Research Article Open Access
Low-intensity Physical Activity is Associated with Lower Maternal Systemic Inflammation during Late Pregnancy
Tinius RA1*, Cahill AG2 and Cade WT1
1Department of Physical Therapy, Washington University School of Medicine, USA
2Department of Obstetrics and Gynecology, Washington University School of Medicine, USA
- Corresponding Author:
- Rachel A Tinius
MSCI, PhD, ACSM-EP-C, School of Kinesiology
Recreation, and Sport Western Kentucky University
1906 College Heights Blvd, #11089
Bowling Green, KY, USA
Tel: 270-745-5026
Fax: 270-745-6043
E-mail: rachel.tinius@wku.edu
Received Date: June 07, 2017; Accepted Date: June 25, 2017; Published Date: June 27, 2017
Citation: Tinius RA, Cahill AG, Cade WT (2017) Low-intensity Physical Activity is Associated with Lower Maternal Systemic Inflammation during Late Pregnancy. J Obes Weight Loss Ther 7:343. doi:10.4172/2165-7904.1000343
Copyright: © 2017 Tinius RA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Obesity & Weight Loss Therapy
Abstract
Excessive maternal inflammation during pregnancy increases the risk for maternal and neonatal metabolic complications. Fortunately, maternal physical activity during pregnancy appears to reduce maternal inflammation. The purpose of this study was to examine the relationship between maternal physical activity intensity and maternal inflammation during late pregnancy. Maternal physical activity levels (sedentary, light, lifestyle, and moderate), fitness levels, and systemic inflammation (plasma C-reactive protein (CRP) concentration) were measured between 32-37 weeks gestation. Relationships were examined by Spearman Rank Coefficient Correlation analyses. Maternal plasma CRP was negatively associated with time spent in light and lifestyle physical activities (Light: r=-0.40, p=0.01; Lifestyle: r=-0.31, p=0.03), but not with time spent in moderate physical activity (r=-0.18, p=0.21). Higher maternal plasma CRP tended to correlate with more time spent sedentary (r=0.27, p=0.06). In addition, increases in light and lifestyle activities may elicit a clinically meaningful change in inflammation. In conclusion, pregnant women should be encouraged to incorporate more low-intensity physical activities into their daily routines in order to decrease systemic inflammation and potentially improve maternal and neonatal pregnancy outcomes.
Keywords
Inflammation; Pregnancy; Physical activity
Introduction
Low-grade chronic inflammation, often secondary to obesity, plays an important role in the pathogenesis of many chronic diseases including metabolic syndrome, cardiovascular disease, diabetes, and hypertension [1-4]. During pregnancy, maternal systemic inflammation is physiologically elevated [5,6]. Excessive inflammation during pregnancy increases the risk for metabolic complications such as insulin resistance/gestational diabetes and hypertension/ preeclampsia [6-8]. Increased inflammation might also increase risk for future maternal disease including metabolic syndrome, insulin resistance, diabetes, hypertension, and cardiovascular disease [9]. Maternal inflammatory changes during pregnancy appear to extend into the placenta potentially exposing the fetus to an inflammatory environment [10], which might contribute to preterm delivery, infection, and the programming of adult metabolic disease [6,11,12].
Light and vigorous maternal physical activities during pregnancy are associated with lower systemic inflammation in the second trimester [13,14]. However, the relationship between physical activity intensity and maternal inflammation in late pregnancy is unclear. The purpose of this study is to examine the relationship between physical activity intensity and inflammation during late pregnancy.
Materials and Methods
Participants were all part of larger ongoing study cohorts [15,16]. Pre-pregnancy body mass index (BMI) was calculated at initiation of prenatal care. All other measures were taken between 32-37 weeks gestation. Body composition was measured using 7-site skinfold anthropometry (Harpenden Skinfolds Caliper, Baty International, United Kingdom) [17]. Fitness levels were assessed using the YMCA submaximal cycle test on a recumbent bicycle (Lode Corvial Recumbant, Lode B.V., The Netherlands). Maternal physical activity levels were assessed for one week one using the ActiGraph GT3X+ accelerometer (ActiGraph LLC, Pensacola, FL) on the non-dominant wrist. ActiGraph data was collected for seven consecutive days at 30 Hertz (compliance was 100% as all 50 women wore the wristband for all seven days). The percentage of time spent sedentary as well as the amount of time spent participating in different categories of physical activity were calculated using algorithms corresponding to the following activity counts: sedentary: 0-99 counts/min, light: 100-759 counts/min, lifestyle: 760-1951 counts/min, moderate: 1952-5724 counts/min [18]. Inflammation was measured via fasting plasma concentration of high-sensitivity C-reactive protein (CRP).
Spearman’s rank order correlation coefficients were used to assess the degree of relationships between CRP and all other variables. Student’s independent t-tests were used to compare time spent in lowintensity activities between those who are at risk for cardiovascular disease (based on an established cut-off value of CRP ≥ 3.0 mg/L, which represents high-risk for cardiovascular disease [19]) and those who are not (CRP<3.0 mg/L). Logistic regression was also used to determine the amount of physical activity necessary to reduce the odds of having a CRP value ≥ 3.0 mg/L.
Results
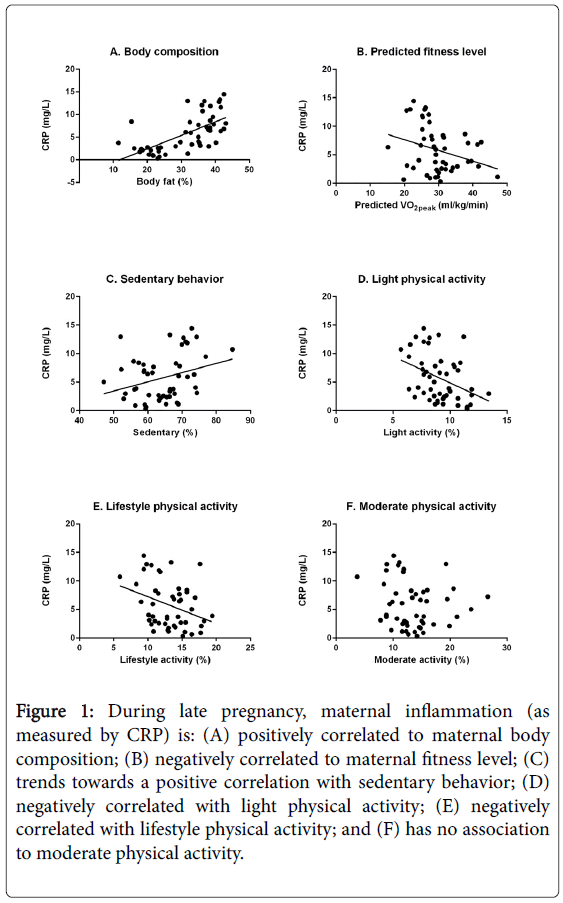
Despite a small sample size, there was an even distribution within the sample among categories of race, parity, and income which might aid in the generalizability of the findings. Maternal plasma CRP concentration was associated with maternal body fat percentage at 32-37 weeks (r=0.70, p<0.001). Higher maternal fitness levels were associated with lower maternal plasma inflammation (r=-0.30, p=0.03). Maternal plasma CRP was negatively associated with time spent in light activity and lifestyle physical activities (light: r=-0.40, p=0.01; lifestyle: r=-0.31, p=0.03). CRP was not correlated with time spent in moderate physical activity (r=-0.18, p=0.21). Higher maternal plasma CRP concentration tended to correlate with more time spent sedentary (r=0.27, p=0.06). Correlations are shown in Figure 1. There were no differences in CRP between the women who only walked and the women who walked in conjunction with other modes of exercise such as biking, swimming, yoga, and weight-lifting (6.2 ± 3.1 mg/L vs. 6.3 ± 1.9 mg/L, p=0.94) (Table 1 and Figure 1).
Figure 1: During late pregnancy, maternal inflammation (as measured by CRP) is: (A) positively correlated to maternal body composition; (B) negatively correlated to maternal fitness level; (C) trends towards a positive correlation with sedentary behavior; (D) negatively correlated with light physical activity; (E) negatively correlated with lifestyle physical activity; and (F) has no association to moderate physical activity.
| Characteristics | mean ± SD |
|---|---|
| Age (year) | 26.6 ± 5.0 |
| Pre-pregnancy BMI (kg/m2) | 30.2 ± 7.5 |
| Body fat percentage (%) | 31.2 ± 8.8 |
| Resting systolic blood pressure (mmHg) | 110.2 ± 9.4 |
| Resting diastolic blood pressure (mmHg) | 70.0 ± 6.8 |
| Resting heart rate (bpm) | 87.4 ± 10.8 |
| Gestational weight gain (kg) | 11.8 ± 7.1 |
| C-Reactive protein (mg/L) | 5.7 ± 4.0 |
| Race | |
| African-American Caucasian Other |
26 (52%) 21 (42%) 3 (6%) |
| Parity | |
| Nulliparous Multiparous |
28 (56%) 22 (44%) |
| Income | |
| Low Moderate-to-high |
23 (46%) 27 (54%) |
| Physical activity levels (%/week) | |
| Sedentary Light Lifestyle Moderate |
64.3 ± 7.5 9.1 ± 1.7 13.1 ± 2.9 13.5 ± 4.3 |
| Predicted VO2max (ml/kg/min) | 29.7 ± 6.4 |
Table 1: Maternal demographic and metabolic characteristics (N=50).
The amount of time spent in low-intensity physical activities (i.e. light or lifestyle) was 24.4 ± 3.8% (351 minutes) for women with a CRP value<3 mg/dl vs. 21.1 ± 4.4% (304 minutes) for women who had a CRP value ≥ 3.0 mg/L (p=0.02). The odds of having CRP ≥ 3.0 mg/L were reduced by 16% for every additional 14 minutes per day of lowintensity physical activity (Exp (B)=0.84, 95% CI [0.72-0.98], p=0.03).
Discussion
The primary finding of our study is that time spent in light and lifestyle physical activities during late pregnancy is associated with lower maternal systemic inflammation. To our knowledge, this is the first study to show relationships between low-intensity maternal physical activity and maternal systemic inflammation during late pregnancy. Understanding the relationships between physical activity intensity and inflammation during late pregnancy (i.e. the present study) is imperative as women are most likely to decrease their physical activity levels and gain additional weight near the end of gestation [20-22]. In addition, our study examined these relationships in a cohort of predominantly obese women, which is important because these women are at the highest risk for excessive maternal inflammation and its downstream sequel [23,24].
Additionally, time spent sedentary during pregnancy tended to be associated with higher maternal systemic inflammation. Surprisingly, there was not a significant relationship between time spent in moderate physical activity and inflammation. These data suggest that low-intensity physical activity may reduce inflammation in pregnant women and that decreasing time spent sedentary and increasing low-intensity activities may be enough of a stimulus to elicit reductions in inflammation. Our findings also suggest that more intense physical activities might not necessarily be superior to walking during late pregnancy in terms of lowering maternal inflammation; however more research in necessary to confirm this.
Upon further analysis, our data suggest that spending an additional 14 minutes per day in light or lifestyle physical activities may reduce the odds of having a CRP value over the clinical threshold of 3.0 mg/L by 16%; however, this should be confirmed in a larger cohort. In addition, pregnant women with CRP values below this clinical threshold spent on average only 47 additional minutes per day doing light and lifestyle activities than those who were above this clinical value. Therefore, even small daily increases in light and lifestyle activities could elicit a clinically meaningful change in inflammation.
Based on the present study, we believe pregnant women should be encouraged to increase physical activity during day-to-day tasks (e.g. taking the stairs, parking further away, walking instead of driving) in order to reduce systemic inflammation late in pregnancy. Not only do these types of lifestyle changes appear to elicit reductions in maternal systemic inflammation, but they are easier for pregnant women to adopt compared to structured exercise programs. In fact, the most commonly reported barriers to physical activity during pregnancy are lack of time, employment obligations, childcare responsibilities, fatigue, and pregnancy-related discomfort [25-29]. Incorporating less sedentary time and more low-intensity physical activities into daily routines might help women overcome these barriers as these modifications do not involve large time commitments (e.g. does not require a blocked-off period of time to go the gym); they can be performed in the workplace (e.g. take the stairs at work, use a standing desk, take frequent breaks at work to walk); they can be done with children (e.g. playing in the yard with other kids or pets, going for a slow walk with a stroller or wagon, walking around a store); and they are not overly fatiguing activities that may be uncomfortable during late pregnancy.
Take-home points
• Maternal inflammation during late pregnancy is negatively correlated with low-intensity physical activities (light, lifestyle) but not moderate intensity activities. Thus, low-intensity activities may help lower systemic inflammation during late pregnancy.
• Spending less total time in sedentary may be enough of a stimulus to reduce inflammation during late pregnancy.
• Even small increases in the duration of time spent in low-intensity physical activities during late pregnancy may elicit clinically meaningful reductions in CRP.
• Pregnant women of all body weights should be encouraged by their health care providers to find low-intensity activities that are enjoyable and can be easily incorporated into their daily lives.
Acknowledgments
The nursing staff at the Washington University Institute for Clinical and Translational Sciences Clinical Research Unit as well as Barnes- Jewish Hospital’s Labor and Delivery floor should be acknowledged for their hard work and altruism. The funding sources: Clinical and Translational Science Award (CTSA) program of the National Center for Advancing Translational Sciences (NCATS) of the National Institutes of Health (NIH) under Award TL1 TR000449 and the Movement Science Program as part of Washington University School of Medicine’s Program in Physical Therapy should also be acknowledged for their contributions.
References
- Yang T, Chu CH, Hsieh PC, Hsu CH, Chou YC, et al. (2013) C-reactive protein concentration as a significant correlate for metabolic syndrome: A Chinese population-based study. Endocrine 43: 351-359.
- Festa A, D'Agostino R, Howard G, Mykkänen L, Tracy RP, et al. (2000) Inflammation and microalbuminuria in nondiabetic and type 2 diabetic subjects: The insulin resistance atherosclerosis study. Kidney Int 58: 1703-1710.
- Ridker PM, Bassuk SS, Toth PP (2003) C-reactive protein and risk of cardiovascular disease: Evidence and clinical application. CurrAtheroscler Rep 5: 341-349.
- Yudkin JS, Stehouwer CD, Emeis JJ, Coppack SW (1999) C-reactive protein in healthy subjects: Associations with obesity, insulin resistance, and endothelial dysfunction: A potential role for cytokines originating from adipose tissue? ArteriosclerThrombVascBiol 19: 972-978.
- Watts DH, Krohn MA, Wener MH, Eschenbach DA (1991) C-reactive protein in normal pregnancy. ObstetGynecol 77: 176-180.
- Schmatz M, Madan J, Marino T, Davis J (2010) Maternal obesity: The interplay between inflammation, mother and fetus. J Perinatol 30: 441-446.
- Ozgu-Erdinc AS, Yilmaz S, Yeral MI, Seckin KD, Erkaya S, et al. (2014) Prediction of gestational diabetes mellitus in the first trimester: Comparison of C-reactive protein, fasting plasma glucose, insulin and insulin sensitivity indices. J Matern Fetal Neonatal Med 2014: 1-6.
- Borzychowski AM, Sargent IL, Redman CW (2006) Inflammation and pre-eclampsia. Semin Fetal Neonatal Med 11: 309-316.
- KöÅÂ?üÅÂ? N, KöÅÂ?üÅÂ? A, Turhan N (2014) Relation between abdominal subcutaneous fat tissue thickness and inflammatory markers during pregnancy. Arch Med Sci 10: 739-745.
- Challier JC, Basu S, Bintein T, Minium J, Hotmire K, et al. (2008) Obesity in pregnancy stimulates macrophage accumulation and inflammation in the placenta. Placenta 29: 274-281.
- Barker DJ (2004) The developmental origins of adult disease. J Am CollNutr 23: 588S-595S.
- Segovia SA, Vickers MH, Gray C, Reynolds CM (2014) Maternal obesity, inflammation, and developmental programming. Biomed Res Int 2014: 418975.
- Wang Y, Cupul-Uicab LA, Rogan WJ, Eggesbo M, Travlos G, et al. (2014) Recreational exercise before and during pregnancy in relation to plasma c-reactive protein concentrations in pregnant Women. J Phys Act Health 12: 770-775.
- Hawkins M, Pekow P, Chasan-Taber L (2014) Physical activity, sedentary behavior, and C-reactive protein in pregnancy. Med Sci Sports Exerc 46: 284-292.
- Tinius RA, Cahill AG, Strand EA, Cade WT (2016) Maternal inflammation during late pregnancy is lower in physically active compared with inactive obese women. ApplPhysiolNutrMetab 41: 191-198.
- Tinius RA, Cahill AG, Strand EA, Cade WT (2015) Altered maternal lipid metabolism is associated with higher inflammation in obese women during late pregnancy. IntegrObes Diabetes 2: 168-175.
- Jackson AS, Pollock ML, Ward A (1980) Generalized equations for predicting body density of women. Med Sci Sports Exerc 12: 175-181.
- Freedson PS, Melanson E, Sirard J (1998) Calibration of the computer science and applications, Inc. accelerometer. Med Sci Sports Exerc 30: 777-781.
- Oda E, Oohara K, Abe A, Veeraveedu PT, Watanabe K, et al. (2006) The optimal cut-off point of C-reactive protein as an optional component of metabolic syndrome in Japan. Circ J 70: 384-388.
- Borodulin KM, Evenson KR, Wen F, Herring AH, Benson AM (2008) Physical activity patterns during pregnancy. Med Sci Sports Exerc 40: 1901-1908.
- Borodulin K, Evenson KR, Herring AH (2009) Physical activity patterns during pregnancy through postpartum. BMC Womens Health 9: 32.
- Walter JR, Perng W, Kleinman KP, Rifas-Shiman SL, Rich-Edwards JW, et al.(2015) Associations of trimester-specific gestational weight gain with maternal adiposity and systolic blood pressure at 3 and 7 years postpartum. Am J ObstetGynecol 212: 499.
- Christian LM, Porter K (2014) Longitudinal changes in serum proinflammatory markers across pregnancy and postpartum: Effects of maternal body mass index. Cytokine 70: 134-140.
- Denison FC, Roberts KA, Barr SM, Norman JE (2010) Obesity, pregnancy, inflammation, and vascular function. Reproduction 140: 373-385.
- Evenson KR, Moos MK, Carrier K, Siega-Riz AM (2009) Perceived barriers to physical activity among pregnant women. Matern Child Health J 13: 364-375.
- Leiferman J, Swibas T, Koiness K, Marshall JA, Dunn AL (2011) My baby, my move: Examination of perceived barriers and motivating factors related to antenatal physical activity. J Midwifery Womens Health 56: 33-40.
- Cramp AG, Bray SR (2009) A prospective examination of exercise and barrier self-efficacy to engage in leisure-time physical activity during pregnancy. Ann Behav Med 37: 325-334.
- Cioffi J, Schmied V, Dahlen H, Mills A, Thornton C, et al. (2010) Physical activity in pregnancy: Women's perceptions, practices and influencing factors. J Midwifery Womens Health 55: 455-461.
- Marshall ES, Bland H, Melton B (2013) Perceived barriers to physical activity among pregnant women living in a rural community. Public Health Nurs 30: 361-369.
Relevant Topics
- Android Obesity
- Anti Obesity Medication
- Bariatric Surgery
- Best Ways to Lose Weight
- Body Mass Index (BMI)
- Child Obesity Statistics
- Comorbidities of Obesity
- Diabetes and Obesity
- Diabetic Diet
- Diet
- Etiology of Obesity
- Exogenous Obesity
- Fat Burning Foods
- Gastric By-pass Surgery
- Genetics of Obesity
- Global Obesity Statistics
- Gynoid Obesity
- Junk Food and Childhood Obesity
- Obesity
- Obesity and Cancer
- Obesity and Nutrition
- Obesity and Sleep Apnea
- Obesity Complications
- Obesity in Pregnancy
- Obesity in United States
- Visceral Obesity
- Weight Loss
- Weight Loss Clinics
- Weight Loss Supplements
- Weight Management Programs
Recommended Journals
Article Tools
Article Usage
- Total views: 3508
- [From(publication date):
June-2017 - Jul 13, 2025] - Breakdown by view type
- HTML page views : 2626
- PDF downloads : 882