Case Report Open Access
Long-Term Recurrent Liposarcoma of the Mediastinum with Gastric Metastasis: A Case Report
Yung-Sung Yeh1,2,3, Yu-Ho Huang4, Hui-Chen Lin5, Ying-Ling Shih6, Chien-Yu Lu7,8 and Jaw-Yuan Wang3,9,10,11*
1Division of Trauma, Department of Surgery, Kaohsiung Medical University Hospital, Kaohsiung Medical University, Kaohsiung 807, Taiwan
2Department of Emergency Medicine, Kaohsiung Medical University Hospital, Kaohsiung Medical University, Kaohsiung 807, Taiwan
3Graduate Institute of Clinical Medicine, College of Medicine, Kaohsiung Medical University, Kaohsiung, Taiwan
4Department of Anatomy, Faculty of Medicine, College of Medicine, Kaohsiung Medical University, Taiwan
5Department of Pathology, Kaohsiung Medical University Hospital, Kaohsiung Medical University, Kaohsiung, Taiwan
6Department of Nursing, Kaohsiung Medical University Hospital, Kaohsiung Medical University, Kaohsiung, Taiwan
7Department of Internal Medicine, Faculty of Medicine, College of Medicine, Kaohsiung Medical University, Kaohsiung, Taiwan
8Division of Gastroenterology, Department of Internal Medicine, Kaohsiung Medical University Hospital, Kaohsiung Medical University, Kaohsiung, Taiwan
9Division of Gastrointestinal and General Surgery, Department of Surgery, Kaohsiung Medical University Hospital, Kaohsiung, Taiwan
10Department of Surgery, Faculty of Medicine, College of Medicine, Kaohsiung Medical University, Kaohsiung, Taiwan
11Center for Biomarkers and Biotech Drugs, Kaohsiung Medical University, Kaohsiung, Taiwan
- Corresponding Author:
- Jaw-Yuan Wang
Division of Gastrointestinal and General Surgery
Department of Surgery
Kaohsiung Medical University Hospital
Kaohsiung Medical University
No. 100 Tzyou 1st Road
San-Ming District, Kaohsiung 807, Taiwan
Tel: +886-7-3122805
Fax: +886-7-3114679
E-mail: cy614112@ms14.hinet.net
Received Date: September 24, 2015 Accepted Date: October 12, 2015 Published Date: October 18, 2015
Citation: Yeh YS, Huang YH, Lin HC, Shih YL, Lu CY, et al. (2015) Long-Term Recurrent Liposarcoma of the Mediastinum with Gastric Metastasis: A Case Report. J Gastrointest Dig Syst S13:005. doi:10.4172/2161-069X.1000S13-005
Copyright: © 2015 Yeh YS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
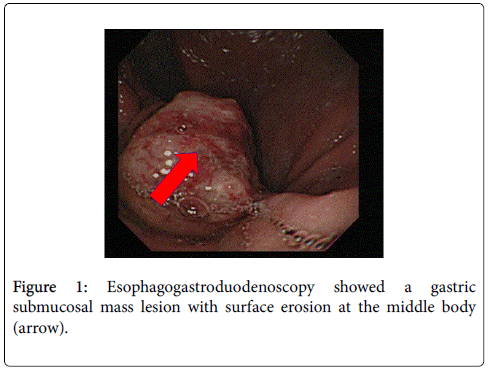
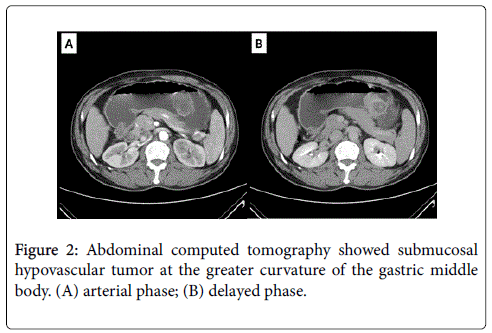
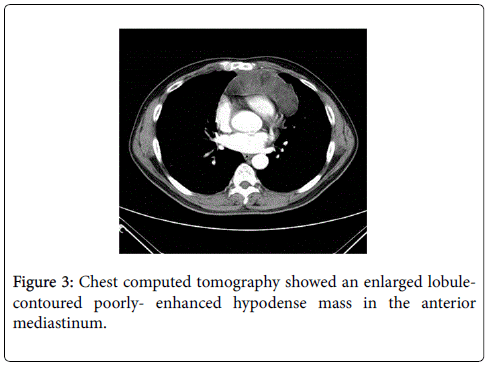
Liposarcoma is a soft tissue sarcoma typically seen in adults, and it usually arises in the limbs or retroperitoneum but rarely has a visceral location. We report here a rare case of long-term recurrent liposarcoma of the anterior mediastinum with gastric metastasis. A 55-year-old male was admitted to hospital with initial presentations of epigastralgia, anorexia, body weight loss and black stool recently. Nine years before this episode, he had received wide excision of a well-differentiated liposarcoma in the anterior mediastinum. After admission, esophagogastroduodenoscopy revealed a submucosal mass with mucosal erosion involving the great curvature of the stomach. A partial gastrectomy was performed and histopathological examination confirmed that the gastric submucosal lesion was a metastasis of the liposarcoma from mediastinum. The patient was finally diagnosed with recurrent mediastinal liposarcoma with gastric metastasis. A review of the medical literature in English till now shows that this is the first reported case of recurrent mediastinal liposarcoma with gastric metastasis.
Keywords
Mediastinum; Liposarcoma; Gastric metastasis
Introduction
Liposarcoma, the most common soft-tissue sarcoma, comprises 15-20% of all patients with sarcoma. It most commonly occurs in the limbs, retroperitoneum and trunk but rarely involves the viscera [1,2]. With recent advances in the molecular genetic characterization of soft tissue tumors, Enzinger and Winslow categorized soft-tissue liposarcoma into three main histogenetic subtypes, including welldifferentiated/ dedifferentiated liposarcoma, myxoid liposarcoma, pleomorphic and mixed-type [3].
Primary mediastinal liposarcoma constitutes <1% of all malignancies and also <1% of primary sarcomas of the mediastinum [1]. Well-differentiated cell type, also known as “atypical lipomatous tumor” is the most common subtype of liposarcoma and is most common in adults. The location of the liposarcoma is the most important prognostic factor in well-differentiated liposarcoma because of the strong correlation between surgical resectability and recurrence rate [1].
Well-differentiated liposarcoma cannot metastasize unless it undergoes dedifferentiation. Dedifferentiation refers to changes in liposarcoma cells that result in higher grades and non-lipogenic status. The most common sites of liposarcoma metastasis are the lungs, liver, soft tissue, bone, and brain [4]. We herein report an unusual case of a recurrent mediastinal liposarcoma with distant metastasis to the stomach.
Case Report
A 55-year-old male was admitted to our hospital with first presentation of tarry stool, epigastralgia, anorexia, and loss of body weight in recent days. Tracing back his past medical history, he had undergone wide excision of a well-differentiated liposarcoma in the anterior mediastinum nine years previously. On admission, physical examination revealed an acutely ill patient with mild epigastralgic tenderness. Laboratory data showed mild leukocytosis, mild anemia (hemoglobin: 12.8 g/dl) and tumor marker levels were within normal limit. Under the suspicion of upper gastrointestinal tract bleeding, esophagogastroduodenoscopic examination revealed a gastric submucosal mass lesion with surface erosion at the middle body over greater curvature (Figure 1). Abdominal computed tomography (CT) scan showed an intramural polypoid mass with a small ulceration at the greater curvature of the gastric middle body, characterized by heterogeneous fatty density (Figure 2). Meanwhile, chest CT scan revealed an enlarged poorly-enhanced hypodense mass with a lobular contour in the anterior mediastinum (Figure 3).
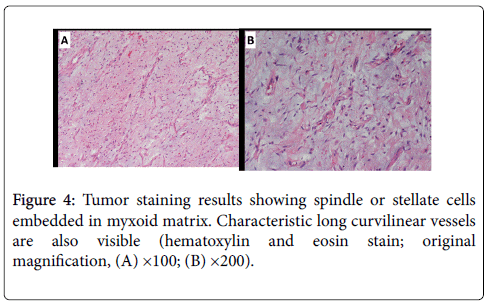
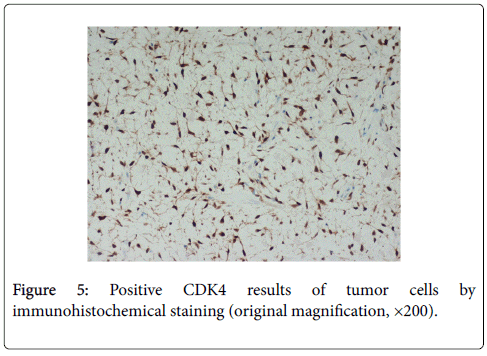
During laparotomy, a partial gastrectomy was performed to prevent tumor bleeding with achieving negative margin. An excised submucosal tumor sample (1.8 × 1.7 × 0.6 cm) appeared yellow-white intersecting the tumor tissue and was elastic in gross inspection. Histopathological findings showed a recurrent well-differentiated liposarcoma with mature adipocytic proliferation (Figure 4). There were myxoid nodules with increased cellularity but occasional mitotic count in a prominent myxoid background presenting a low grade myxofibrosarcoma-like dedifferentiated appearance. The surgical resection line was tumor-free. Immunohistochemical study showed positive for S-100 protein and these cells were distributed in the vicinity of mature fat cells. The mature fat cells and lipoblasts were positive for CDK4 staining (Figure 5) and negative for CD117, CD34, SMA, and DOG-1staining.
Discussion
Primary mediastinal liposarcomas are rare, especially with distant metastasis to the stomach. There are three histological subtypes of liposarcoma: well-differentiated/dedifferentiated liposarcoma, myxoid liposarcoma, pleomorphic and mixed-type. Liposarcomas commonly arise in the extremities and retroperitoneum, but less than 5% of liposarcomas arise in the mediastinum [5].
Mediastinal location is very unusual for this disease entity, and the occurrence in the anterior and posterior mediastinum has relatively equal frequency. The age range of these patients is reported as being between 20 and 70 years with a peak in the 5th decade [6].
The anatomical location of the well-differentiated liposarcoma is the major prognostic factor. Recurrence is common in liposarcomas situated in deep anatomic sites such as the retroperitoneum and the mediastinum, where a sufficiently wide surgical excision margin is often impossible [7]. Although recurrence usually occurs within 6 months after the initial excision, cases of recurrence 5 or even 10 years later have been reported [5]. The patient we report here had a previous history of a huge tumor in the anterior mediastinum 9 years previously; after reviewing the medical history, recurrent mediastinal liposarcoma was highly suspected.
The term dedifferentiation refers to lesions that first appear as lowgrade lesions before progressing to high-grade tumors with evidence of non-lipogenic differentiation. Dedifferentiation, which is most likely a time-dependent phenomenon, occurs in 10% of well-differentiated liposarcomas, typically within 7 to 11 years after the initial diagnosis. The risk of dedifferentiation is highest in mediastinal and retroperitoneal tumors.
Although their histology is highly variable, dedifferentiated areas often resemble unclassified malignant fibrous histiocytoma (MFH)- like pleomorphic sarcomas or intermediate-to-high grade myxofibrosarcomas. The diagnosis of dedifferentiation in the patient reported here was based on pathologic findings showing myxoid nodules in a prominent myxoid background and imparting a lowgrade myxofibrosarcoma-like dedifferentiated appearance. Welldifferentiated liposarcoma has no potential to metastasis unless it undergoes dedifferentiation. Once dedifferentiation occurs, accelerated deterioration of the clinical course is inevitable [8,9], such as in our case.
The most common site of distant metastasis in liposarcoma is the lung, which is consistent with hematogenous dissemination of a tumor, but development of extrapulmonary metastasis of liposarcoma is common. A retrospective review of 60 liposarcoma patients by Cheng et al. showed that 22 patients had developed metastasis [10]; 59% of the initial site of metastasis was an isolated extrapulmonary metastasis. Unlike extrapulmonary metastatic liposarcoma, metastatic liposarcoma of the stomach has not yet been reported. A PubMed search of the English medical literature since 1950 shows no case reports for queries combining “metastasis”, “liposarcoma”, and “stomach neoplasms” as search terms [10].
For the current patient, our histopathological diagnosis was recurrent well-differentiated liposarcoma in the anterior mediastinum and a metastatic stomach liposarcoma. Surgical treatment with or without intraoperative radiation therapy for resectable sarcoma is recommended [11].
Surgical margins should be defined by the pathologist. A reresection with a positive surgical margin is strongly recommended if function is not significantly affected. Adjuvant radiation therapy may be considered for a close margin from normal tissue or microscopically positive margin on nerves, major vessels or bones. Postoperative external bean radiotherapy or brachytherapy improved local control, but do not benefit overall survival. Chemotherapy has an established role in the palliative management of metastatic liposarcoma.
The response of liposarcoma to chemotherapy differs according to histological subtype and grade, which found a significant higher response rate in myxoid liposarcoma compared to all other liposarcomas. In contrast to conventional cytotoxic chemotherapies, which are non-specific, the majority of these novel therapies are based on the understanding of disease biology inherent to a given sarcoma histology, in many cases targeting a specific, aberrant genetic, or molecular pathway. For the majority of novel therapies, treatment efficacy is heavily dependent on subtype [12].
Patients who undergo complete (macroscopic) or even compartmental resection of the primary tumor have an improved prognosis with a 5-year overall survival of 54– 70% (2, 15), yet 41–50% of these patients will demonstrate locally recurrent disease within 5 years after surgery [13].
In this case, surgical margins were at least 1 cm from the tumor and histopathological findings showed a recurrent well-differentiated liposarcoma. Because well-differentiated liposarcoma and dedifferentiated liposarcoma respond poorly to systemic chemotherapy, it is essential that novel molecular targets will be identified to provide new possibilities for therapies.
If no microscopic evidence of residual disease is observed, follow-up including physical exams with imaging (abdominal and pelvic CT scans) should be performed every 3-6 months for the initial 2-3 years and then annually.
In conclusion, recurrent mediastinal liposarcoma with gastric metastasis is very rare; attention should be paid to liposarcoma patients with upper gastrointestinal tract bleeding.
Acknowledgements
This work was supported by an Excellence for Cancer Research Center Grant through funding and the Ministry of Health and Welfare (MOHW104-TDU-B-212-124-003), Taiwan, Republic of China.
References
- Boland JM, Colby TV, Folpe AL (2012) Liposarcomas of the mediastinum and thorax: a clinicopathologic and molecular cytogenetic study of 24 cases, emphasizing unusual and diverse histologic features. Am J SurgPathol 36: 1395-1403.
- Tepetes K, Christodoulidis G, Spyridakis ME, Nakou M, Koukoulis G, et al. (2007) Liposarcoma of the stomach: a rare case report. World J Gastroenterol 13: 4154-4155.
- Weiss SW (2008) Enzinger and Weiss’s Soft Tissue Tumors. Philadelphia, PA: Mosby/E;servier.
- Huang HY, Brennan MF, Singer S, Antonescu CR (2005) Distant metastasis in retroperitoneal dedifferentiated liposarcoma is rare and rapidly fatal: a clinicopathological study with emphasis on the low-grade myxofibrosarcoma-like pattern as an early sign of dedifferentiation. Mod Pathol 18: 976-984.
- Coulibaly B, Bouvier C, Payan MJ, Thomas P (2009) Recurrent dedifferentiated liposarcoma of mediastinum involving lung and pleura. Interact CardiovascThoracSurg 9: 741-742.
- Fukai R, Fukumura Y, Suzuki K (2009) A dedifferentiated liposarcoma of the anterior mediastinum. Int J ClinOncol 14: 174-177.
- Macchiarini P, Ostertag H (2004) Uncommon primary mediastinaltumours. Lancet Oncol 5: 107-118.
- Dei Tos AP (2000) Liposarcoma: new entities and evolving concepts. Ann DiagnPathol 4: 252-266.
- McCormick D, Mentzel T, Beham A, Fletcher CD (1994) Dedifferentiated liposarcoma. Clinicopathologic analysis of 32 cases suggesting a better prognostic subgroup among pleomorphic sarcomas. Am J SurgPathol 18: 1213-1223.
- Cheng EY, Springfield DS, Mankin HJ (1995) Frequent Incidence of Extrapulmonary Sites of Initial Metastasis in Patients with Liposarcoma. Cancer 75: 1120-1127.
- (2012) National Comprehensive Cancer Network. Clinical Practice Guidelines in Oncology.
- Matthyssens LE, Creytens D, Ceelen WP (2015) Retroperitoneal liposarcoma: current insights in diagnosis and treatment. Front Surg 2: 4.
- Liles JS, Tzeng CW, Short JJ, Kulesza P, Heslin MJ (2009) Retroperitoneal and intra-abdominal sarcoma. CurrProblSurg 46: 445-503.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 14496
- [From(publication date):
specialissue-2015 - Apr 05, 2025] - Breakdown by view type
- HTML page views : 9924
- PDF downloads : 4572