Review Article Open Access
Magnesium, Iron and Zinc Alloys, the Trifecta of Bioresorbable Orthopaedic and Vascular Implantation - A Review
Michael Heiden, Emily Walker and Lia Stanciu*School of Materials Engineering, Purdue University, West Lafayette, Indiana, USA
- Corresponding Author:
- Lia Stanciu
Materials Engineering, Purdue University
701 West Stadium Avenue, West Lafayette, IN 47907, USA
Tel: 7654963552
E-mail: lstanciu@purdue.edu
Received date:: March 04, 2015; Accepted date:: April 23, 2015; Published date:: April 30, 2015
Citation: Heiden M, Walker E, Stanciu L (2015) Magnesium, Iron and Zinc Alloys, the Trifecta of Bioresorbable Orthopaedic and Vascular Implantation – A Review. J Biotechnol Biomater 5:178. doi:http://dx.doi.org/10.4172/biotechnology-biomaterials.1000178
Copyright: © 2015 Heiden M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Biotechnology & Biomaterials
Abstract
Bioresorbable metals continue to have immense potential to be used in the clinical treatment of a variety of soft and hard tissue injuries and disease. For many applications, the presence of a permanent device may cause severe negative effects and require re-intervention in the long-term. A transient support for a healing tissue is an attractive solution for orthopaedic and vascular interventions alike. The mechanical properties of metals in particular make them attractive candidates for this temporary support. This review aims to provide an update and insight into the current status of absorbable metal designs, as well as to discuss ongoing issues regarding the use of such materials as degradable orthopaedic fixation devices and vascular scaffolds. An effort was made to assemble a comprehensive list of the necessary requirements going forward for these unique implants, along with the reported degradation rates discovered in literature for various resorbable alloys. Furthermore, this work aims to clearly illuminate the current challenges that must be overcome in order for these unique materials to become viable replacements for permanent designs in clinical use.
Keywords
Ransient implants; Bioresorbable metals; Biodegradation
Introduction
Issues associated with permanent biomedical implants include inflammation, thrombus formation, stress shielding, and reintervention to remove a device with transient functionality. In this context, it is desirable to replace some of the existing titanium, cobaltchromium, and stainless steel permanent vascular and orthopaedic implants that have temporary functionality, with bioresorbable alternatives. Other issues include long-term migration of the implant, pain associated with fracture, interferences induced by the magnetic field of the material with standard imaging equipment, and the restriction posed on the development of new tissue within young patients [1].
Existing hard tissue biomaterials are employed as permanent fixation devices which are used primarily in load-bearing applications. Examples include bone plates, staples, suture anchors, screws and pins to secure fractures, along with dental implants [2]. However, most fracture fixation devices are removed after healing, requiring invasive procedures and additional costs. In case of load-bearing, fracture fixation devices, such as intramedullary rods or bone plates, stress shielding (bone becomes weaker due to transfer of normal stresses to stiffer implant) is another challenge associated with their permanent in-vivo presence [3,4].
For vascular therapies, late stent thrombosis and restenosis due to permanent metal and drug eluting stents are persistent problems [5,6]. Furthermore, permanent stenting can result in jailing of side branches of a blood vessel, preventing intervention in nearby affected sites [6]. An ideal vascular scaffold would support the vessel with adequate radial force to prevent elastic recoil during the healing process following angiography, and disappear at the same rate as the vessel heals, restoring normal vasoreactivity [5]. Degradable polymers have been explored, but vascular scaffolds made from these materials require a larger strut size compared with their metal counterparts in order to produce the required mechanical properties to prevent vessel recoil [5]. However, it is important to note that most other proposed resorbable metallic scaffolds have also been reported having thicker strut sizes than the current permanent metallic vascular scaffolds [7,8]. Depending on the design, this larger profile can impact the hemodynamics of the vessel [9]. In the past, bioabsorbable polymer designs have suffered from poor control of degradation rate based on manufacturing routes used [10]. More recently however, degradation rates are becoming better controlled by altering hydrophilic or hydrophobic end groups, adding copolymers, or adding other catalysts to the design [11]. For example, Kim et al. found that electrospinning PLA with PLGA helped enhance degradation [12]. Nevertheless, problems remain for polymeric scaffolds in that there tends to be a rapid loss of radial strength as soon as hydrolysis causes depolymerization [11].
For these reasons, interest in bioresorbable metallic vascular scaffolds and orthopaedic fracture fixation devices has increased in the last decade [13]. The purpose of this paper is to review the current development of bioresorbable hard and soft tissue metallic implants and provide a potential outline for future considerations.
Criteria for Bioresorbable Implants
To achieve the ultimate bioresorbable tissue implant, a series of general conditions need to be fulfilled before the material can be used clinically [1]. Table 1 specifies more detailed, individual requirements for vascular and orthopaedic applications since their environments and mechanically supportive needs differ. Though, it appears many of the desired mechanical properties in literature have been based off of current, clinically employed stents such as stainless steels, which may prove in the future to be slightly different for resorbable applications. It is also important to note that there currently exists no vascular scaffold or orthopaedic implant with every ideal property listed, however depending on the environment and application, the most appropriate implant can be chosen.
| Properties | Vascular Resorbable Scaffolds | OrthopaedicResorbable Scaffolds |
|---|---|---|
| Constraints | Constraints | |
| Cell Response | Encourage endothelial cell attachment, but not smooth muscle cell attachment, as it may have a negative effect on vessel patency [10,14] | Encourage new bone formation through both osteoblast and osteoclast attachment and proliferation, but also avoid fibrous capsule formation [15] |
| Mechanical Integrity | > 8 months > 6-12 months [1,7,13,16] |
> 6 months (Based on longest healing time for neck of femur) [16] |
| Yield Strength | > 200MPa [17] | > 230MPa [18] |
| Ultimate Tensile Strength | > 300MPa [17] | > 300MPa [17] |
| Elongation to Failure (%Strain) |
> 15-18% Higher ductility is ideal for higher flexibility while expanded while in arteries, but still need enough radial force to open lesions [17,19] |
> 15-18% [17] |
| Elastic Modulus | Low elastic modulus to be able to bend around the human circulatory system, but still stiff enough to retain necessary hoop and radial strengths for artery support [20-22] | As close to cortical bone as possible to avoid stress-shielding (10-20 GPa) [3] |
| Fatigue Strength at 10^7 cycles (Mpa) | > 256 Strength must be sufficient to prevent acute recoil and negative remodeling [2,4,17,29] |
> 256 [17,19] |
| Elastic Recoil on Expansion | < 4% [17] | N/A |
| Hydrogen Evolution | < 10 uL/cm^2/day (Though blood flow may increase this maximum tolerance) [17,25] |
< 10 uL/cm^2/day [25,26] |
Table 1: Desired properties for resorbable materials based on application.
1. The material must be biocompatible and not produce any negative local or systemic side effects in vivo, thereby requiring immediate elimination from the body; i.e. no inflammatory responses or destructive gas bubble formation.
2. The material must fully mechanically support the tissue under reconstruction for the full period of healing. For hard tissue applications in particular, the material should have an elastic modulus as close as possible to that of natural bone to minimize or eliminate severe stress concentrations while supporting the surrounding hard tissue. A material with too high of an elastic modulus denies the bone its normal stress, delaying the natural production of bone [2]. Furthermore, the compressive and tensile strengths of the material should be greater than the tissue that it supports to protect from further fracture. High fatigue strength and fracture resistance are also essential in absorbing the natural stresses and loads experienced by the skeletal system.
3. To increase the likelihood of the implant integrating well with the surrounding tissue, the surface chemistry, roughness and topography all need to be carefully tailored to promote suitable cell adhesion and proliferation in each particular environment.
4. The degradation parameters need to be carefully controlled in order for the material to be completely resorbed in a timely manner (generally accepted as within a few years) [1]. After degradation of the implant, there should not be any residual material left in the system that could produce detrimental effects to the healthy tissue. Furthermore, the degradation mode of the implant must not cause tissue damage; flakes or large chunks of metal must be avoided during degradation, which could detrimentally obstruct or block normal cellular functions.
In recent years, research on bioresorbable materials has navigated away from ceramic-based biomaterials due to their brittle nature and low degradability, though hydroxyapatite and calcium phosphates paired with resorbable metals are currently being investigated [27,28]. In the last decade, resorbable studies have mainly focused on investigating biodegradable polymers [1,29-34]. However, many degradable polymers display insufficient strength to withstand the structural support needed for the reconstruction of both soft and hard tissues within the body. Stress relaxation and creep also tend to occur in polymeric materials, decreasing the material’s ability to encourage tissue regrowth through mechanical support [1].
The low hardness of polymer orthopaedic screws has been found to be inadequate to withstand screw insertion, where threads can be damaged or the screw’s head can be torn off due to the high amount of torque [3]. Additionally, the degradation products from many types of polymers typically have high chances of causing negative tissue reactions within the patient, generating inflammatory responses, swelling, and subsequent cytotoxicity [1,34].
The degradation speed of these potential implants also needs to be further optimized. Drogset et al conducted an experiment on nineteen human patients with anterior cruciate ligament ruptures and used poly- L-lactic acid interference screws to fix them in place for reconstructive healing. After two years, one third of the volume of the screw was remaining in the bone tunnels, which is considered excessive [29]. In order for polymers to become more viable as bioresorbable materials, the mechanical, thermal and viscoelastic properties need to be further optimized.
Metallic biomaterials similarly need to overcome several obstacles concerning optimizing the degradation rate and eliminating any toxic effects that could occur in the body before becoming practical supportive materials for clinical applications [35]. The advantages of using metals as bioresorbable materials include their typically high impact strengths, wear resistances, ductility and toughness. Moreover, some types of metals such as magnesium, iron, and zinc already exist in varying quantities within the human body, which highlight them as highly biocompatible [36].
However it is important for scientists and engineers to carefully monitor the concentration of ion metals diffusing into the surrounding tissues. Another challenge is the fact that several metal implants interfere with radiologic images of the underlying tissues, making it difficult to follow the evolution of the device within the body [19]. The current state on the viability of employing specific biodegradable metal implants in hard and soft tissues is discussed below. Additionally, Table 2 is provided in the appendix in order to show side-by-side comparisons of past recorded degradation rates of different metal alloys in a variety of media. Only values that were explicit within the literature were included.
Biocompatibility of Metallic Degradation Products
The body contains several types of trace metallic elements, including chromium, manganese, iron, cobalt, nickel, copper, zinc, and molybdenum. Magnesium and calcium, however, are described as major metallic elements in the human body. Previous research on bioresorbable metals has predominantly focused on base metals of magnesium or iron, with a variety of elements being alloyed with them, though most recently there has also been some interesting investigations into using zinc alloys for absorbable applications [17,37].
There have been no major reports of these particular elements causing cytotoxicity to the body, which heightens their viability as potential bioresorbable materials. However, excess concentrations of degradation products above the daily elemental allowance of any of these metals have been found to cause other long-term symptoms to occur within the body: Hypermagnesemia can develop from excess magnesium, which can be linked to diseases such as arrhythmia and asystole; hydrogen gas bubbles formed from degrading magnesium have the possibility of blocking blood vessels or causing death of the patient. Recently, Seitz et al. illuminated that products from some Mg implants such as hydroxides, oxides, chlorides and Mg apatites can cause a “burst release” of corrosion products and changes occur in local cell activity due to alkalization [38]. Excessive iron has been shown to generate lesions in the gastrointestinal tract, cause abdominal pain, fatigue, and liver damage, while manganese can cause manganism, which causes negative psychiatric and motor effects [16,35]. Zinc overload on the other hand can cause neurotoxicity [16]. Consequently, controlling the degradation rate of any of these materials is vital for long-term health.
Magnesium Alloys
Orthopaedic potential
Magnesium alloys have been primarily investigated as a prospective candidate for use as clinical degradable materials. Their capacity as an orthopaedic material has been heightened by the fact that these alloys are biocompatible and have elastic moduli, toughness, and compressive yield strength values comparable to cancellous bone [39]. In general, bone modulus varies with a person’s age, the type of bone, and the direction of measurement, but previous studies appear to establish that cancellous bone’s Young’s modulus is between 0.01-2 GPa and its compressive strength is between 0.2-80 MPa which is comparable to several current synthesized Mg alloys [40]. However, even though a low modulus aids against stress-shielding, this can increase the chance of fracture in high load situations such as large compressive loads in the spine [25]. Thus, a balance must be sought when designing to these particular applications.
The most commonly reported downside of these metallic materials is that they corrode too rapidly to allow full completion of tissue reconstruction as they lack the necessary resistance to the high content of chloride elements in the bodily environment, which has a pH around 7.4–7.6 [41]. Moreover, various experiments have been conducted both in vitro and in vivo which demonstrates that the degradation of most Mg alloys causes the formation of large amounts of gas, resulting in wound interface cavitation and tissue necrosis [26,42]. This is due to the aqueous environment forming products of magnesium hydroxide and hydrogen gas [43]. Currently, additional procedures employing syringes are necessary soon after implantation in order to diffuse out the gas that is generated and alleviate the discomfort of the patient. The reported tolerable rate of hydrogen gas release is 10 μL/cm^2/day [25]. In tailoring the degradation rate for a Mg implant, Yuen et al. suggests that the daily exposure limit for an average 60-kg adult is about 350- 400 mg of magnesium [35].
Li et al. demonstrated how open pores and large surface areas can aid fluid transport in the body, accelerating tissue reconstruction, along with increasing in-growth of bone tissues [44]. This study showed how porous metallic materials can enhance long-term fixation between bone tissue and the implants. However, the authors used the shape memory alloy NiTi. Nasab et al. explains that while nickel is necessary in stimulating the immune system, it can be toxic when there is a high dissolution of nickel ions or wear particles in the body [45]. Thus, researchers have focused more on the potential of Mg alloys instead, though interestingly enough, past alloys experimented with typically consist of various concentrations of aluminum, which has major concerns related to its toxicology [35]. AZ31 (Al: 3%, Zn: 1%, Mg: Balance) , AZ91 (Al: 9%, Zn: 1%, Mg: Balance), WE43 (Nd: 71%, Ce: 8%, Dy: 8%, Pr: 8%, Mg: Balance), and LAE442 (Ce: 51%, La: 22%, Nd: 16%, Pr: 8%, Mg: Balance) were tested by F. Witte et al., who determined that AZ31, AZ91 and WE43 degraded faster in vivo than the alloy LAE442 [46]. They also found that alloying magnesium with aluminum and zinc increased the rate of oxidation, while alloying with rare earth elements decreased the oxidation rate [46]. However, there was still a release of subcutaneous hydrogen gas bubbles that had to be punctured with a syringe seen in Figure 1.
Hampp et al. also proposed the LAE442 alloy and another type designated as LANd442, which is similar to LAE442 except the rare earth mixture was replaced by the individual element neodymium [47]. They also tested their alloys on live rabbits and saw an increase in bone volume and bone porosity, but a decrease in bone density. On the other hand, the control group of rabbits that underwent surgery and received no implant showed active bone remodeling as well, indicating that the surgery method itself leads to some cell activation and also initiates the remodeling processes [47].
One alloy with biocompatibility potential that was later dismissed by Huehnerschulte et al. was ZEK100 [48]. Huehnerschulte et al. describes how this Mg alloy induced an unfavorable osteoclastogenic resorbption of old bone and a rushed reactive formation of new bone [48]. Dziuba et al. further supports this negative outcome by showing how ZEK100 specifically induced pathological effects on the host tissue following complete degradation and needs to be removed from future biomedical testing [49].
A Mg-Nd-Zn-Zr (NZK) alloy was tested by Wang et al., who concluded through hemolysis and cytotoxicity tests that the alloy exhibited good hemocompatibility and cytocompatibility in vitro [50]. They also demonstrated that the addition of alloying elements such as Nd, Zn, and Zr increases the high corrosion resistance of magnesium. Li et al. found promise in using Mg-Ca alloys, which demonstrated an increase in osteoblasts and osteocytes around the Mg-1Ca alloy pin [28]. The metallic device also degraded within ninety days in vivo and showed no signs of toxicity, elevating it to a significantly high potential for clinical viability [28].
More recently Xia et al. experimented with an Mg–4.0Zn–0.2Ca alloy that did not exhibit any cytotoxicity on osteoblast cells and furthermore 35-38% of the implant had degraded after ninety days in vitro [51]. No inflammation reaction was detected and new bone was observed around the remaining implant [51]. Celarek et al. conducted another study with ZX50 (MgZnCa) and found that the degradation rate was still too fast to maintain its mechanical stability for the remodeling process [42]. Additional experiments with MgZnCa in bulk metallic glass form (BMG), which had inherent high strength, good elasticity, and a glassy structure showed that BMG’s allow alloying of higher fractions of elements compared to crystalline Mg [42]. These qualities of BMGs help make it easier to tailor the degradation rate and hydrogen evolution, but the mechanical stability of this material was lacking. Celarek et al. finally showed through their experiments that WZ21 (MgYZnCa) has a high potential for clinical bioresorbability because it possesses a high shear strength, but the material degrades at a rate slower than that desired for clinical applications [42].
Methods for decelerating the corrosion rate of Mg alloys have been investigated for quite some time, but no tests have conclusively proved a method to combat the high amount of blood hemolysis caused by the dissolution of Mg ions. In 2008, Witte et al. highlighted how surface treatments have the best chance at slowing Mg’s high corrosion rate and reducing hemolysis [52]. Witte and colleagues indicated that potential techniques for this include alkaline heat treating, microarc oxidation, phosphate treating, electro deposition, and polymer coating [52]. Tests conducted by Zhang et al. have shown that alloying Mg with a high percentage of Zn helps create a passivation film, providing protection for the material against chloride ions and body fluid, thereby decreasing the rate of corrosion [53]. Properties such as residual stresses or microstructure of the material have also been found to play a significant role in the degradation kinetics of the implant. For Mg alloys in particular, a finer microstructure has been modeled to help decrease the rate of material degradation [2]. Denkena et al. experimentally found that deep rolling an MgCa3.0 alloy decreased its rate of corrosion by a factor of 100 due to an increase in subsurface compressive stresses [2]. Due to the preceding research, an alloy containing Mg and a small amount of Ca appears to have the highest bioresorbable potential, but surface and subsurface modifications are still necessary to enhance Mg’s mechanical properties to reduce chance of brittle fracture while further decreasing hydrogen evolution in order to bring this material up to the clinical standard for hard tissues.
Magnesium – Vascular potential
Magnesium has also shown considerable promise for use as an absorbable metal vascular scaffold (AMS) material. Preliminary human trials for the treatment of critical limb ischemia with magnesium (>90%, alloyed with rare-earth elements) vascular scaffolds showed success in all 20 patients, with a 3-month clinical patency rate of 89.5% and a 12 month patency rate of 72.4% [5,54]. No toxicity was observed in any of the patients, and the limb salvage rate was 94.7% after one year [5]. Schranz et al. implanted a magnesium alloy vascular scaffold (AMS, Biotronik) into the aorta of a 3-week old male patient to treat recoarctation of the aorta [55]. Follow-up angiography revealed that the vessel had begun to return to its original damaged state upon degradation of the magnesium vascular scaffold, requiring implantation of a second scaffold [55]. This suggests that the absorption rate of the magnesium alloy is still too rapid to support the vessel for the duration of the healing process. In spite of the insertion of the second stent, the levels of magnesium in the patient’s blood were not elevated [55]. The Biotronik magnesium alloy vascular scaffold was also tested in the Clinical Performance and Angiographic Results of Coronary Stenting with Absorbable Metal Stents trial [56]. The vascular scaffold was completely absorbed within 2 months, with radial support lost possibly within days of implantation [56]. No deaths, thrombosis, or heart attacks were reported as a result of the stenting, but these vascular scaffolds were associated with a high restenosis rate [56]. Based on this information, it is clear that magnesium vascular scaffolds are biocompatibile, but for many alloys, their high strength is lost too quickly due to their resorbption rate being too rapid causing vessel recoil during the healing process. As a note, strut design is especially important for these highly degrading alloys because pitting or non-uniform breaking down of the struts can significantly decrease the efficacy of the material’s mechanical support, especially if the strut size is too small [16]. Thus, it is ideal to produce a homogenous microstructure in the scaffold.
Heublein et al. implanted six magnesium alloy discs, 200 μm thick and 3 mm in diameter, subcutaneously into rats to assess the corrosion effects and inflammation due to these materials in vivo [57]. The material that produced the least detrimental effects, composed of 2% aluminum and 1% rare earth elements (Ce, Pr, Nd), was then implanted as a coronary vascular scaffold into pigs [57]. No in-stent thrombosis was detected in any of the pigs, while one pig died shortly after implantation due to unknown causes [57]. In contrast, a recent study by Schumacher et al. showed that extruded pure magnesium stimulated an inflammatory response with nasal epithelial cells [58]. Recently, Lock et al. looked into another avenue using MgY, AZ31, and pure Mg being for ureteral stent applications and found the alloys to degrade quite differently in urine environments compared to blood arteries [59].
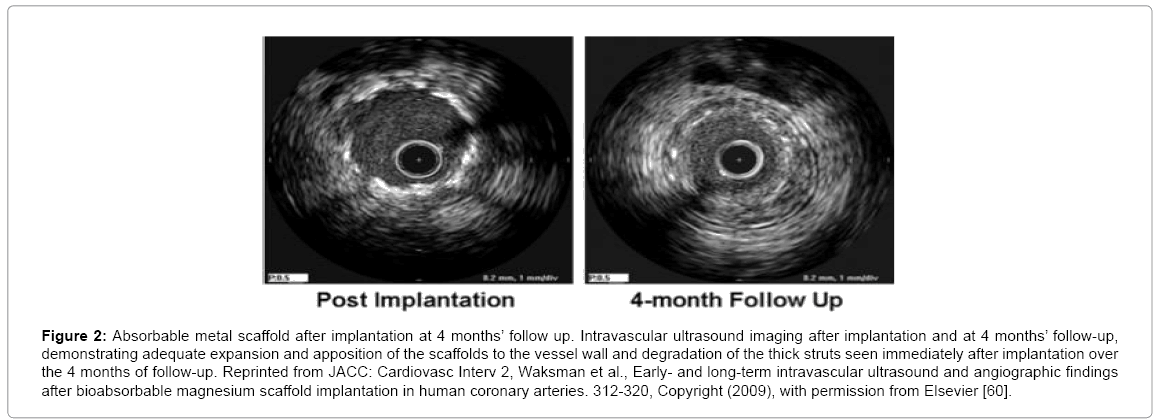
Waksman et al. reported on the implantation of the PROGRESSAMS magnesium vascular scaffold from Biotronik into 63 patients for the treatment of coronary lesions [60]. Ultrasound imaging showed that the scaffolds degraded in about four months, with no adverse effects to the vessel wall, nor calcification observed [60]. Figure 2 shows ultrasound images of the scaffolds at implantation and after 4 months in vivo [60]. Early recoil causes restenosis. Therefore, continuing to improve degradation profiles is necessary in order to make magnesium vascular scaffolds viable candidates for clinical intervention [60].
Figure 2: Absorbable metal scaffold after implantation at 4 months’ follow up. Intravascular ultrasound imaging after implantation and at 4 months’ follow-up, demonstrating adequate expansion and apposition of the scaffolds to the vessel wall and degradation of the thick struts seen immediately after implantation over the 4 months of follow-up. Reprinted from JACC: Cardiovasc Interv 2, Waksman et al., Early- and long-term intravascular ultrasound and angiographic findings after bioabsorbable magnesium scaffold implantation in human coronary arteries. 312-320, Copyright (2009), with permission from Elsevier [60].
In 2005, Zartner et al. implanted a resorbable magnesium vascular scaffold, consisting of less than 10% rare earth elements, into a 6-week old preterm baby, born at 26 weeks gestation [61]. In an attempt to ligate the arterial duct, the left pulmonary artery was unintentionally ligated, resulting in respiratory failure and occlusion of the left pulmonary artery [61]. The left pulmonary artery was sharply bent, preventing angiography past the stenosis, so a resorbable magnesium vascular scaffold was introduced to re-establish perfusion to the lung 15 days after the initial ligation [61]. Re-perfusion was established in the lung, and no toxicity due to the magnesium was observed [61]. In a followup paper, Zartner reported that the baby had contracted pneumonia and died 5 months later [62]. However, autopsy showed that the scaffold had completely resorbed with no traces and no necrosis had occurred [62]. The inner lumen diameter of the left pulmonary artery was 3.7 mm, indicating slight growth after implantation (from 3 mm), while the healthy right pulmonary artery had a diameter of 7 mm [62]. Additional in vivo studies are necessary in order to determine whether this intervention is viable for clinical use.
Hydrogen bubble formation appears to be even more rapid in fastflowing vascular environments, demonstrating the material’s problem of rapid degradation and very short lifetime in vivo [26]. Because of this fast corrosion rate, the radial support may be lost too early, which can result in recoil and restenosis [60]. For these reasons, more work is still needed on magnesium vascular scaffolds to determine the ideal alloy composition and scaffold geometry to ensure the degradation time is sufficient to support the vessel during healing, but rapid enough to prevent late-stent thrombosis and restenosis. Drug-eluting magnesium-based absorbable scaffolds appear to show the greatest promise for this type of application. However, clinical effectiveness is still limited for bare metallic scaffolds [63].
Iron Alloys
Orthopaedic potential
In an almost ironic circumstance, iron, the other resorbable metallic material of choice, has a degradation rate in osteogenic environments found to be excessively slow to be practical for bioresorbable applications [64]. Therefore, an alloying element such as manganese is usually added in an effort to increase iron’s corrosion rate through creation of microgalvanic corrosion sites, while also reducing its magnetic susceptibility. Contrary to tests with magnesium alloys, finer microstructures and thereby larger volumes of high energy grain boundaries in iron alloys appear to increase the corrosion rate [65].
Yuen et al. reported that the daily exposure limits for an average 60-kg adult of Fe and Mn are 2.55 mg and 0.42 mg respectively, which is much lower than Mg [35]. Again, one of the main considerations for future investigations into any metal alloy is to measure the concentrations of degradation products and make sure they are below the renal threshold. Experiments have also shown Fe-Mn alloys displaying antiferromagnetic behavior, which makes it more compatible with MRI scans during in vivo experiments compared to pure iron [66]. Hermawan et al. created a sintered compact of Fe-35Mn and found it to have an ultimate tensile and yield strength of 550+/-8 MPa and 235+/-8 MPa respectively, which is comparable to existing mechanical properties of clinically-used SS316L [66]. Moravej et al. obtained similar yield strength results for their Fe35Mn alloys and explained that the generated porosity and MnO inclusions within the material helped accelerate the degradation of the alloy [65]. Moravej et al. further suggested that modifying the degradation rate could be achieved by altering the microstructure and the concentration of Mn [65]. Interestingly, Liu et al. found that slightly decreased corrosion rates are associated with alloying small amounts of Mn, Al, or B, illuminating a nonlinear response for composition of alloying elements and their effect on corrosion rate [67].
Schaffer et al. conducted a more recent investigation into the biocompatibility and mechanical properties of VIM-melted, extruded, and cold-drawn ferrous wires [68]. More specifically, Schaffer et al. experimented with different amounts of cold worked 99.95% Fe, 316L SS for control, Fe-35Mn, a composite Fe-35Mn-drawn-filledtube (DFT) 25% ZM21, Fe-DFT-25%Mg, and Fe-DFT-57%Mg [68]. Schaffer et al. concluded that the Fe35Mn alloy had the best potential for future bioresorbable studies in both vascular and orthopaedic applications due to its comparable toughness of 30.5 mJ/mm3 to that of 316L stainless steel, and fatigue strengths capable of enduring normal structural functions [68]. Furthermore, Schaffer et al. explains that in order for Fe-Mn alloys to become better suited for soft and hard tissue applications, research needs to be conducted into discovering how variations in the grain size, microstructure, and material composition affects the corrosion susceptibility of Fe-Mn alloys [10].
Besides tests on biocompatibility and corrosion rate, there appears to be a need for further research into better tailoring the surface properties (microstructure, morphology, roughness and surface patterning) to destabilize the iron’s ability to quickly form a thick oxide layer that hampers and slows chloride and media attack. Instead of focusing solely on the corrosion interaction of body media on the implant, another alternative to this issue may be to look at somehow facilitating an increased rate of cellular attack on these oxide layers, potentially increasing the pH slightly around the material to increase degradation rate. Additionally, cell adhesion plays a major role in the degradation rate of these alloys, as attached cells can slow the attack of the surrounding media on the absorbable metal and reduce the degradation rate in vivo considerably. Though, a strong, physical connection between hard tissues and a bioresorbable implant is vital towards promoting osteoblast proliferation and thus encouraging bone growth to replace the implant in the necessary reconstructive timeframe [66]. Future studies on ferrous bioresorbable materials would benefit from further developing high surface area, porous substructures in order to increase the kinetics of corrosion in slowmoving environments such as hard tissues. At the present time, Fe-Mn alloys appear to have mechanical properties similar to that of current permanent orthopaedics and thus have a high clinical potential for beneficial skeletal reconstruction, but still degrade too slowly to be used in transient applications.
Iron – Vascular potential
Iron is an intriguing candidate for a resorbable metal vascular scaffold as it is necessary in trace concentrations in the blood for proper oxygen transport. Peuster et al. first reported on the in vitro and in vivo degradation of pure iron scaffolds in 2001 [64]. Liu et al. also discovered that there were higher cell viabilities for endothelial cells cultured on various Fe alloys than smooth muscle cells, indicating good potential as coronary vascular scaffolds [67].
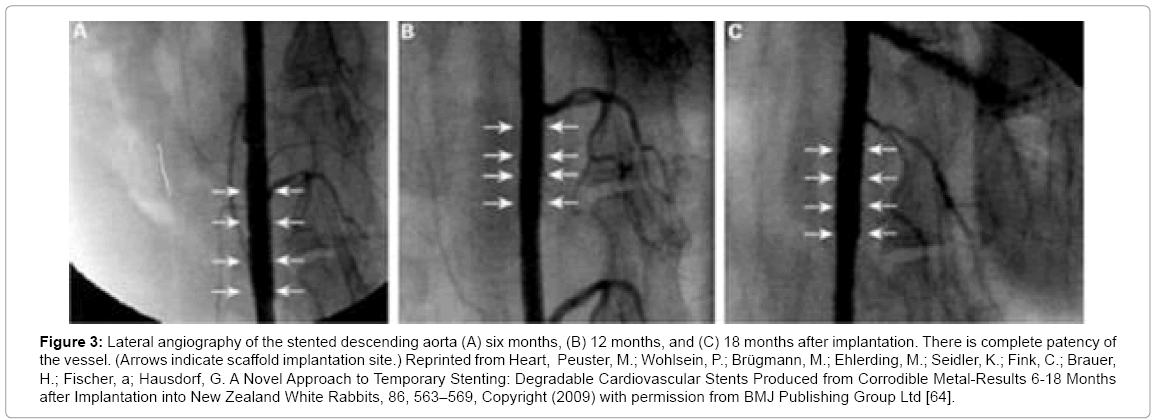
The NOR-I vascular scaffold (pure iron, shown in Figure 3) was implanted into 16 rabbit aortas [64]. Despite the slow degradation rate (struts were still detected 18 months past implantation), there were no cases of thrombosis or death [64-69]. However, the scaffolds caused considerable damage to the tunica media [64,69].
Figure 3: Lateral angiography of the stented descending aorta (A) six months, (B) 12 months, and (C) 18 months after implantation. There is complete patency of the vessel. (Arrows indicate scaffold implantation site.) Reprinted from Heart, Peuster, M.; Wohlsein, P.; Brügmann, M.; Ehlerding, M.; Seidler, K.; Fink, C.; Brauer, H.; Fischer, a; Hausdorf, G. A Novel Approach to Temporary Stenting: Degradable Cardiovascular Stents Produced from Corrodible Metal-Results 6-18 Months after Implantation into New Zealand White Rabbits, 86, 563–569, Copyright (2009) with permission from BMJ Publishing Group Ltd [64].
As mentioned above, iron-manganese alloys have the potential to bridge the gap between pure iron’s slow degradation rates and pure magnesium’s rapid degradation, allowing for tailoring to a more ideal degradation rate [70]. Iron-manganese alloys containing more than 29 wt% Mn are completely austenitic and anti-ferromagnetic, which makes them more MRI compatible than 316L stainless steel [66,70]. An alloy composed of Fe-35Mn has been shown to have good ductility and a yield strength of up to 200 MPa [66]. Compared with pure iron, the Fe-35Mn alloy has a lower corrosion potential and a corrosion rate of almost three times that of pure iron [66]. Compared with 316L, Fe- 35Mn alloys have shown similar toughness and greater tensile strength, suggesting these alloys would provide adequate radial support to the vessel [68]. Preliminary in vitro studies on the endothelial attachment on Fe-35Mn showed a 200% increase in attachment compared with that on 316L [10]. More tests are currently underway to assess the blood compatibility of iron manganese alloys, along with cytotoxicity and cell adhesion. The degradation rate, biocompatibility, and mechanical properties of iron manganese alloys make them an intriguing candidate for resorbable metal scaffolds, but more research is still necessary to determine the utility of these materials for vascular interventions.
Zinc Alloys- Vascular and Orthopaedic Potential
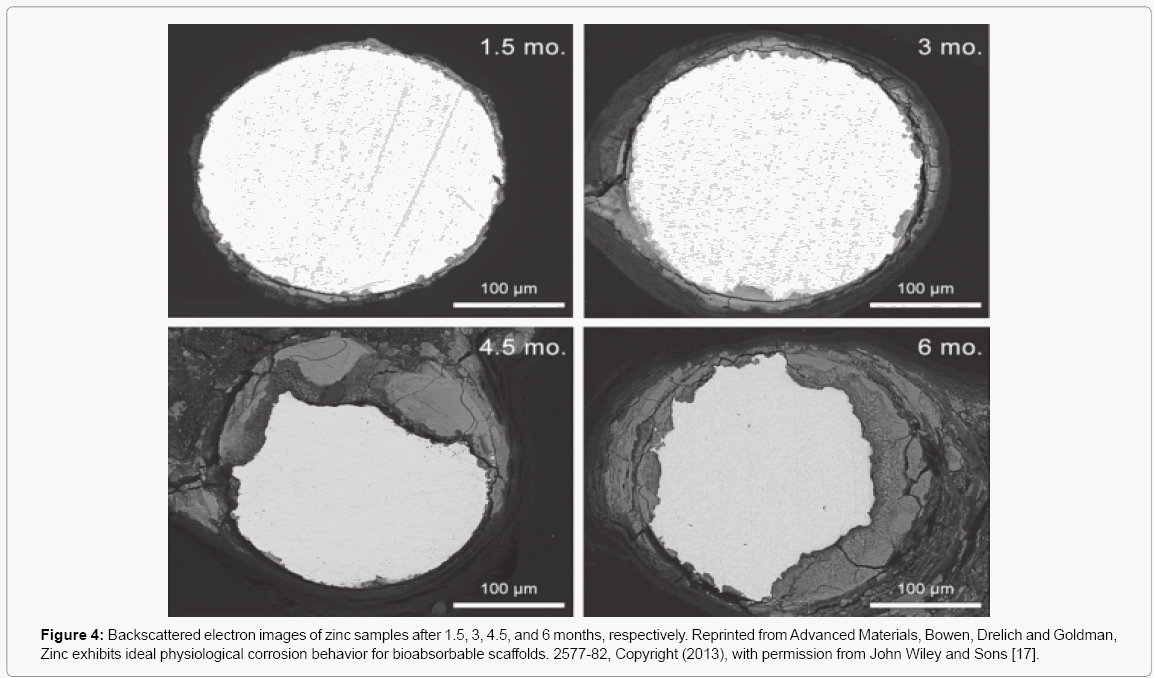
Zinc has come to the attention of researchers in the last few years as a possible vascular scaffold material due to its anti-inflammatory and anti-proliferative properties [17]. Zinc may be effective in reducing the risk of atherosclerosis, as it influences apoptosis of vascular endothelial cells [71]. Ren et al. found that the administration of zinc supplements to New Zealand White rabbits on a high cholesterol diet significantly reduced the size of atherosclerotic lesions compared with rabbits on a high cholesterol diet without zinc, and reduced the levels of Fe detected in the lesions [72]. This could potentially reduce the major problem of in-stent restenosis, which is one of the most common causes of implant failure [73]. It is believed that the zinc stabilizes the membrane of endothelial cells, preventing apoptosis [17]. In a recent study, Bowen et al. found that the cross-sectional area of pure zinc scaffold struts was reduced by >35% after 6 months of implantation in rat aortas [17]. Mechanical integrity of the vascular scaffolds must be maintained for approximately 4 months in order to facilitate vessel healing, and the zinc scaffolds retained about 70% of its cross section at 4 months post-implantation[17]. While zinc has advantages in terms of antiatherogenic properties and degradation rate, it suffers from very low radial strength compared with other alloys [17]. The tensile strength of pure zinc is approximately 120 MPa, while a minimum of 300 MPa is desired to provide adequate support in a blood vessel [17]. Figure 4 from Bowen et al. shows zinc samples after they have been degraded for up to 6 months in vivo [17].
Figure 4: Backscattered electron images of zinc samples after 1.5, 3, 4.5, and 6 months, respectively. Reprinted from Advanced Materials, Bowen, Drelich and Goldman, Zinc exhibits ideal physiological corrosion behavior for bioabsorbable scaffolds. 2577-82, Copyright (2013), with permission from John Wiley and Sons [17].
Pure Zn and Zn-Mg appear to be the only alloys investigated for bone fixation to date, where the latter employs Mg in an attempt to increase the overall corrosion rate, while also increasing the ultimate and yield strengths to make them stronger than bone [37,74]. However, the percent elongation (1-2%) of these materials is still too low to be able to withstand the load forces in orthopaedic applications [74]. In general, pure zinc corrodes much slower than Mg alloys and Vojtech et al. found that by adding small concentrations of Mg (1, 1.5, and 3%Mg), the corrosion rates increased slightly while immersed in SBF [74]. Interestingly enough, Prosek et al. found the corrosion rate to decrease with increasing Mg concentrations in humid air, until reaching Zn- 32Mn where the corrosion rate was even higher than that of pure Mg [37]. Overall, zinc alloys are still relatively new to being added as a class of bioresorbable metallic materials, so significantly more research is needed to determine their vascular scaffold and orthopaedic potential.
Conclusions
Metals possess much higher strengths compared to their polymer counterparts, which leads to better support and resistance to fracture in both orthopaedic and vascular applications. They also display higher toughness, which aids in successful hard tissue screw or pin insertion. Additionally, metals are not affected by creep and stress relaxation in the same magnitude as polymeric materials.
In spite of these advantages, however, specific challenges must be overcome in order for metallic alloys to become clinically viable in the future as degradable biomedical implants. Stress-shielding, for example, continues to be a challenge for higher modulus materials, however, due to the transient nature of these implants and their use more in non-load bearing situations, this may not be a major concern. A more significant challenge stays in the fact that the release rate and concentration of metallic degradation products must be better controlled to eliminate toxic level metal concentrations. Currently, the two major metallic materials that appear to show the greatest potential for orthopaedic applications with a base alloy of magnesium or iron include WZ21 (MgYZnCa) and Fe-35Mn, respectively [42,66,68]. In the case of Mg alloys, the two major obstacles that still need to be overcome include further decreasing the high degradation rate, which should inherently counter the material’s tendency to generate destructive hydrogen bubbles. Conversely, in the case of iron alloys, the rate of degradation must be substantially increased, either by altering the composition of biocompatible alloying elements or by modifying the microstructure and surface substructures to promote more rapid corrosion and inherent instability within the iron oxide layer. Other potential alternatives for increasing degradation rate exist, including manufacturing these materials with higher porosity to increase the surface area, while also making sure the porosity doesn’t detrimentally affect the mechanical properties of the material, thereby increasing surface area and corrosiveness. Zn alloys also need further investigation into methods of increasing their corrosion rates, while also increasing their ultimate tensile, compressive, and yield strengths to support the surrounding tissue. Research into these alloys are still relatively new though. Despite several existing challenges, the future of metallic materials being used for bioresorbable implantation remains promising.
A more complex problem that remains to be identified and agreed upon in literature is the specification of ideal degradation rates for different biomedical devices within the body. It appears at the moment, a degradation limit of anything less than a few years is the unofficial guideline that researchers aim for, as anything that degrades for too long is considered permanent. However, rates of resorbability will differ for vascular and orthopaedic applications, in addition to the tissue healing time variances in different locations within the body. It would be beneficial for scientists in the field to determine target degradation rates for regions of the body so that more accurate comparisons can be better drawn to all past and future experimental corrosion data. These agreed upon goal rates would additionally help in tailoring future bioresorbable materials to the variety of clinical applications currently available.
References
- Pietrzak WS, Sarver D, Verstynen M (1996) Bioresorbable implants--practical considerations. Bone 19: 109S-119S.
- Denkena B, Lucas A (2007) Biocompatible Magnesium Alloys as Absorbable Implant Materials – Adjusted Surface and Subsurface Properties by Machining Processes. CIRP Annals - Manufacturing Technology 56: 113-116.
- Hofmann GO, Wagner FD (1993) New implant designs for bioresorbable devices in orthopaedic surgery. Clin Mater 14: 207-215.
- Viceconti M, Muccini R, Bernakiewicz M, Baleani M, Cristofolini L (2000) Large-sliding contact elements accurately predict levels of bone-implant micromotion relevant to osseointegration. J Biomech 33: 1611-1618.
- Waksman R (2006) Update on bioabsorbable stents: from bench to clinical. J IntervCardiol 19: 414-421.
- Bonan R, Asgar AW (2009) Interventional Cardiology Biodegradable Stents-Where Are We in 2009?.Interventional Cardiology 81-84.
- Feng Q, Zhang D, Xin C, Liu X, Lin W, et al. (2013) Characterization and in vivo evaluation of a bio-corrodible nitrided iron stent. J Mater Sci Mater Med 24: 713-724.
- Savage P, O’Donnell BP, McHugh PE, Murphy BP, Quinn DF (2004) Coronary Stent Strut Size Dependent Stress – Strain Response Investigated Using Micromechanical Finite Element Models. Ann Biomed Eng 32: 202-211.
- Duraiswamy N, Cesar JM, Schoephoerster RT, Moore JE Jr (2008) Effects of stent geometry on local flow dynamics and resulting platelet deposition in an in vitro model. Biorheology 45: 547-561.
- Schaffer JE, Nauman EA, Stanciu LA (2013) Cold drawn bioabsorbable ferrous and ferrous composite wires: an evaluation of in vitro vascular cytocompatibility. ActaBiomater 9: 8574-8584.
- Alexy RD, Levi DS (2013) Materials and manufacturing technologies available for production of a pediatric bioabsorbable stent. Biomed Res Int 2013: 137985.
- Kim K, Yu M, Zong X, Chiu J, Fang D, et al. (2003) Control of degradation rate and hydrophilicity in electrospun non-woven poly(D,L-lactide) nanofiber scaffolds for biomedical applications. Biomaterials 24: 4977-4985.
- Hermawan H, Dubé D, Mantovani D (2010) Developments in metallic biodegradable stents. ActaBiomater 6: 1693-1697.
- Erne P, Schier M, Resink TJ (2006) The road to bioabsorbable stents: reaching clinical reality? CardiovascInterventRadiol 29: 11-16.
- Anselme K, Ponche A, Bigerelle M (2010) Relative Influence of Surface Topography and Surface Chemistry on Cell Response to Bone Implant Materials. Part 2: biological Aspects. ProcInstMechEng H 224: 1487-1507.
- Zheng YF, Gu XN, Witte F (2014) Biodegradable Metals. Materials Science and Engineering: R: Reports 77: 1-34.
- Bowen PK, Drelich J, Goldman J (2013) Zinc exhibits ideal physiological corrosion behavior for bioabsorbable stents. Adv Mater 25: 2577-2582.
- Schinhammer M, Hänzi AC, Löffler JF, Uggowitzer PJ (2010) Design strategy for biodegradable Fe-based alloys for medical applications. ActaBiomater 6: 1705-1713.
- Rodrigues A (2012) Mechanical Properties of Stent Graft Materials. Journal of Materials: Design and Applications.
- Alicea LP, Aviles JI, López IA, Mulero LE, Sánchez LA (2004) Mechanics Biomaterials?: Stents Engineering 1: 1-21.
- Hermawan H, Ramdan D, Djuansjah JRP (2009) Metals for Biomedical Applications.
- Levesque J, Dube D, Fiset M, Mantovani D (2004) Materials and Propertires for Coronary Stents.
- Brar HS, Platt MO, Sarntinoranont M, Martin PI, Manuel MV (2009) Magnesium as a Biodegradable and Bioabsorbable Material for Medical Implants. Jom 61: 31-34.
- Schaffer JE (2012) Development and Characterization of Vascular Prosthetics for Controlled Bioabsorption. Purdue University.
- Kirkland NT (2012) Magnesium Biomaterials: Past, Present and Future. Corrosion Engineering, Science and Technology 47: 322-328.
- Zeng R, Dietzel W, Witte F,Hort N, Blawert C (2008) Progress and Challenge for Magnesium Alloys as Biomaterials. Advanced Engineering Materials 10: B3-B14.
- Lee S, Porter M, Wasko S, Lau G, Chen PY,et al. (2012) Potential Bone Replacement Materials Prepared by Two Methods. MRS Proceedings1418.
- Li Z, Gu X, Lou S, Zheng Y (2008) The development of binary Mg-Ca alloys for use as biodegradable materials within bone. Biomaterials 29: 1329-1344.
- Drogset JO, Grøntvedt T, Myhr G (2006) Magnetic Resonance Imaging Analysis of Bioabsorbable Interference Screws Used for Fixation of Bone-Patellar Tendon-Bone Autografts in Endoscopic Reconstruction of the Anterior Cruciate Ligament. Am J Sports Med 34: 1164-1169.
- Drogset JO, Grøntvedt T, Tegnander A (2005) Endoscopic reconstruction of the anterior cruciate ligament using bone-patellar tendon-bone grafts fixed with bioabsorbable or metal interference screws: a prospective randomized study of the clinical outcome. Am J Sports Med 33: 1160-1165.
- Vaccaro AR, Singh K, Haid R, Kitchel S, Wuisman P, et al. (2003) The use of bioabsorbable implants in the spine. Spine J 3: 227-237.
- Cox S, Mukherjee DP, Ogden AL, Mayuex RH, Sadasivan KK, et al. (2005) Distal TibiofibularSyndesmosis Fixation: A Cadaveric, Simulated Fracture Stabilization Study Comparing Bioabsorbable and Metallic Single Screw Fixation. J Foot Ankle Surg 44: 144-151.
- Maurus PB, Kaeding CC (2004)Bioabsorbable Implant Material Review. Operative Techniques in Sports Medicine 12: 158-160.
- An YH, Woolf SK, Friedman RJ (2000) Pre-clinical in vivo evaluation of orthopaedicbioabsorbable devices. Biomaterials 21: 2635-2652.
- Yuen CK, Ip WY (2010) Theoretical risk assessment of magnesium alloys as degradable biomedical implants. ActaBiomater 6: 1808-1812.
- Zhu S, Huang N, Xu L, Zhang Y, Liu H, et al. (2009) Biocompatibility of Pure Iron: In Vitro Assessment of Degradation Kinetics and Cytotoxicity on Endothelial Cells. Materials Science and Engineering: C 29: 1589-1592.
- Prosek T, Nazarov A, Bexell U, Thierry D, Serak J (2008) Corrosion Mechanism of Model Zinc-Magnesium Alloys in Atmospheric Conditions. Corrosion Science 50: 2216–2231.
- Seitz JM, Eifler R, Bach FW, Maier HJ (2014) Magnesium degradation products: effects on tissue and human metabolism. J Biomed Mater Res A 102: 3744-3753.
- Gibson LJ (1985) The mechanical behaviour of cancellous bone. J Biomech 18: 317-328.
- Wen CE, Yamada Y, Shimojima K, Chino Y, Hosokawa H,et al. (2004) Compressibility of Porous Magnesium Foam: Dependency on Porosity and Pore Size. Materials Letters 58: 357-360.
- Shaw BA, Sikora E, Virtanen S (2008) Fix , Heal , and Disappear?: A New Approach to Using Metals in the Human Body 45-49.
- Celarek A, Kraus T, Tschegg EK, Fischerauer SF, Stanzl-Tschegg S, (2012) Crystalline and Amorphous Magnesium Alloys: Promising Candidates for BioresorbableOsteosynthesis Implants? Mater SciEng C 32: 1503-1510.
- Gill P (2012)Corrosionand Biocompatibility Assessment of Magnesium Alloys. J BiomaterNanobiotechnol 03: 10-13.
- Li Y, Rao G, Rong L, Li Y (2002) The Influence of Porosity on Corrosion Characteristics of Porous NiTi Alloy in Simulated Body Fluid. Materials Letters 57: 448-451.
- Nasab MB, Hassan MR (2010) Metallic Biomaterials of Knee and Hip - A Review.
- Witte F, Kaese V, Haferkamp H, Switzer E, Meyer-Lindenberg A, et al.(2005) In Vivo Corrosion of Four Magnesium Alloys and the Associated Bone Response. Biomaterials 26: 3557-3563.
- Hampp C, Angrisani N, Reifenrath J, Bormann D, Seitz JM, et al. (2013) Evaluation of the biocompatibility of two magnesium alloys as degradable implant materials in comparison to titanium as non-resorbable material in the rabbit. Mater SciEng C Mater BiolAppl 33: 317-326.
- Huehnerschulte TA, Reifenrath J, von Rechenberg B, Dziuba D, Seitz JM, et al. (2012) In vivo assessment of the host reactions to the biodegradation of the two novel magnesium alloys ZEK100 and AX30 in an animal model. Biomed Eng Online 11: 14.
- Dziuba D, Meyer-Lindenberg A, Seitz JM, Waizy H, Angrisani N, et al. (2013) Long-term in vivo degradation behaviour and biocompatibility of the magnesium alloy ZEK100 for use as a biodegradable bone implant. ActaBiomater 9: 8548-8560.
- Wang Y, He Y, Zhu Z, Jiang Y, Zhang J, et al. (2012) In Vitro Degradation and Biocompatibility of Mg-Nd-Zn-ZrAlloy. Chinese Sci Bull 57: 2163-2170.
- Xia Y, Zhang B, Wang Y, Qian M, Geng L (2012) In-Vitro Cytotoxicity and in-Vivo Biocompatibility of as-Extruded Mg–4.0Zn–0.2Ca Alloy. Mater SciEng C 32: 665-669.
- Witte F, Hort N, Vogt C, Cohen S, Kainer KU, et al.(2008) Degradable Biomaterials Based on Magnesium Corrosion. CurrOpin Solid State Mater Sci 12: 63-72.
- Zhang E, Yin D, Xu L, Yang L, Yang K (2009) Microstructure, Mechanical and Corrosion Properties and Biocompatibility of Mg–Zn–Mn Alloys for Biomedical Application. Mater SciEng C 29: 987-993.
- Peeters P, Bosiers M, Verbist J, Deloose K, Heublein B (2005) Preliminary results after application of absorbable metal stents in patients with critical limb ischemia. J EndovascTher 12: 1-5.
- Schranz D, Zartner P, Michel-Behnke I, Akintürk H (2006) Bioabsorbable metal stents for percutaneous treatment of critical recoarctation of the aorta in a newborn. Catheter CardiovascInterv 67: 671-673.
- Ormiston JA, Serruys PW (2009) Bioabsorbable coronary stents. CircCardiovascInterv 2: 255-260.
- Heublein B, Rohde R, Kaese V, Niemeyer M, Hartung W, et al. (2003) Biocorrosion of magnesium alloys: a new principle in cardiovascular implant technology? Heart 89: 651-656.
- Schumacher S, Roth I, Stahl J, Bäumer W, Kietzmann M (2014) Biodegradation of metallic magnesium elicits an inflammatory response in primary nasal epithelial cells. ActaBiomater 10: 996-1004.
- Lock JY, Wyatt E, Upadhyayula S, Whall A, Nuñez V,et al. (2014) Degradation and Antibacterial Properties of Magnesium Alloys in Artificial Urine for Potential Resorbable Ureteral Stent Applications. J Biomed Mater Res - Part A 102: 781-792.
- Waksman R, Erbel R, Di Mario C, Bartunek J, de Bruyne B, et al.(2009) Early- and Long-Term Intravascular Ultrasound and Angiographic Findings after Bioabsorbable Magnesium Stent Implantation in Human Coronary Arteries. JACC CardiovascInterv 2: 312-320.
- Zartner P, Cesnjevar R, Singer H, Weyand M (2005) First Successful Implantation of a Biodegradable Metal Stent into the Left Pulmonary Artery of a Preterm Baby. Catheter CardiovascInterv 66: 590-594.
- Zartner P, Buettner M, Singer H, Sigler M (2007) First Biodegradable Metal Stent in a Child with Congenital Heart Disease: Evaluation of Macro and Histopathology. Catheter CardiovascInterv 69: 443-446.
- Kitabata H, Waksman R, Warnack B (2014) Bioresorbable metal scaffold for cardiovascular application: current knowledge and future perspectives. CardiovascRevasc Med 15: 109-116.
- Peuster M, Wohlsein P, Brügmann M, Ehlerding M, Seidler K,et al. (2001) A Novel Approach to Temporary Stenting: Degradable Cardiovascular Stents Produced from Corrodible Metal-Results 6-18 Months after Implantation into New Zealand White Rabbits. Heart 86: 563-569.
- Moravej M, Mantovani D (2011) Biodegradable metals for cardiovascular stent application: interests and new opportunities. Int J MolSci 12: 4250-4270.
- Hermawan H, Alamdari H, Mantovani D, Dubé D (2008) Iron–manganese: New Class of Metallic Degradable Biomaterials Prepared by Powder Metallurgy. Powder Metall 51: 38-45.
- Liu B, Zheng YF (2011) Effects of alloying elements (Mn, Co, Al, W, Sn, B, C and S) on biodegradability and in vitro biocompatibility of pure iron. ActaBiomater 7: 1407-1420.
- Schaffer JE, Nauman EA, Stanciu LA (2012) Cold-Drawn Bioabsorbable Ferrous and Ferrous Composite Wires: An Evaluation of Mechanical Strength and Fatigue Durability. Metallurgical and Materials Transactions B 43: 984-994.
- Mario D, Griffiths HUW, Peeters P, Verbist JAN, Bosiers M, et al.(2004) Future Devices?:Bioabsorbable Stents. The British Journal of Cardiology 80-84.
- Hermawan H, Purnama A, Dube D, Couet J, Mantovani D (2010) Fe-Mn alloys for metallic biodegradable stents: degradation and cell viability studies. ActaBiomater 6: 1852-1860.
- Hennig B, Toborek M, Mcclain CJ (1996) Antiatherogenic properties of zinc: implications in endothelial cell metabolism. Nutrition 12: 711-717.
- Ren M, Rajendran R, Ning P, Tan KwongHuat B, Choon Nam O, et al. (2006) Zinc supplementation decreases the development of atherosclerosis in rabbits. Free RadicBiol Med 41: 222-225.
- Berger M, Rubinraut E, Barshack I, Roth A, Keren G, et al. (2004) Zinc reduces intimal hyperplasia in the rat carotid injury model. Atherosclerosis 175: 229-234.
- Vojtěch D, Kubásek J, Serák J, Novák P (2011) Mechanical and corrosion properties of newly developed biodegradable Zn-based alloys for bone fixation. ActaBiomater 7: 3515-3522.
- Schinhammer M, Steiger P, Moszner F, Löffler JF, Uggowitzer PJ (2013) Degradation performance of biodegradable Fe-Mn-C(-Pd) alloys. Mater SciEng C Mater BiolAppl 33: 1882-1893.
- Hermawan H, Moravej M, Dubé D, Fiset M, Mantovani D (2007) Degradation Behaviour of Metallic Biomaterials for Degradable Stents. Advanced Materials Research 15-17: 113-118.
- Wen Z, Wu C, Dai C, Yang F (2009) Corrosion Behaviors of Mg and Its Alloys with Different Al Contents in a Modified Simulated Body Fluid. Journal of Alloys and Compounds 488: 392-399.
- Gu XN, Zheng YF (2010) A Review on Magnesium Alloys as Biodegradable Materials. Frontiers of Materials Science in China 4: 111-115.
- Zhang S, Zhang X, Zhao C, Li J, Song Y, et al. (2010) Research on an Mg-Zn alloy as a degradable biomaterial. ActaBiomater 6: 626-640.
- Hermawan H, Dubé D, Mantovani D (2010) Degradable metallic biomaterials: design and development of Fe-Mn alloys for stents. J Biomed Mater Res A 93: 1-11.
- Witte F, Feyerabend F, Maier P, Fischer J, Störmer M, et al. (2007) Biodegradable magnesium-hydroxyapatite metal matrix composites. Biomaterials 28: 2163-2174.
- ZainalAbidin NI, Martin D, Atrens A (2011) Corrosion of High Purity Mg, AZ91, ZE41 and Mg2Zn0.2Mn in Hank’s Solution at Room Temperature. Corrosion Science 53: 862-872.
- Shi Z, Atrens A (2011)An Innovative Specimen Configuration for the Study of Mg Corrosion. Corrosion Science 53: 226-246.
- Gu XN, Li XL, Zhou WR, Cheng Y, Zheng YF (2010) Microstructure, Biocorrosion and Cytotoxicity Evaluations of Rapid Solidified Mg-3Ca Alloy Ribbons as a Biodegradable Material. Biomed Mater5: 035013.
- Cao JD, Kirkland NT, Laws KJ, Birbilis N, Ferry M (2012) Ca-Mg-Zn bulk metallic glasses as bioresorbable metals. ActaBiomater 8: 2375-2383.
- Heiden M, Walker E, Nauman E, Stanciu L (2015) Evolution of novel bioresorbable iron-manganese implant surfaces and their degradation behaviors in vitro. J Biomed Mater Res A 103: 185-193.
- Heiden M, Kustas A, Chaput K, Nauman E, Johnson D,et al. (2015) Effect of Microstructure and Strain on the Degradation Behavior of Novel Bioresorbable Iron-Manganese Alloy Implants. Journal of Biomedical Materials Research Part A 103: 738–745.
Relevant Topics
- Agricultural biotechnology
- Animal biotechnology
- Applied Biotechnology
- Biocatalysis
- Biofabrication
- Biomaterial implants
- Biomaterial-Based Drug Delivery Systems
- Bioprinting of Tissue Constructs
- Biotechnology applications
- Cardiovascular biomaterials
- CRISPR-Cas9 in Biotechnology
- Nano biotechnology
- Smart Biomaterials
- White/industrial biotechnology
Recommended Journals
Article Tools
Article Usage
- Total views: 18416
- [From(publication date):
August-2015 - Jul 12, 2025] - Breakdown by view type
- HTML page views : 13507
- PDF downloads : 4909