Lymphedema In A Patient With Decompensated Cirrhosis
Received: 01-Mar-2024 / Manuscript No. science-24-127665 / Editor assigned: 03-Mar-2024 / PreQC No. science-24-127665 / Reviewed: 17-Mar-2024 / QC No. science-24-127665 / Revised: 19-Mar-2024 / Manuscript No. science-24-127665 / Accepted Date: 24-Mar-2024 / Published Date: 25-Mar-2024 QI No. / science-24-127665
Abstract
The lymphatic system is critical in body fluid homeostasis. Although lymphatic vascular expansion prevents the development of ascites and edema in the early stages of liver cirrhosis, compensatory mechanisms cannot achieve this in the advanced stages due to lymphatic dysfunction. A 36-year-old male patient, who had been followed up for cryptogenic cirrhosis for 15 years, had been complaining of excessive swelling in his legs for the last 4 years. Excessive swelling in the legs was accompanied by skin rashes and ulcers, and the leg skin had an orange peel appearance observed in lymphedema. Bilateral lower extremity artery and venous system color doppler ultrasonography showed that the vascular structures of the right lower extremity arterial and venous system were open and the flow rate, direction and spectrum are normal. The patient, who could not undergo liver transplantation due to organ limitations, died due to sepsis following lymphedema-induced wound infection. In conclusion, this case suggests that lymphedema should be considered in the presence of edema in cases of decompensated cirrhosis and the necessary conservative treatments should be applied.
Keywords
Cirrhosis; Lymphedema
Introduction
Ascites and hepatic edema are major complications observed in patients with decompensated cirrhosis and are associated with increased morbidity [1] and poor quality of life [2]. The lymphatic vascular system plays a critical role in ascites formation. The lymphatic vascular system removes interstitial fluid from tissues in the body and returns it to the bloodstream. Failure of normal lymphatic function results in a build-up of interstitial fluid and can lead to the lymphedema and ascites [3].
Liver is the largest lymph-producing organ, generating 25% to 50% of the lymph flowing through the thoracic duct [4] Recent studies have suggested that progression of liver disease causes structural and functional changes in both hepatic and extrahepatic lymphatic vessels. This suggests a possible link between lymphatic vessel changes and disease progression [5,6]. In this case report, we aim to present the lymphedema we encountered in a patient with cirrhosis.s
Case Report
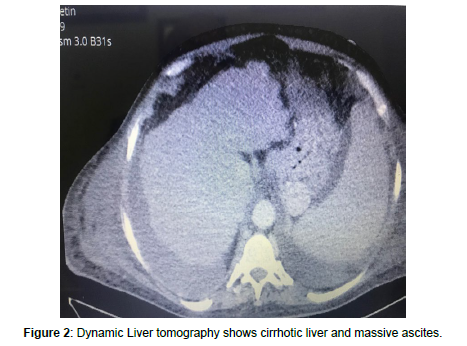
A 36-year-old male patient, who had been followed up for cryptogenic cirrhosis for 15 years, had been complaining of excessive swelling in his legs for the last 4 years. Excessive swelling in the legs was accompanied by skin rash and ulcers (Figure 1). His sister underwent a living donor liver transplantation due to cryptogenic liver cirrhosis. The patient had been hospitalized twice before with the same complaint and had undergone debridement surgery at the plastic surgery department due to the wounds on his legs. In the last abdominal ultrasound examination, it was determined that the liver had a heterogeneous parenchymal echo and its contours were lobulated (chronic liver disease), the size of the spleen increased (16 cm) and there was massive ascites. Bilateral lower extremity artery and venous system color doppler ultrasonography showed that the vascular structures of the right lower extremity arterial and venous system were open and the flow rate, direction and spectrum are normal. In the examination area, the subcutaneous tissue thickness is increased and edematous in bilateral thigh and leg sections. Figure 2 shows cirrhotic liver and massive ascites on dynamic liver tomography.
His laboratory values were creatinine.1.4. mg/dL, total bilirubine 11.95 mg/dL, direct bilirubine 7.19 mg/dL, prothrombin time INR 1.45 ,NA(SODYUM):131 mmol/L, Albumine 1.4 G/DL,Kolesterol:52 MG/DL,,tg:96 MG/DL vldl 19.2. HBsAg and Anti-HCV were negative. MELD-Na and Child-Pugh scores 26 and 11, respectively. Liver transplantation was planned due to decompensated cirrhosis. However, cadaveric or living donor liver transplantation could not be performed due to organ limitations. Cultures taken from the wounds on his legs grew Klebsiella pneumoniae and Pseudomonas aeruginosa bacteria. The patient did not respond to antibiotic treatments in the intensive care unit and died due to sepsis.
Discussion
Ascites and edema are common in patients with decompensated cirrhosis. Since lymphedema is rare, it is generally considered as classical edema in this patient group at first and is not brought to mind. In addition, lymphedema is generally considered an untreatable and resistant chronic problem. All of these may lead to diagnostic delays. To diagnose lymphedema, attention should be paid to the patient’s risk factors and specific findings on physical examination [2]. Peripheral lymphedema manifests itself physically as an orange peel appearance on the skin, as seen in Figure 3.
The lymphatic system is critical in body fluid homeostasis, adaptive immunity, and transport of lipids. In patients with liver cirrhosis, capillary filtration increases markedly due to an increase in hydrostatic pressure, resulting in increased lymph production. In the early stages, expansion of the lymphatic vascular system attempts to prevent fluid accumulation by returning fluid to the systemic circulation. However, with the progression of cirrhosis, lymphatic functions become compromised and, as a result, the lymphatic compensatory mechanism becomes overloaded, contributing to the development and eventual worsening of ascites and edema [2]. Additionally, there are studies reporting that the progression of liver disease is accompanied by changes in hepatic and extrahepatic lymphatic vessels [5]. Although there are very few publications on lymphedema in patients [2] with cirrhosis, the frequency of peripheral lymphedema in patients with cirrhosis and refractory ascites was reported as 33.5% in one study [1]. The paucity of literature on lymphedema in patients with cirrhosis is probably due to the fact that patients are considered to have classical edema and are less noticed, and the difficulties in the diagnosis and treatment of lymphedema.
In the treatment of lymphedema, intensive bandaging and lymphatic massage are essential, as well as the use of compression clothing. Surgical interventions may be required in cases that do not respond to conservative treatments.7 Our case had to undergo surgery twice due to deep ulcers. Patients with lymphedema are more prone to cellulite due to their deep fissures, stagnant lymph and weak immunity.9 Our case with decompensated cirrhosis also died due to sepsis following lymphedema-induced wound infection.
Conclusion
In conclusion, this case suggests that slymphedema should be considered in the presence of edema in cases of decompensated cirrhosis and the necessary conservative treatments should be applied.
References
- Pallone F, Monteleone G (1998) Interleukin 12 and Th1 responses in inflammatory bowel disease. Gut 43: 735-736.
- Duchmann R, Kaiser I, Hermann E, Mayet W, Ewe K, et al. (1995) Tolerance exists towards resident intestinal flora but is broken in active inflammatory bowel disease (IBD). Clin Exp Immunol 102: 448-455.
- Strober W, Kelsall B, Fuss I, Marth T, Ludviksson B, et al. (1997) Reciprocal IFN-γ and TGF-β responses regulate the occurrence of mucosal inflammation. Immunol Today 18: 61- 64.
- Elson CO, Sartor RB, Tennyson GS, Riddell RH (1995) Experimental models of inflammatory bowel disease. Gastroenterology 109: 1344-1367.
- Melmed GY, Ippoliti AF, Papadakis KA, Tran TT, Birt JL, et al. (2006) Patients with inflammatory bowel disease are at risk for vaccine-preventable illnesses. Am J Gastroenterol 101: 1834-1840.
- Melmed GY, Ippoliti AF, Papadakis KA, Tran TT, Birt JL, et al. (2006) Patients with inflammatory bowel disease are at risk for vaccine-preventable illnesses. Am J Gastroenterol 101: 1834-1840.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Alizade E (2024) Lymphedema In A Patient With DecompensatedCirrhosis. Arch Sci 8: 216.
Copyright: © 2024 Alizade E. This is an open-access article distributed under theterms of the Creative Commons Attribution License, which permits unrestricteduse, distribution, and reproduction in any medium, provided the original author andsource are credited.
Share This Article
Open Access Journals
Article Usage
- Total views: 179
- [From(publication date): 0-2024 - Jan 26, 2025]
- Breakdown by view type
- HTML page views: 145
- PDF downloads: 34