Review Article Open Access
Lymphocytic Esophagitis: A Newly Recognized Mimic of Eosinophilic Esophagitis
Vipul R Nayi1 and David A. Johnson2*
1Montefiore Medical Center Bronx NY, USA
2Professor of Medicine/Chief of Gastroenterology, Eastern VA Medical School, Norfolk VA, USA
- *Corresponding Author:
- David A. Johnson
Professor of Medicine/Chief of Gastroenterology
Eastern VA Medical School, Norfolk VA, USA
Tel: 7576416685
Fax: 7574405713
E-mail: dajevms@aol.com
Received date: November 4, 2015 Accepted date: November 27, 2015 Published date: December 04, 2015
Citation:Nayi VR, Johnson DA (2015) Lymphocytic Esophagitis: A Newly Recognized Mimic of Eosinophilic Esophagitis. J Gastrointest Dig Syst 5:357. doi:10.4172/2161-069X.1000357
Copyright: © 2015 Nayi VR, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Lymphocytic Esophagitis (LyE) is a type of chronic esophagitis defined by three histologic characteristics: 1) dense peripapillary lymphocytic infiltrates in the esophageal squamous mucosa (termed Peripapillary Lymphocytosis), 2) little to no i ntraepithelial granulocytes within these areas of focus and 3) the presence of spongiosis, or intercellular edema, of the squamous epithelial cells specifically in the areas of focus. This condition has a higher predominance in white females. Patients typically present with symptoms of dysphagia, chest/ abdominal pain and heartburn. Common endoscopic features of LyE include esophagitis, strictures and stenosis, but there is a large portion of patients with a normal appearing esophagus. One technique that shows promise in increasing detection and decreasing sampling error is narrow-band imaging magnifying endoscopy (NBI-ME). Currently, there is no research guiding treatment for LyE, but proton pump inhibitors and swallowed corticosteroids have been used in the past.
Keywords
Lymphocytic esophagitis; Eosinophilic esophagitis; Esophageal stricture
Introduction
There has been very little information published regarding a new subtype of chronic esophagitis, termed Lymphocytic Esophagitis (LyE). It was described in 2006 as an increase in lymphocytic infiltration within the distal two-thirds of the esophagus [1]. This definition is similar to that of another chronic esophagitis, eosiniophilc esophagitis (EoE), but is specific to a different immune cell type.
Signs and Symptoms
Although not a complete list, the most frequent symptoms of patients who are diagnosed with LyE are: dysphagia, chest/abdominal pain and heartburn/reflux [2-10]. The rates of patients presenting with dysphagia and subsequently diagnosed with LyE are comparable to patients with dysphagia diagnosed with EoE. One difference noted, was that LyE patients typically didn’t present with food impaction [10]. There have been few reports of more serious symptoms in patients with LyE. One case report of a 35-year-old female who presented with chest pain, fever and hemodynamic shock was found to have diffuse thickening of the esophagus with bilateral pleural effusions, thought to be due to microperforation of the esophagus. Of note, she endorsed mild odynophagia following her most recent meal along with an acute non-productive cough. Upper endoscopy performed one week after the acute event was unremarkable, but biopsies from the mid and distal esophagus showed large numbers of intramucosal peripapillary lymphocytes along with spongiosis, with a lack of eosinophils, viral inclusions or dysplastic/neoplastic lesions. Workup for autoimmune and chronic inflammatory disease was negative. This case study is one of the first to describe a potentially lethal diagnosis of spontaneous esophageal perforation in which LyE might have played a role [4].
Endoscopic Features
Histopathologic characterization is what defines LyE, but the endoscopic view of the esophagus will be the endoscopists’ gateway into making the diagnosis. Studies have shown that esophagitis was present only 18-24% of the time [2,8], with strictures appearing 10.1% [2] and narrow-caliber/stenosis seen in 36% of patients with LyE3. Interestingly, about 30% of patients with a normal looking esophagus were ultimately diagnosed with LyE [2,8]; this highlights the importance of biopsy in making this diagnosis, and not only relying on gross appearance. Trying to differentiate between EoE and LyE based on a gross view of the esophagus can be challenging. Researchers have reported that about 70% of patients diagnosed with LyE had at least 1 feature suggestive of EoE on esophagogastroduodenoscopy (felinization with furrows, white plaques and strictures) [3]. As mentioned above, gross endoscopic features may not always provide a clear picture as to what is truly occurring within the esophagus. One study recommends using narrow-band imaging magnifying endoscopy (NBI-ME) in order to improve detection rates of LyE and EoE [3]. NBI-ME is commonly used to assess invasiveness of superficial esophageal cancers by visualization of intrapapillary capillary loops (IPCLs). These researchers demonstrated that patients with LyE and EoE were found to have at least 1 of the following characteristics on NBI-ME:
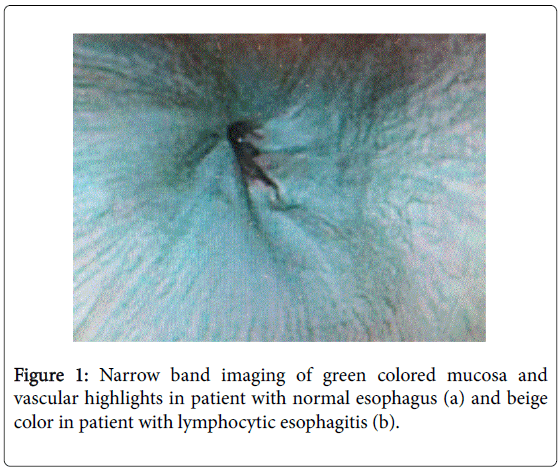
1. Beige color (normal color of the esophagus is light green) shown in Figure 1.
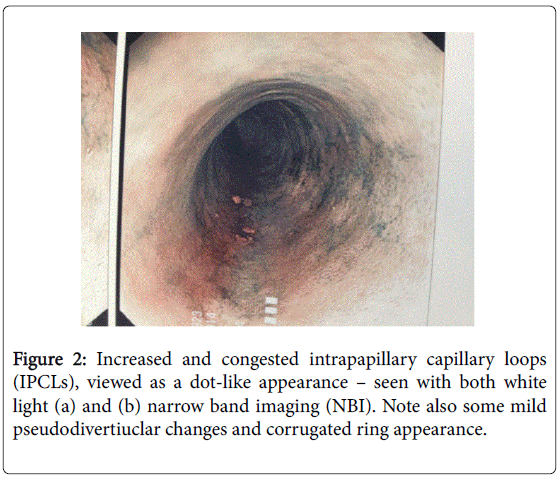
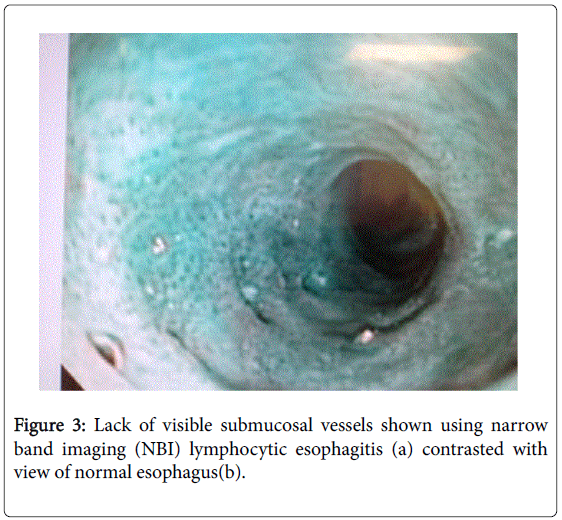
2. Increased and congested intrapapillary capillary loops (IPCLs), viewed as a dot-like appearance – seen with both white light (Figure 2) and narrow band imaging (NBI) (Figure 3).
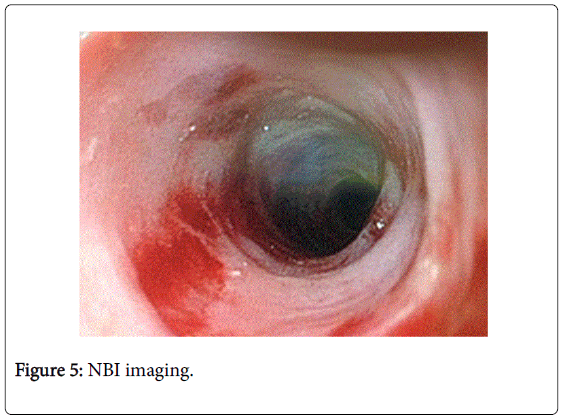
3. Lack of visible submucosal vessels. Figures 2 and 3 (same as above) and normal esophagus seen in Figure 4 (standard white light) and Figure 5 (NBI imaging).
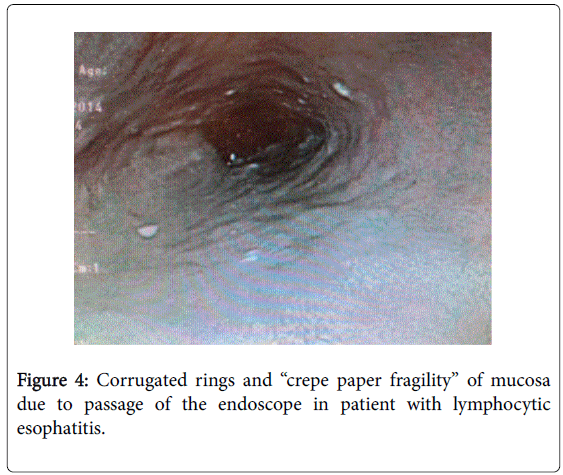
Additionally, in our experience, these LyE patients exhibit the same “crepe paper fragility” of the mucosa, similar to what has been described with EoE (Figure 4). Patients with gastroesophageal reflux disease (GERD) did not exhibit any of these features [3]. Therefore, this technique could be helpful in differentiating between LyE/EoE from GERD, and assist with biopsy locations within the esophagus in order to reduce sampling error.
Diagnostic Criteria
A diagnosis of LyE must meet 3 histological characteristics: 1) dense peripapillary lymphocytic infiltrates in the esophageal squamous mucosa (termed Peripapillary Lymphocytosis), 2) little to no intraepithelial granulocytes (neutrophils, eosinophils) within these areas of focus and 3) the presence of spongiosis, or intercellular edema, of the squamous epithelial cells specifically in the areas of focus [2]. The exact number of lymphocytes present to satisfy the first requirement has varied across different studies, with minimum cutoffs set as low as 30 per high power field 2 up to 50 per high power field [5,6]. The study that originally used 30 intraepithelial lymphocytes (IELs) per high power field concluded that having a minimum cutoff could be misleading and would not increase the specificity of making the diagnosis; the researchers felt that that the focus should rather lie in the distribution of the lymphocytes rather than the sheer number [2].
Pathophysiology
Unfortunately, there is not much known regarding the pathophysiology of this condition. One group of researchers hypothesized that since lymphocytic esophagitis is histologically similar to acute spongiotic dermatitis (such as allergic contact dermatitis, irritant contact dermatitis and atopic dermatitis), the cause of LyE may have an allergic or irritant component [8]. Unfortunately, their study found no statistically significant non-drug allergy or drug allergy association in patients diagnosed with LyE [8]. Although the origin of LyE is currently unknown, further research into this condition will provide a greater insight as to how and why it develops. To date, there have been no specific testing pH monitoring evaluations for GERD in this population.
Incidence and Demographics
One of the largest studies done that included a little less than one hundred and thirty thousand patients showed that about 0.1% of patients who had esophageal biopsies, satisfied the criteria for lymphocytic esophagitis [2]. This incidence has been increasing over time, with the majority of patients being diagnosed within the last 3 years (most likely due to increased recognition, but an increase in the number of cases or number of esophageal biopsies taken cannot be ruled out) [10]. LyE can be found in both children and adults, with the average age of patients being 51 years old [10]. Both men and woman are at risk of developing this condition.
Unlike eosinophilic esophagitis, which is more likely to be seen in males, lymphocytic esophagitis has a higher predominance in females [2,10]. Also, an overwhelming majority of these patients are white [10].
Associated Conditions
Of the few studies done focusing on LyE, most have tried to find associated conditions but have failed. So far, there has been no associations between LyE and allergies (drug and non-drug), H. pylori gastritis or celiac disease8; the association between LyE and Crohn’s disease is still controversial. One of the earlier studies done found that about 40% of patients with LyE also had Crohn’s disease [1]. Subsequent studies have failed to show a statistically significant association, but interestingly, these studies were all done in adults [2,5]. When looking back at the original study that demonstrated an association, about half of the patients with LyE were less than seventeen years old. Two newer studies done focusing on only pediatric patients, both found statistically significant associations between LyE and Crohn’s disease [6,9]. One even went as far to say that when LyE is found in a pediatric patient with Crohn’s disease, it is more likely to be an upper gastrointestinal manifestation of Crohn’s disease rather than another, separate entity [6].
Labs
There are no serum biomarkers currently known to correlate with LyE. A smaller study had found that patients with peripapillary lymphocytosis, one of criteria of LyE, were associated with higher inflammatory markers such as erythrocyte sedimentation rate and C-reactive protein [5]. More research in this area is needed to determine if these tests would be useful clinically in this setting.
Treatment
Treatment options for LyE have not been well studied or defined. Given one of the main symptoms of LyE being heartburn, proton pump inhibitors (PPI) have been prescribed to patients. One study found that about half of patients diagnosed with LyE felt improvement of their initial symptoms after starting a PPI, although it was unsure if there was concomitant GERD that was being treated. It is not clear if there will be a PPI lymphocyte responsive subset of patients as was seen in the PPI responsive EoE patients [11]. Similarly there has not been a dietary exclusion trial assessment for clinical success as has been shown with EoE [12]. Others have tried esophageal dilation and topical swallowed steroids, which are similar treatments for other forms of esophagitis [7].
Natural History
Although extremely limited data is available, the course of this disease appears to be favorable. Almost 90% of patients with LyE were still living three years after being diagnosed [10]. Most patients report a good quality of life and satisfaction with their health at follow-up visits within three years post diagnosis [10]. Only about 33% of patients with LyE had visited the emergency room with a gastrointestinal complaint [10].
Conclusion
This emerging condition still has a long way to go before it is fully understood. With the increase in incidence of LyE, more physicians will hopefully become familiar with the disease. NBI-ME shows promise in assisting with biopsy locations in order to help sampling error. One area specifically that needs greater clarity is the relationship between LyE and Crohn’s disease in the pediatric population and GERD among all patients. Greater knowledge regarding the pathophysiology of this condition will shed insight into potential treatment strategies in the future.
References
- Rubio CA, Sjodahl K, Lagergren J (2006) Lymphocytic esophagitis: a histologic subset of chronic esophagitis. Am J Clin Pathol 125: 432-437.
- Haque S, Genta RM (2012) Lymphocytic oesophagitis: clinicopathological aspects of an emerging condition. Gut 61: 1108-1114.
- Tanaka K, Rubio CA, Dlugosz A, Truskaite K, Befrits R, et al. (2013) Narrow-band imaging magnifying endoscopy in adult patients with eosinophilic esophagitis/esophageal eosinophilia and lymphocytic esophagitis. Gastrointest Endosc 78: 659-664.
- Hendy PJ, Wong DS, Florin TH (2013) Spontaneous oesophageal perforation: an unreported complication of lymphocytic oesophagitis. Gut 62: 1668-1669.
- Basseri B, Vasiliauskas EA, Chan O, Wang HL, Basseri RJ1, et al. (2013) Evaluation of peripapillary lymphocytosis and lymphocytic esophagitis in adult inflammatory bowel disease. Gastroenterol Hepatol (N Y) 9: 505-511.
- Sutton LM, Heintz DD, Patel AS, Weinberg AG (2014) Lymphocytic esophagitis in children. Inflamm Bowel Dis 20: 1324-1328.
- Figueiredo PC, Pinto-Marques P, Borralho P, Freitas J (2014) Unusual cause for smoldering dysphagia. Lymphocytic esophagitis. Dysphagia 29: 283-285.
- Purdy JK, Appelman HD, Golembeski CP, McKenna BJ (2008) Lymphocytic esophagitis: a chronic or recurring pattern of esophagitis resembling allergic contact dermatitis. Am J Clin Pathol 130: 508-513.
- Ebach DR, Vanderheyden AD, Ellison JM, Jensen CS (2011) Lymphocytic esophagitis: a possible manifestation of pediatric upper gastrointestinal Crohn's disease. Inflamm Bowel Dis 17: 45-49.
- Cohen S, Saxena A, Waljee AK, Piraka C, Purdy J, et al. (2012) Lymphocytic esophagitis: a diagnosis of increasing frequency. J Clin Gastroenterol 46: 828-832.
- Dellon ES, Speck O, Woodward K, Gebhart JH, Madanick RD, et al. (2013) Clinical and endoscopic characteristics do not reliably differentiate PPI-responsive esophageal eosinophilia and eosinophilic esophagitis in patients undergoing upper endoscopy: a prospective cohort study. Am J Gastroenterol 108: 1854-1860.
- Arias A, González-Cervera J, Tenias JM, Lucendo AJ (2014) Efficacy of dietary interventions for inducing histologic remission in patients with eosinophilic esophagitis: a systematic review and meta-analysis. Gastroenterology 146: 1639-1648.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 24661
- [From(publication date):
December-2015 - Apr 04, 2025] - Breakdown by view type
- HTML page views : 23456
- PDF downloads : 1205