Research Article Open Access
Lower Gastrointestinal Bleeding in Saudi Patients: A Retrospective Longitudinal Study
Ibrahim M. Alruzug*, Thamer A. Aldarsouny, Toufic Semaan and Adnan AlMustafa
Consultant Gastroenterologist, King Saud Medical City, Riyadh, Saudi Arabia
- Corresponding Author:
- Ibrahim M. Alruzug, MD
Consultant Gastroenterologist
King Saud Medical City, Riyadh, Saudi Arabia
Tel: 15144515888
E-mail: alruzug@gmail.com
Received Date: March 21, 2016; Accepted Date: March 31, 2016; Published Date: April 05, 2016
Citation: Alruzug IM, Aldarsouny TA, Semaan T, AlMustafa A (2016) Lower Gastrointestinal Bleeding in Saudi Patients: A Retrospective Longitudinal Study. J Gastrointest Dig Syst 6:410. doi:10.4172/2161-069X.1000410
Copyright: © 2016 Alruzug IM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Aims/Objectives: The epidemiology of lower gastrointestinal bleeding (LGIB) in western populations has been well documented but there are scant reports about this condition in Saudi Arabia. This research studied the demographic characteristics of LGIB and assessed the specific colonoscopy findings in Saudi national patients who attended a large population based hospital in Riyadh, the capital city of Saudi Arabia.
Methods: The present study took place at King Saud medical city, Riyadh, Saudi Arabia. A longitudinal retrospective analysis of patient endoscopy records was carried out covering the period from 2004 through to 2015. The patients included were Saudis aged 18 years and above who were receiving first time colonoscopy for an unknown etiology of bleeding.
The patients were from a number of sources: emergency room (ER), inpatients or referred from other centres. Data were entered into Excel and then transferred to SPSS for statistical analysis.
Results: A total of 1,137 patients were included in the study. 178 patients were excluded due to missed or incomplete medical record numbers leaving a total of 959 patients, consisting of 574 (60%) males and 385 (40%) females, with a median age of 51.9 years (SD 18.4, range 18 to 113 years). Most patients were in-patients/ER (346, 42.5%), or out patients (350, 43%), while 137 (14.5%) were referred from other centers. In all colonoscopy findings of LGIB there were significantly more male than female patients, with a male to female ratio of 1.5:1. The most common colonoscopy findings of LGIB were hemorrhoids (369) 38.5%, colitis (78) 8.1%, diverticulosis (116) 12.1%, neoplasm (95) 9.9% and polyps (47) 4.9%, respectively. The colon was normal in (140) 14.6% patients.
Conclusions: Our research showed that hemorrhoids, rectal ulcers, colitis, diverticulosis and tumors were the most common colonoscopy findings of LGIB in a Saudi adult population, with men more predisposed to LGIB than women. These findings are broadly similar to those reported in western populations.
Keywords
Gastrointestinal bleeding; Saudi patients; Retrospective research; Colonoscopy
Introduction
Lower gastrointestinal bleeding (LGIB) is defined as a bleeding source below the ligament of Trietz [1-6]. LGIB usually causes hematochezia, or bright red blood per rectum, but in unusual circumstances hematochezia may result from massive upper GI bleeding with rapid transit times through the gut due to a cathartic effect of the blood. Most acute LGIB stops spontaneously [3], etiologies of LGIB have been reported in many regions over the world [5,7,8], As far as we are aware, there are no available data on the etiology and epidemiology of LGIB in Saudi patients. Hence, our research aimed to identify the demographic characteristics and relevant epidemiological information available in Saudi Arabia in order to guide better the clinical management of patients with LGIB and to compare these findings with patients in other parts of the world.
Methods
The study took place at King Saud Medical City hospital. A longitudinal retrospective analysis of patient records was carried out covering the period 2004 through to 2015. The patients who attended the emergency room (ER) were in-patients or had attended an outpatient clinic or they were referred from other health centres. The study included all Saudi national patients aged 18 years or over who presented with LGIB. Exclusion criteria were non-Saudi patients or patients who had repeated procedures for any reason, whether inpatients or those discharged from hospital and then readmitted, who had a known etiology for LGIB. Poorly prepared patients or with incomplete examination or who had a known ethology for bleeding were also excluded. Data that included patient’s gender, age and endoscopic findings were entered into Excel and then transferred for statistical analysis into SPSS. Data were plotted as appropriate and non-parametric statistics performed where relevant.
Results
A total of 1,137 patients were included in the study. 176 patients were removed from our list due to missing or errors in the Medical Record Number, so a final total of 959 patients were included in the study, consisting of 574 (60%) males and 385 (40%) females (Table 1). There were significantly more males than females in the sample (χ2(1) = 37.2, P < 0.001). The male to female ratio was 1.5:1, with a mean age of 50 years (IQR 38 – 65) and 51.8 (SD 18.4) years, respectively (range 18 to 113 years). The distribution of age was approximately normally distributed except for the censored ages below 18 years.
| Gender | n | % |
|---|---|---|
| Male | 574 | 60 |
| Female | 385 | 40 |
| Patient source | ||
| ER/Inpatient | 346 | 42.5 |
| Outpatient | 350 | 43 |
| Referred from other hospitals | 144 | 14.5 |
| Symptoms | ||
| Hematochezia | 863 | 90 |
| Melena | 96 | 10 |
| Colonoscopy findings | ||
| Haemorrhoids | 369 | 28.5 |
| Diverticulitis/Diverticulosis | 116 | 12.1 |
| Mass/Tumour | 95 | 9.9 |
| Colitis | 78 | 8.1 |
| Rectal Ulcer | 79 | 8.2 |
| Polyps | 47 | 4.9 |
| Angiodysplasia | 32 | 3.3 |
| Other | 3 | 0.3 |
| Normal colonoscopy | 140 | 14.6 |
| Total | 959 | 100 |
Table 1: Demographic characteristics of Saudi patients with LGIB.
There was no evidence of a difference in mean age for males (51.5 years) and females (52.3 years) suffering from LGIB, t(876) = 0.61, P = 0.545. It is clear that the number of cases strongly depends on age since the number of cases in each 5-year age group departed from what would be expected from the age profile of the Saudi population (χ2(17) = 3,532, P < 0.001) Table 2.
| Colonoscopy findings | Mean | Median | M:F ratio | n |
|---|---|---|---|---|
| Hemorrhoids | 48 | 47 | 1.7 | 369 |
| Colitis + related | 48.8 | 46 | 0.9 | 78 |
| Rectal ulcers | 55.8 | 60 | 1.5 | 79 |
| Others (Dieulafoy's lesion + rectal varices) | 58.7 | 60 | 2 | 3 |
| Diverticulum/Diverticulosis | 65.2 | 66 | 1.5 | 116 |
| Polyps | 50.9 | 47 | 1.6 | 47 |
| Mass/Tumor | 58.2 | 58 | 1.3 | 95 |
| Telangiectasia/Angiodysplasia | 53.2 | 54.5 | 1.7 | 32 |
| Normal LGIE | 45.5 | 44 | 1.5 | 140 |
| Total | 51.8 | 50 | 1.5 | 959 |
Table 2: Colonoscopy findings by age and gender.
Most patients were in-patients/ER (346, 42.5%), or out patients (350, 43%), while 137 (14.5%) were referred from other centres. The majority of patients presented with hematochezia (90%) or melena (10%).
Hemorrhoids in 369 (38.5%) patients, diverticulosis in 108 (12.3%), mass or tumor in 88 (10%) confirmed by histopathology to be malignant, rectal ulcer in 79 (8.2%), colitis including inflammatory bowel disease, ischemic colitis, drug-induced or infectious colitis in 78 (8.1%), were the most common colonoscopy findings of LGIB in our centre. Other findings were polyps in 40 patients (4.6%) including benign or malignant polyps (post polypectomy bleeding was added in this category), angiodysplasia in 28 (3.2%) and other causes in 3 patients (0.3%), including Dieulafoy’s lesion and rectal varices. Normal colonoscopy findings were observed in 140 patients (14.6%).
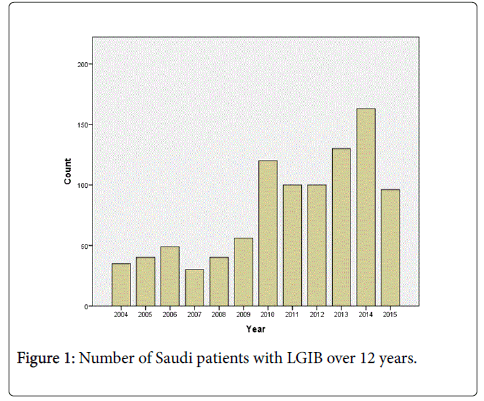
The colonoscopy findings according to age and gender are listed in Table 2. It was noted there was a male predominance in all colonoscopy findings of LGIB except for colitis. The male predominance was expected given that overall there were more male than female LGIB patients. There is a significant rise in cases of lower gastrointestinal bleeding over the years (Figure 1).
Discussion
This large single-centre population-based retrospective study examined demographic features of LGIB in Saudi patients who presented to the General Hospital of King Saud Medical City, Riyadh from January 2004 to December 2015.
This paper has focused on acute LGIB necessitating hospitalisation, medical intervention and support, and those patients with minimal per rectal bleeding, who are often managed as outpatients.
Approximately 900-1,000 colonoscopies are carried out annually in our centre, with about 11% because of LGIB.
Our patients come from ER/inpatient (44.5%) departments, are outpatients (40.5%) or are transferred from other centres (15%). The high numbers of patients with LGIB who came through out patients’ clinics were mainly suffering from haemorrhoids and were routinely referred for colonoscopy to exclude other aetiologies.
The LGIB observed in Saudi patients confirmed previous reports that it increases with age [6,7], and was more common in male than female patients [9,10]. Our study showed predominantly a higher percentage of males (as expected as there were more males than females in patients suffering from LGIB) and male to female ratio1.5:1 in nearly all colonoscopy findings, with a median age of 50 years for both sexes., Males often suffer from chronic constipation due to low fibre diet, low intake of liquids especially water and fruit juices and ignorance of fresh vegetable usage, intake of tobacco and other abuses affect the formation and synthesis of gastric juices and enzymes and retain faecal wastages in the colon and so enhancing bleeding from the large intestines.
The causes of LGIB vary from one region of the world to another. In Western Europe and the United States, diverticulosis is the most common causes of LGIB [11-15].
The most common colonoscopy findings of LGIB in our research were hemorrhoids (38.5%), diverticulosis (12.1%), and neoplasm confirmed by pathology (9.9%), rectal ulcer (8.2%), irritable bowel disease (IBD) and other types of colitis (8.1%). Other less common findings were polyps and post-polypectomy bleeding (4.9%), angiodysplasia (3.3%) and others including Dieulafoy’s lesion (0.2%) and rectal varies (0.1%). Normal colonoscopy was observed in approximately 14.6% of patients.
In contrast to patients from western countries [9], hemorrhoids is the most common colonoscopy findings of LGIB in Saudi patients (38.5%) which is similar to data from other neighbour countries, and some regions in African [8]. This finding might be in part due to obesity, which represents 35% of the population as per the national registry of 2007, frequent or chronic constipation, a low fiber diet and pregnancy. However, the association between these diseases remains ambiguous.
Hemorrhoids cause intermittent low-volume bleeding, with bright red blood seen on the toilet tissue or around, but not mixed, in the stool. Careful examination of the anorectal area with anascopy is essential for diagnosis [16]. In a prospective study, Murshid [17-20] described bleeding as the main presenting symptom of hemorrhoids in Saudi patients who were seen for the first time. Though hemorrhoids can cause chronic mild per rectal bleeding, it is frequently difficult to confirm active bleeding from hemorrhoids in all patients; hence it remains a probable and not definitive source of bleeding, as the majority of people have hemorrhoids that do not bleed [12].
Contrary to the western population, in which diverticular bleeding is the most common etiology of bleeding (34%), it was less common in our research (12.1%) although it ranked as the second commonest finding for LGIB.
Colorectal neoplasm constituted approximately10% of findings in patients with LGIB. More than 90% of these tumours were located in the left colon and confirmed by pathology to be malignant. The reported frequency of acute LGIB resulting from colonic neoplasms ranges from 2% to 26% [3,13]. Though it may be present with other symptoms, lack of bleeding may delay diagnosis in these patients; hence screening programs for colorectal cancers would be worthwhile. Rectal ulcers (including solitary, idiopathic and acute hemorrhagic types) were seen in 8.2% of patients. Rectal ulcers were among the common causes of severe hematochezia in the UCLA CURE study [14]. Rectal ulcers may be the result of fecal impaction, rectal trauma, or rectal prolapse [6].
Among other findings, IBD (confirmed by pathology, ulcerative colitis 3.3% and Crohn’s disease 0.8%, and colitis 1.7% of LGIB patients. Although gastrointestinal bleeding is a common manifestation of inflammatory bowel disease, acute severe hematochezia is infrequent. Most patients with ulcerative colitis report clinically apparent bleeding, in contrast to patients with Crohn’s disease, of who only one third report bleeding. Acute severe hematochezia accounts for up to 6% of hospitalizations for patients with Crohn’s disease and 1.4% to 4.2% of patients with ulcerative colitis [3]. Colitis may be caused by ischemia, be drug-induced, infection and/or IBD. However, the pathology did not confirm the etiology at the first time of biopsy for these patients. Rare findings include Dieulafoy’s lesion (0.2%) and rectal varices (0.1%).
Although there is a significant rise in cases over the years, this increase should be interpreted with caution since there was dropout of data in earlier years (2004–2006) due to poor record keeping. In addition, the city’s population increased from 4.09 million in 2004 to 5.90 million in 2013, which might be expected to impact on the total number of patients seen with LGIB. There were also increased referrals from other health centres in 2013 and 2014.
Limitations
Colonoscopy reports were the major source of data in this retrospective research and so other relevant clinical information beyond the endoscopy report was limited, such as drug history, associated comorbid diseases, severity of bleeding or outcome, and whether some of the reported endoscopic findings definitely establish the exact bleeding site.
In spite of these limitations, there are strengths in our research in that it took place in a large population based centre of Saudi Arabia and was limited to Saudi citizens as well as providing a data base from which to draw future strategic plans and research. It also determines identifies the demographic characteristics and relevant epidemiological information available in Saudi Arabia in order to supervise more appropriate prescription and hospitalization of patients with LGIB and to analyse these clinical features with patients in other region of the worldwide.
Conclusions
Most Saudi patients who presented to our medical center were male, middle aged and were more likely to have hemorrhoids, diverticulosis, tumors, colitis or rectal ulcers that could explain LGIB.
Further prospective research is needed to identify the etiology and outcomes of LGIB in Saudi patients.
References
- Hreinsson JP (2013) Lower gastrointestinal bleeding: incidence, etiology, and outcomes in a population-based setting. European Journal of Gastroenterology &Hepatology 25: 37-43.
- Vernava AM, Moore BA, Longo WE, Johnson FE (1997) Lower gastrointestinal bleeding.Dis Colon Rectum 40: 846-858.
- Bounds BC (2003) Lower gastrointestinal bleeding. Gastroenterology Clinics North America 32: 1107-1125.
- Gayer C, Chino A, Lucas C, Tokioka S, Yamasaki T, et al. (2009). Acute gastrointestinal bleeding in 1,112 patients admitted to an urban emergency medical centre. Surgery 146: 600-606.
- Zuccaro G (2008) Epidemiology of lower gastrointestinal bleeding.Best Pract Res ClinGastroenterol 22: 225-232.
- Strate LL (2005) Lower GI bleeding: epidemiology and diagnosis.GastroenterolClin North Am 34: 643-664.
- Farrell JJ, Friedman LS (2000) Gastrointestinal bleeding in older people.GastroenterolClin North Am 29: 1-36, v.
- Ajayi AOA (2014) Lower Gastrointestinal Bleeding: Spectrum of colonoscopy findings in Ado-Ekiti, Nigeria. International Journal of Medical Science 6: 128-133.
- Chaudhry V, Hyser MJ, Gracias VH, Gau FC (1998) Colonoscopy: the initial test for acute lower gastrointestinal bleeding.Am Surg 64: 723-728.
- Potter GD, Sellin JH (1988) Lower gastrointestinal bleeding.GastroenterolClin North Am 17: 341-356.
- Bono MJ (1996) Lower gastrointestinal tract bleeding.Emerg Med Clin North Am 14: 547-556.
- Gralnek IM (2013) The role of colonoscopy in evaluating hematochezia: a population based study in a large consortium of endoscopy practices. Gastrointestinal Endoscopy 77: 410-418.
- Fernández E, Linares A, Alonso JL, Sotorrio NG, de la Vega J, et al. (1996) Colonoscopic findings in patients with lower gastrointestinal bleeding send to a hospital for their study. Value of clinical data in predicting normal or pathological findings.Rev EspEnferm Dig 88: 16-25.
- Machicado GA, Jensen DM (2006) Endoscopic diagnosis and treatment of severe lower gastrointestinal bleeding.Indian J Gastroenterol 25 Suppl 1: S43-51.
- Bramley PN, Masson JW, McKnight G, Herd K, Fraser A, et al. (1996) The role of an open-access bleeding unit in the management of colonic haemorrhage. A 2-year prospective study.Scand J Gastroenterol 31: 764-769.
- Rockey DC (2006) Lower gastrointestinal bleeding.Gastroenterology 130: 165-171.
- Murshid KR (1997) Hemorrhoids! Don't call the surgeon yet.Saudi J Gastroenterol 3: 94-95.
- Shennak MM, Tarawneh MM (1997) Pattern of colonic disease in lower gastrointestinal bleeding in Jordanian patients: a prospective colonoscopic study.Dis Colon Rectum 40: 208-214.
- Ohyama T, Sakurai Y, Ito M, Daito K, Sezai S, et al. (2000) Analysis of urgent colonoscopy for lower gastrointestinal tract bleeding.Digestion 61: 189-192.
- Bai Y, Peng J, Gao J, Zou DW, Li ZS (2011) Epidemiology of lower gastrointestinal bleeding in China: single-center series and systematic analysis of Chinese literature with 53,951 patients.J Gastroenterol Hepatol 26: 678-682.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 11234
- [From(publication date):
April-2016 - Apr 04, 2025] - Breakdown by view type
- HTML page views : 10317
- PDF downloads : 917