Short Article Open Access
Lymphatic Vessels in the Human Endometrium: Are they Present or Absent?
Tatsuo Tomita* and Kuni Mah
Departments of Integrative Bioscience and Pathology, Oregon Health and Science University, Portland, USA
- *Corresponding Author:
- Tomita T
Oregon Health and Science University
USA
FAX: 5034948918
Tel: 5036465747
E-mail: tomitat@ohsu.edu
Received date: June 16, 2015 Accepted date: July 20, 2015 Published date: July 23, 2015
Citation:Tomita T, Mah K (2015) Lymphatic Vessels in the Human Endometrium: Are they Present or Absent?. J Clin Exp Pathol 5:241. doi: 10.4172/2161-0681.1000241
Copyright: ©2015 Tomita T, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Clinical & Experimental Pathology
Abstract
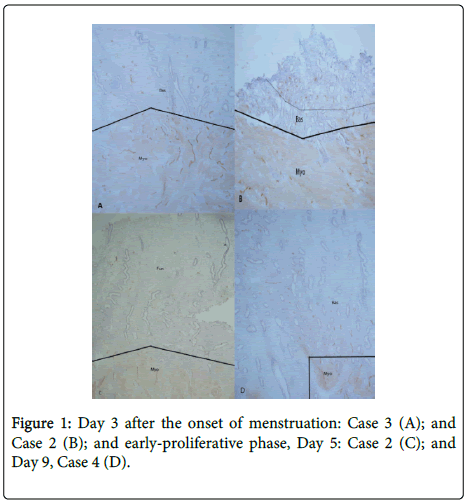
The presence and structure-function relationship of lymphatic vessels in the human endometrium are still sketchy and unsettled: some authors claimed that there were no lymphatic vessels [1,2] but more reports agreed that lymphatic vessels are present in the human endometrium, especially in the basalis but may not be in the functionalis [3-6]. Recently more reliable Immunocytochemical markers for lymphatic vessels became available and have been widely utilized using D2-40 [7] and lymphatic epithelial hyaluronan receptor-1 (LYVE-1) [8]. D2-40 recognizes the collecting lymphatic vessels and LYVE-1 recognizes mainly lymphatic capillaries [9]. With routinely formalin-fixed and paraffin-embedded sections, not all lymphatic sections are immunostained but frozen sections provide consistently much more lymphatic and venous vessels. There are numerous lymphatic vessels in the myometrium and basalis in all menstrual phases. In the Day 3 endometrium from the menstrual period, there were numerous small lymphatic vessels in the remaining basalis by both D2-40 and LYVE-1. There are cyclic changes of lymphatic vessels in the functionalis: The early proliferative phase endometrium, Day 5 showed very few, small lymphatic vessels in the lower functionalis (Figure 1) and Day 9 endometrium revealed few lymphatic vessels in the upper endometrium.
Introduction
The presence and structure-function relationship of lymphatic vessels in the human endometrium are still sketchy and unsettled: some authors claimed that there were no lymphatic vessels [1,2] but more reports agreed that lymphatic vessels are present in the human endometrium, especially in the basalis but may not be in the functionalis [3-6]. Recently more reliable Immunocytochemical markers for lymphatic vessels became available and have been widely utilized using D2-40 [7] and lymphatic epithelial hyaluronan receptor-1 (LYVE-1) [8]. D2-40 recognizes the collecting lymphatic vessels and LYVE-1 recognizes mainly lymphatic capillaries [9]. With routinely formalin-fixed and paraffin-embedded sections, not all lymphatic sections are immunostained but frozen sections provide consistently much more lymphatic and venous vessels. There are numerous lymphatic vessels in the myometrium and basalis in all menstrual phases. In the Day 3 endometrium from the menstrual period, there were numerous small lymphatic vessels in the remaining basalis by both D2-40 and LYVE-1. There are cyclic changes of lymphatic vessels in the functionalis: The early proliferative phase endometrium, Day 5 showed very few, small lymphatic vessels in the lower functionalis (Figure 1) and Day 9 endometrium revealed few lymphatic vessels in the upper endometrium .
There were numerous large lymphatic vessels in the myometrium (Myo) and a mixture of many large and small lymphatic vessels in the basalis (Bas) (A and B). Small fragmented lymphatic vessels were noted in the upper basalis (B). The early-proliferative phase, Day 5 endometrium showed large lymphatic vessels in basalis with few small lymphatic vessels in the upper-endometrium (C). Day 9 endometrium revealed small lymphatic vessels in the lower functionalis (D). Immunostained with D2-40 for lymphatic vessels.
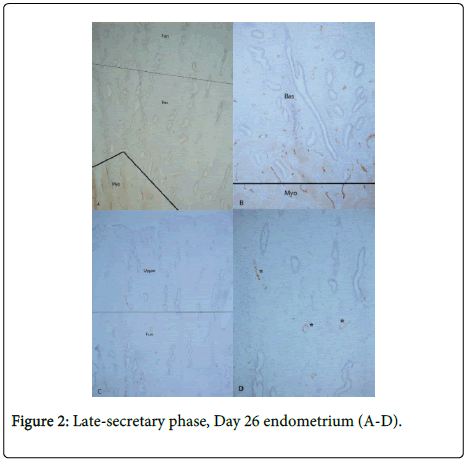
In the late secretary phase, Day 25, there were a few scattered large longitudinal lymphatic vessels in the upper functionalis (Figure not shown). Numerous dilated disrupted lymphatic vessels appeared in the Day 26 functionalis by D2-40 immunostaining. By LYVE-1 immunostaining, more lymphatic vessels were generally immunostained than those by D2-40 immunostaining. The Day 26 endometrium revealed much more longitudinal lymphatic vessels in the upper functionalis concomitant with markedly dilated venous vessels (Figure 2).
There were more increased dilated larger lymphatic vessels in the upper functionalis as compared to smaller lymphatic in the lower functionalis (A and B). There were numerous dilated venous vessels in the upper functionalis than in the lower functionalis (C and D). A and B: Immunostained with LYVE-1 for lymphatic vessels. C and D: Immunostained with von Willebrand factor/factor-8 for venous vessels.
By functional study using mouse models, Rodgers et al reported that a majority of menstrual bleeding commences from arterial and capillary vessels for 70% of blood loss whereas 25% of blood loss follows for venous loss [7]. It is likely that the remaining 5% of menstrual fluid is through burst dilated lymphatic vessels in the functionalis as suggested histologically in this study. Thus, these data from the frozen section immunostaining support consistent presence of lymphatic vessels in the myometrium and basalis and cyclic changes of lymphatic vessels in the functionalis with few to a few lymphatic vessels in the early to mid-proliferative phase functionalis and markedly increased dilated lymphatic vessels in the functionalis from the premenstrual phase [8,9]. Thus, it appears that all arterial, venous and lymphatic vessels undergo menstrual cyclic changes shed for menstruation [8-10].
Acknowledgement
This study was supported in part by ONPRC Core grant NIH 000163.
References
- Red-Horse K, Rivera J, Schanz A, Zhou Y, Winn V, et al. (2006)Cytotrophoblast induction of arterial apoptosis and lymphangiogenesis in an in vitro model of human placentation. J Clin Invest 116:2643-2652.
- Koukourakis MI, Giatromanolaki A, Sivridis E, Simopoulos C, Gatter KC, et al. (2005) LYVE-1 immunohistochemical assessment of lymphangiogenesis in endometrial and lung cancer. J Clin Path 58:202-206.
- Nayak NR, Critchley HO, Slayden OD, Menrad A, Chwalisz K, et al. (2000) Progesterone withdrawal up-regulates vascular endothelial growth factor receptor type 2 in the superficial zone stroma of the human and macaque endometrium: potential relevance to menstruation. J ClinEndocrinolMetab 2000, 85:3443-3452.
- Blackwell P, Fraser I (1981) Superficial lymphatics in the functionalzone of normal human endometrium. Microvasc Res 21:142-152.
- Garling JE, Rogers PA (2012) The endometrial lymphatic vasculature: Function and dysfunction. Rev EndocrMetab Disorder 13:265-275.
- Uchino S, Ichikawa S, Okubo M, Nakamura Y, Iimura A (1987) Methods of detection of lymphatic s and their changes with oesterous cycle. Int Angiology 6:271-278.
- Rogers PA, Donoghue JF, Walter LM, Girling JE (2009) Endometrial angiogenesis, vascular maturation and lymphangiogenesis. ReprodSci 6:201-209.
- Tomita T, Mah K (2014) Cyclic changes of lymphatic vessels in human endometrium. Open J Pathol 4:5-12.
- Tomita T, Mah K Cyclic changes of lymphatic and venous vessels in human endometrium. Open J Pathol 4:194-205.
- Spinella F, Garrafa E, Di Castro V, Rosanò L, Nicotra MR (2009) Endothelin-1 stimulates lymphatic endothelial cells and lymphatic vessels to grow and invade. Cancer Res 2009, 69:2669-2676
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 14254
- [From(publication date):
August-2015 - Jul 04, 2025] - Breakdown by view type
- HTML page views : 9671
- PDF downloads : 4583