appliances in the treatment of obstructive sleep apnea-hypopnea: A systematic review. Crit Rev Oral Biol Med 15:137-155.
- Tihacek-Sojic L, Andjelkovic M, Milic-Lemic A, Milosevic B (2012) The effectiveness of oral appliances in elderly patients with obstructive sleep apnoea treated with lorazepam-a pilot study. J Oral Rehabil 39:785-790.
- Milosevic B (2012) Oral appliances in sleep apnea therapy.
- Al-Jewair TS, Gaffar BO, Flores-Mir C (2016) Quality assessment of systematic reviews on the efficacy of oral appliance therapy for adult and pediatric sleep-disordered breathing. J Clin Sleep Med 12:1175-1183.
- Heidsieck DS, de Ruiter MH, de Lange J (2016) Management of obstructive sleep apnea in edentulous patients: an overview of the literature. Sleep Breath 20:395-404.
- Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep14:540-545.
- Ivanhoe JR, Cibirka RM, Lefebvre CA, Parr GR (1999) Dental considerations in upper airway sleep disorders: A review of the literature. J Prosthet Dent82:685-698.
- Calero EA, Escalona EE, Mora JM, Carreras JML, Reina ES (2012) Obstructive sleep apnea syndrome (OSAS). Med Oral Patol Oral Cir Bucal 17: e925-e929.
- Marklund M (2006) Predictors of long term orthodontic side effects from mandibular advancement devices in patients with snoring and obstructive sleep apnea. Am J OrthodDentofacialOrthop129:214-221.
- Barnes M, McEvoy RD, Banks S, Tarquinio N, Murray CG, et al. (2004) Efficacy of positive airway pressure and oral appliance in mild to moderate obstructive sleep apnoea. Am J RespirCrit Care Med 170:656-664.
- Bucca C, Cicolin A, Brussino L, Arienti A, Graziano A, et al. (2006) Tooth loss and obstructive sleep apnoea. Respir Res7:8.
- Arisaka H, Sakuraba S, Tamaki K, Watanabe T, Takeda J, et al. (2009) Effects ofwearing complete dentures during sleep on the apnea-hypopnea index. Int J Prosthodont22:173-177.
- Mehta A, Qian J, Petocz P, Darcndeliler MA, Cistulli PA (2001) Randomized, controlled study of a mandibular advancement splint for obstructive sleep apnea. Am J RespirCrit Care Med 163:1457-1461.
- Pitsis AJ, Darendeliler MA, Gotsopoulos H, Pelocz P, Cistulli PA (2002) Effect of vertical dimension on efficacy of oral appliance therapy in obstructive sleep apnea. Am J RespirCrit Care Med 166:860-864.
- Rose E, Staats R, Virchow C, Jonas IE (2002) A comparative study of two mandibular advancement appliances for the treatment of obstructive sleep apnoea. Eur J Orthod 23:191-198.
- Tripathi A, Gupta A, Tripathi S, Dubey A (2014) A novel use of complete denture prosthesis as mandibular advancement device in the treatment of obstructive sleep apnea in edentulous subjects. J Dental Sleep Med 1:115-119.
- Emami E, Nguyen PT, Almeida FR, Feine JS, Karp I, et al. (2014) The effect of nocturnal wear of complete dentures on sleep and oral health related quality of life: study protocol for a randomized controlled trial. Trials 15:358.
- Erovigni F, Graziano A, Ceruti P, Gassino G, De Lillo A, etal. (2005) Cephalometric evaluation of the upper airway in patients with complete dentures. Minerva Stomatol 54:293-301.
- Gale DJ, Sawyer RH, Woodcock A, Stone P, Thompson R, et al. (2000) Oral appliances enlarge the airway in patients with obstructive sleep apnoea? A prospective computerized tomographic study. Eur J Orthod 22: 159-168.
- Ishida M, Inoue Y, Suto Y, Okamoto K, Ryoke K, et al. (1998) Mechanism of action and therapeutic indication of prosthetic mandibular advancement in obstructive sleep apnea syndrome.Psychiatry ClinNeurosci 52: 227-229.
Relevant Topics
- Advanced Bleeding Gums
- Advanced Receeding Gums
- Bleeding Gums
- Children’s Oral Health
- Coronal Fracture
- Dental Anestheia and Sedation
- Dental Plaque
- Dental Radiology
- Dentistry and Diabetes
- Fluoride Treatments
- Gum Cancer
- Gum Infection
- Occlusal Splint
- Oral and Maxillofacial Pathology
- Oral Hygiene
- Oral Hygiene Blogs
- Oral Hygiene Case Reports
- Oral Hygiene Practice
- Oral Leukoplakia
- Oral Microbiome
- Oral Rehydration
- Oral Surgery Special Issue
- Orthodontistry
- Periodontal Disease Management
- Periodontistry
- Root Canal Treatment
- Tele-Dentistry
Recommended Journals
Article Tools
Article Usage
- Total views: 3660
- [From(publication date):
November-2016 - Apr 24, 2025] - Breakdown by view type
- HTML page views : 2830
- PDF downloads : 830