Long Term Follow up in Children with Anxiety Disorders Treated with Acceptance and Commitment Therapy or Cognitive Behavioral Therapy: Outcomes and Predictors
Received: 20-Sep-2016 / Accepted Date: 25-Oct-2016 / Published Date: 05-Nov-2016 DOI: 10.4172/2375-4494.1000317
Abstract
Objective: Anxiety disorders in children are the most prevalent of mental health conditions, but also the most treatable. However, a significant number do not benefit from treatment and these places them at risk for future psychiatric disturbance. Whilst Acceptance and Commitment Therapy (ACT) is gaining rapid evidence for its utility in treating a variety of disorders, research in children and adolescence is at an early stage. This paper reports on 2 year follow-up (2YFU) outcomes of the first randomized controlled trial of ACT and traditional cognitive behavioral therapy (CBT) in children with a DSM-IV diagnosis of anxiety disorders. Method: Of the 111 children from urban Sydney, Australia who completed treatment (10-week group-based program of ACT or CBT). A total of 79 (40 ACT and 39 CBT) were assessed at 2YFU. Pre-treatment, posttreatment, 3 months (3MFU) and 2YFU assessments included clinician/self/parent-reported measures of anxiety, anxiety-related quality of life (QOL) and acceptance/defusion outcomes. Several baseline predictors of anxiety outcome were also examined. Results: Positive findings were obtained for both ACT and CBT in terms of long-term maintenance of gains. Across measures, highly significant improvements observed at post and 3MFU were maintained at 2YFU. At post approximately one-third of participants in both treatment groups no longer met criteria for any anxiety disorder, with further improvement evident at 3MFU. Continued improvement was observed at 2YFU, with 45% of ACT and 60% of CBT participants diagnosis free (non-significant difference). Both completer and intention to treat analyses found ACT and CBT to produce similar outcomes. The only significant predictors in the short-term were pre-treatment severity and age. At 2YFU, no significant predictors were identified. However, most participants were in the severe anxiety category pre-treatment, limiting the exploration of severity as a predictor. Conclusion: Both ACT and CBT have shown similar long terms benefits for children with anxiety disorders. There was no clear or strong pattern of baseline predictors of outcomes. Further research is needed to explore this area.
Keywords: Acceptance and commitment therapy, Cognitive behavior therapy, Anxiety disorders, Children, Young people, Randomized controlled trial
218263Introduction
Childhood anxiety disorders are among the most common mental health conditions affecting youth, and they are predictive of long-term adulthood psychiatric problems [1]. Increasing acknowledgement of the significant impact of anxiety disorders on public health has seen greater focus on treatment approaches and empirical evaluation of their effectiveness.
A review of treatments for anxiety disorders in children concluded that evidence-based psychological treatments (cognitive behavior therapy; CBT) and selective serotonin reuptake inhibitor medications (SSRIs) are effective in decreasing anxiety symptoms and functional impairment [2]. Each treatment on its own is effective for young people with anxiety disorders, but a combination of SSRIs and CBT has been found to be more effective than mono-therapies, with this difference decreasing over time [3]. However, pharmacological treatment is not recommended as a first line as there is a potential risk of harm to children and young people [2].
Acceptance and Commitment Therapy (ACT) is considered to be part of the “third wave” of behavioral and cognitive therapies, incorporating elements of CBT with processes of mindfulness and acceptance [4]. Traditional CBT has demonstrated medium to large effect sizes in RCTs and has the most amount of evidence in the treatment of anxiety disorders [5]. Swain, et al. [6] systematic review of ACT for adults with anxiety disorders found ACT to be effective. The literature suggests a potential of ACT for children and young people, but to date there are only three studies all with low external validity [7-9]. However, a review of 21 studies utilizing ACT for a range of presenting problems demonstrated that ACT has some evidence for its effectiveness in the treatment of children [10]. There is a growing amount of research on the effectiveness of ACT versus CBT in the treatment of anxiety. Ruiz [11] found ACT outperformed CBT in 68% of included studies in a systematic review and meta-analysis, with ACT superior in all but one anxiety-specific study. Two randomized clinical trials of over 100 adults with anxiety found both ACT and CBT to be highly effective over time, with similar outcomes [12,13]. Hancock, et al. [14] reported similar results in children and adolescents up to 3 months post-treatment.
Research is scant examining the long term impact of CBT treatments among children with anxiety. Several studies have shown maintenance of gains one year post treatment [15-17]; and including youth 2-3 years [3], 3.5 years [18], 6 years [19] and 7.4 years [20] following treatment cessation. Assessing outcomes over the long term may be particularly indicated among children treated with ACT as studies of ACT for children with a spectrum of presenting problems have found that treatment gains were either not fully evident at posttreatment (or initial follow-up), or that greater improvements for ACT were obtained some months after therapy cessation [21-23]. This underscores the need for the inclusion of longer follow-up time points in research.
Currently there are limited data that clinicians can use to guide treatment decisions regarding which children might benefit most and which might benefit least from currently available empirically supported treatments. The Child/Adolescent Multimodal Study [3,24,25] reviewed psychosocial and medication studies for all DSM– IV pediatric anxiety disorders (ages 6-18 years) published between 1980 and 2010 that included either predictor analyses (factors influencing the likelihood of an outcome during treatment) or moderator analyses (presence or size that at baseline influences the relative likelihood of a particular outcome occurring with one versus another treatment). The review identified 98 RCTs (53 psychosocial; 45 medication trials). Although findings from the predictor analyses were mixed, higher baseline symptom severity and poorer family functioning were consistent predictors of poorer outcome. Moderator analyses findings were also inconsistent across studies, with some showing an effect of gender, type of anxiety disorder, severity of principal anxiety disorder, and comorbidities, but others not. Small sample sizes have been the norm, and findings, when present, often do not remain consistent across measures or informants. Differing definitions of treatment response have been used (e.g. diagnostic status at outcome versus change in symptom severity).
Ginsburg, et al. [25] found that consistent predictors of remission were having good family functioning, male gender, higher socioeconomic status and lower baseline anxiety severity. However, effect sizes were modest, and methodological inadequacies were present (e.g. naturalistic design). Another group [26] examined the influence of genetic, demographic and clinical information on outcomes following cognitive behavioral therapy in child anxiety disorders. They found similar results to Ginsburg, et al. [25] in terms of pre-treatment severity and gender as predictors. However, they also found having comorbid mood and externalizing disorders predicted poorer outcomes, as well as genetic factors over and above clinical and demographic factors moderating treatment response. This variability limits the strength of the conclusions and underscores the need for further work. More evidence is needed on exploring what factors are related to change.
The present study furthers the research in this area by assessing the participants involved in the Hancock, et al. [14] study, 2 years posttreatment. In addition, this study addresses the problem of treatment non-responders (up to 40%–50%, [16]) by investigating predictors of outcomes over time. Identifying predictors of treatment outcome is important in enabling clinicians to better individualize treatment [27]. At baseline, individuals or subgroups can be identified who may be non-respondents and who may benefit from new or refined interventions. It may also help to determine whether certain baseline characteristics are associated with superior outcomes for some treatments over others, in which case individuals may be better matched for certain treatments. From a research point of view, predictors can be helpful in designing studies by identifying potential stratification variables that correlate with primary outcomes [28].
Based on the literature, in particular the findings of the largest RCT of predictors and moderators of treatment outcomes for children with anxiety, the present study evaluated the following potential domains as predictors of outcomes: demographic characteristics, measures of severity, principal anxiety disorder and psychiatric comorbidity, and family functioning psychosocial factors.
Method
Full details of the methodology have been previously reported [14,29]. A brief description follows.
Participants
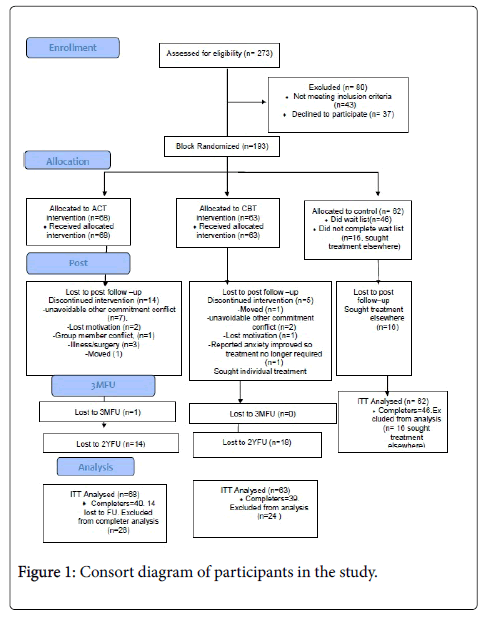
Of the 193 children (54% children 7-11 years and 46% adolescents 12-17 years) initially enrolled who met criteria for one or more anxiety disorders using the Anxiety Disorders Interview Schedule for Children for DSM-IV (ADIS-IV; [30]), randomized to ACT (n=68), CBT (n=63) or wait list control WLC (n=62) conditions, 157 completed treatment, of whom 110 were allocated to ACT or CBT (see patient flow diagram in Figure 1). Follow up was performed for those in ACT and CBT only. Participants were recruited in Sydney, Australia via referrals from school counsellors, parents, word of mouth, and health professionals [14].
Attempts were made to contact all 111 of the ACT and CBT participants who completed the treatment (the WLC received treatment following post assessment so were not followed up), although three could not be located. Of the 108 located, all but three agreed, and 79 completed the 2YFU assessment (the remainder cancelled several times or failed to attend the assessment). Of these, 20 (26%) of participants had received further psychological treatment since the original study. Analysis found these participants to have significantly higher clinical severity rating (CSR) scores at post and 3MFU (t=2.27 and 2.35 respectively, p<0.05) and at the 2YFU (t=3.58, p<0.01), but no significant differences at pre-treatment (t=1.01, p=0.31) or sociodemographically (p>0.05). These participants were included in the final analysis to avoid biasing the results towards more effect. Additionally, this was an exploratory study aimed at identifying the status of all followed up, regardless of whether or not they had received further treatment (Figures 2 and 3).
The 79 final participants (39 ACT, 40 CBT) ranged in age from 9-19 years (x�=12.52, SD=2.82), all having 2 years since treatment. The most common primary diagnosis at baselinne was generalized anxiety disorder (41%), followed by social anxiety disorder (29.5%), separation anxiety disorder (19.2%), specific anxiety disorder (6.4%) and obsessive compulsive disorder (3.8%).
Table 1 shows the demographics and clinical characteristics of the intention-to-treat sample. As seen in Table 2, mean pre CSR was in the severe range, with around 80% being in this category.
| Characteristic | Total (N=193) | ACT (n=68) | CBT (n=63) | Control (n=62) |
|---|---|---|---|---|
| Gender | ||||
| Female | 58% (111) | 54% (37) | 60% (38) | 58% (36) |
| Reported ethnicity | ||||
| Caucasian | 78% (150) | 77% (52) | 78% (49) | 79% (49) |
| European | 7% (14) | 10% (7) | 6% (4) | 5% (3) |
| Middle Eastern | 9% (17) | 7% (5) | 8% (5) | 11% (7) |
| Indian/Sri Lankan/Pakistani | 5% (10) | 3% (2) | 8% (5) | 5% (3) |
| Asian | 1.0% (2) | 2.9% (2) | 0 | 0 |
| Age in years M (SD) | 11.20 (2.76) | 11.15(2.50) | 10.81(2.92) | 11.66 (2.84) |
| Adolescents (12-17 yrs) | 46% (88) | 46% (31) | 40% (25) | 52% (32) |
| Currently on psychotropic med | 3.6% (7) | 7% (5) | 2% (1) | 2% (1) |
| Primary diagnosis | ||||
| Generalized anxiety disorder | 39% (76) | 38% (26) | 37% (23) | 44% (27) |
| Social anxiety disorder | 21% (41) | 25% (17) | 27% (17) | 11% (7) |
| Separation anxiety disorder | 10% (20) | 9% (6) | 18% (11) | 5% (3) |
| Specific anxiety disorder | 8% (15) | 7% (5) | 10% (6) | 7% (4) |
| Obsessive Compulsive Disorder | 6% (12) | 7% (5) | 3% (2) | 8% (5) |
| Agoraphobia without Panic | 1% (1) | 2% (1) | 0 | 0 |
| Co-morbid anxiety disorder | 94% (181) | 93% (63) | 91% (57) | 97% (61) |
| Co-morbid depressive disorder | 18% (35) | 18% (12) | 13% (8) | 24% (15) |
| Co-morbid Axis 2 disorder ADHD | 3% (6) | 2% (1) | 8% (5) | 0 |
| Co-morbid Axis 2 disorder Asp* | 2% (3) | 3% (2) | 2% (1) | 0 |
| Principal disorder clinical | 6.68(0.96) | 6.56 (0.87) | 6.59(1.026) | 6.92 (0.963) |
| severity rating at pre, M (SD) | ||||
| Received previous treatment | 71% (136) | 72% (49) | 78% (49) | 61% (38) |
Note: ACT=acceptance and commitment therapy; CBT=cognitive behavioral therapy; Pre=pre=treatment. *Asp=Asperger Syndrome. Comorbidity was defined as a clinical severity rating of 4 or above on the Anxiety Disorders Interview Schedule-IV (ADIS-IV) for Children.
Table 1: Demographic and Clinical Characteristics of the Intention-to-Treat Sample.
| Measure and condition | Pre-trt | Post-trt | 3-mth post | 2YFU |
|---|---|---|---|---|
| ADIS Clinical Severity Rating | ||||
| ACT | 6.56 (0.87) | 4.31(2.52) | 4.07 (2.43) | 4.20 (2.52) |
| CBT | 6.59 (1.03) | 3.44 (2.86) | 3.12 (2.71) | 3.07 (3.03) |
| WLC | 6.92 (0.96) | 6.18 (1.80) | ||
| MASC Child | ||||
| ACT | 62.21 (14.35) | 54.56 (13.33) | 51.74 (14.00) | 51.62 (13.92) |
| CBT | 59.58 (11.84) | 49.46 (11.56) | 48.85 (10.60) | 49.54 (12.70) |
| WLC | 61.54 (11.60) | 61.23 (11.67) | ||
| MASC Parent | ||||
| ACT | 59.97 (12.10) | 53.59 (11.65) | 51.56 (12.22) | 51.78 (13.17) |
| CBT | 58.64 (10.99) | 50.79 (11.01) | 48.71 (11.86) | 50.41 (13.35) |
| WLC | 57.81 (10.77) | 57.42 (11.67) | ||
| CALIS-Parent Interference | ||||
| ACT | 16.45 (6.19) | 11.15 (5.18) | 10.78 (5.21) | 10.81 (5.07) |
| CBT | 17.08 (5.36) | 13.24 (5.52) | 13.01 (4.78) | 13.24 (5.89) |
| WLC | 17.78 (4.96) | 16.00 (3.41) | ||
| CALIS-Family Interference | ||||
| ACT | 13.07 (7.11) | 9.77 (5.40) | 9.68 (5.51) | 8.56 (4.83) |
| CBT | 14.22 (7.41) | 10.79 (5.88) | 10.93 (5.89) | 10.79 (5.89) |
| WLC | 14.04 (6.74) | 13.22 (3.76) | ||
| AFQ-Avoidance Fusion | ||||
| ACT | 29.43 (14.26) | 22.30 (11.96) | 19.24 (13.49) | 20.03 (13.55) |
| CBT | 30.86 (14.19) | 19.67 (12.02) | 17.81 (10.96) | 18.54 (12.97) |
| WLC | 31.97 (10.96) | 30.53 (13.50) | ||
Note: ADIS=Anxiety Disorders Interview Schedule for Children; MASC=Multidimensional Anxiety Scale for Children; CALIS=Child Anxiety Life Interference Scale; AFQY=Avoidance and Fusion Questionnaire for Youth. Pre=Pre-treatment; Post=Post-treatment; ACT=Acceptance and Commitment therapy; CBT=Cognitive behavioral therapy; WLC=Waitlist control
Table 2: Means and standard deviations (SD) of outcome measures for the three groupsusing intention-to-treat.
Intervention
Participants allocated to ACT or CBT completed a group-based therapy program of 10 x 1.5 hour sessions at no cost. Parents and children both attended each session, with groups for each run concurrently and separate time allowed for working together as a family unit. Treatment was conducted by between two and four psychologists, dependent upon group numbers. Further details on both the treatments and their differences can be found in Swain, et al. [29] and Hancock, et al. [14]. Contact the authors for a program copy.
Main outcome measures
All measures have well-established validity and reliability [29].
Anxiety disorder diagnosis and clinical severity (ADIS-IV)
The ADIS-IV [30,31], was completed by participants and a parent. It produces a CSR between 0-8. Scores of 4 or greater are indicative of clinical disorders, with higher scores reflecting increasing disorder severity (5-6=severe, 7-8=very severe). All ADIS interviews were audio-recorded and inter-rater reliabilities conducted. The � agreement for an overall diagnosis of anxiety disorder was 1, with a range of 0.87 to 0.97 across the major anxiety disorders. The overall CSR severity reliability rating was k=0.76.
Children’s global assessment scale (CGAS)
The CGAS [32] provides a measure of global impairment and functioning with scores ranging from 1 (lowest functioning) to 100 (highest functioning). The CGAS has acceptable psychometric properties [32]. The Intraclass correlation (ICC) was 0.61.
Multidimensional anxiety scale for children (masc)
The MASC is a self and parent-report inventory of anxiety symptoms (MASC-C and MASC-P respectively) including physiological symptoms, avoidance, social and separation anxiety [33,34]. In the present study the average internal consistency of the MASC subscales across the assessment time points was between α=0.83 - 0.86.
The children’s depression inventory (CDI)
The CDI is a self-report measure of depression for children and adolescents aged 8-16 years. It comprises 27 items assessing cognitive, affective and behavioral signs of depression [35,36].
Anxiety life interference: Children’s anxiety life interference scale (CALIS)
The CALIS is a self-report measure that assesses life interference across school, family, peers/friendships, and physical health. Items are rated on a five-point Likert scale from “not at all” to “all the time”. There is a child (CALIS-C) and parent form (CALIS-P), the latter having two subscales. There is also a family interference scale (CALISF) [37]. All three scales were used in this study. Test-retest reliability has been established as moderate (r=0.66 - 0.87) and intra-class correlations acceptable (r=0.38 - 0.74) [37]. Reliability estimates were found to be good at 0.80 and convergent validity has been established [37]. The CALIS-F and CALIS-P were found to demonstrate high internal consistency in the current study (α=0.89 and 0.93). For this paper, only the parent reports are included as there were clinically significant pre-treatment differences between ACT and CBT CALIS-C scores (t114=2.67, p<0.01).
The Avoidance & fusion questionnaire - youth (AFQ-Y)
The AFQ-Y is a 17-item self-report measure of cognitive fusion (“fusion”) and experiential avoidance (EA; the antithesis of acceptance of and defusion from anxious thoughts) for youth, developed for children aged 8-14 years and validated in a sample with an average age of 12.43 years. Internal consistency has been demonstrated [38] and in this sample was good (α=0.87 –0.95) depending upon the assessment time point.
Predictor analysis
Description of predictor variables
Demographic characteristics
Age and gender: Age in years at baseline was examined in the predictor analysis as a continuous variable. We also examined whether results changed when categorized as children versus adolescents, which was negative. Gender was recorded at baseline.
Ethnicity: Parents classified their children into one of the following categories: Caucasian, European, Middle Eastern, Indian/Sri Lankan/ Pakistani, or Asian. There were no African or Aboriginal/Torres Strait Islander participants. The category ‘Australian’ was not used as a category as Australia is a strongly multicultural society with many first and second generation migrants, and all participants were Australian citizens.
Socioeconomic status: Income was not obtained for this study. According to the Australian Index of Relative Socio-economic Disadvantage based on postcodes [39] approximately 16% of the sample were from relatively socio-economically disadvantaged areas (ranking 1-3 out of 10), 41% were middle-range (4-7 out of 10) and 43% were at the upper end of advantage (8-10 out of 10).
Measures of symptom severity: Symptom severity predictor measures included the ADIS-IV, MASC, CALIS and AFQ-Y, and are discussed above in the main outcome measures section.
Family psychosocial factors: McMaster Family Assessment Device (FAD) [40]. The FAD is a 53-item inventory completed by caregivers on the structure, organization and patterns of transactions within families. Six dimensions of family functioning are identified in the model including Problem Solving, Communication, Roles, Affective Responsiveness, Affective Involvement and Behavioral Control. Moderate-to-strong reliabilities have been obtained for the FAD. It also has established discriminant and concurrent validity.
Co-morbidity: Participants were assessed for a range of anxiety disorders using the ADIS. The majority of participants had a comorbid anxiety disorder. They were also assessed for externalising disorders (oppositional defiant disorder, conduct disorder, attentiondeficit/ hyperactivity disorder).
Treatment credibility and parent expectancies: Although treatment credibility and parent expectancies for therapy were assessed using a modified version of the Credibility/Expectancy Questionnaire (CEQ; [41]), complete data was only available for 33% of the initial sample (ACT n=17, CBT n=19). Thus this variable was not entered as a predictor due to the large amount of missing data.
Treatment fidelity and competence: A therapist adherence scale (available from the authors) was developed based on a similar scale to Norton [42]. Overall, the therapists were found to adhere to both treatment protocols. The average adherence rating was 4.37 (SD=0.34) for ACT and 4.50 (SD=0.50) for CBT, with no significant group differences (t18=-0.18, p=0.86). Therapists’ consistency with treatment (i.e. ACT or CBT consistent overall each session) was rated on a dichotomous yes/no scale at each session, in accordance with the relevant treatment. Therapist competence scale scores were measured using a validated sub-scale of an ACT/CBT adherence and competence tool [43]. This scale investigated factors such as “knowledge of treatment”, “skill in delivering treatment”, “relationship with client” and “overall performance”. At the end of each recording, mean ratings on scale items represented the therapist competence for that session, as per Arch, et al. [12]. Results indicated very good therapist skills in both ACT (M=4.32, SD=0.40), and CBT (M=4.36, SD=0.60) with no significant group differences (t18=-0.66, p=0.52).
Therapist allegiance: Upon commencement of the study, therapists were asked to rate therapeutic allegiance by answering the question “Which treatment do you think leads to better outcomes?” Three stated they believed both treatments would be equally effective, two ACT, and one CBT. Thus allegiance was dispersed. All therapists performed both treatments.
Data analysis
Data were analysed using SPSS 19 (IBM, USA) by a statistician who was masked to group status (the data set was decoded for treatment group). Intention-to-treat (ITT; all participants who were allocated to a condition) and completer (only cases with complete data) analyses were conducted using mixed model analyses.
Regarding main outcomes, the only differences in ITT versus completer mixed model results were for the primary outcome – ADISIV – so both results are reported for this variable. Missing data were handled using the last-observation-carried-forward (LOCF) method.
The primary endpoint was the ADIS-IV (measured by CSR and number of diagnoses). Linear mixed model analyses were used to determine differences between groups on continuous measures (pre, post, 3MFU and 2YFU). An unstructured covariance structure, which provided the best fit, was used. Post-hoc comparisons between groups were undertaken using Least Significance Differences.
Exploratory data analyses
Exploratory data analyses ensured assumptions were met for multiple linear regression analysis. The outcome (dependent variable) was CSR 2YFU. Only IVs significantly related to outcome at p<0.05 were entered into a standard multiple regression analysis (all independent variables entered into the equation at the same time). Table 3 shows the significant correlations with outcome, and Table 4 shows all the pretreatment variables tested as correlates and the interrcorrelations between variables and outcome predictor variables. Multiple linear regression analysis was used to identify the best model of predictors of outcome. This is an appropriate analysis when the researcher does not know which independent variables will create the best prediction model. For the predictor analyses, there were some differences between ITT and completer analyses, so results are presented for both analyses. A preliminary analysis indicated that treatment received was not related to regression outcomes for all completer analyses time points, so data is presented for ACT and CBT together. However, ITT analyses at 2YFU are presented separately for groups as there was a significant difference between the two treatment groups on CSR (p<0.05). To adjust for multiple comparisons, predictors were grouped into subsets, including demographic variables, measures of severity, principal anxiety disorder and comorbidity, and family factors. Predictors were considered significant based on a corrected p value of 0.05 or less (two-tailed).
| Category/variable measure | CSR Post (both groups) | CSR 2YFU (both groups) | CSR2YFU | |
|---|---|---|---|---|
| ACT | CBT | |||
| Demographic characteristics | ||||
| Age | 0.18 (0.05)* | 0.15 (0.09) | 0.13 (0.31) | 0.14(0.26) |
| Gender | 0.10 (0.25) | 0.09 (0.31) | 0.18 (0.14) | 0.04(0.79) |
| Socioeconomic status | 0.10 (0.26) | -0.07 (0.45) | 0.06 (0.66) | -0.19(0.13) |
| Ethnicity | 0.06 (0.53) | 0.04 (0.69) | 0.06 (0.63) | 0.10(0.42) |
| Symptom severity | ||||
| CSR pre | 0.20 (0.02)* | 0.13 (0.14) | 0.08 (0.54) | 0.18(0.16) |
| CGAS | 0.01 (0.90) | 0.05 (0.96) | 0.01 (0.95) | 0.07(0.59) |
| MASC (Child) | 0.07 (0.46) | 0.03 (0.77) | -0.19 (0.12) | 0.22(0.08) |
| MASC (parent) | 0.13 (0.13) | 0.12 (0.17) | 0.08 (0.53) | 0.15(0.24) |
| CDI | 0.13 (0.13) | 0.18 (0.04)* | 0.01 (0.95) | 0.34(0.01)* |
| Psychiatric comorbidity | -0.03 (0.71) | -0.08 (0.37) | 0.13 (0.91) | -0.16(0.21) |
| Psychosocial factors | ||||
| FAD Communication | 0.01 (0.90) | 0.15 (0.19) | -0.16(0.21) | 0.19(0.13) |
| FAD Roles | 0.05 (0.55) | 0.02 (0.89) | -0.03(0.79) | 0.06(0.62) |
| FAD | ||||
| Affective Responsiveness | 0.02 (0.79) | 0.02 (0.84) | -0.21(0.08) | -0.02(0.91) |
| FAD Affective Involvement | -0.09 (0.29) | 0.16 (0.17) | -0.20(0.11) | 0.17(0.19) |
| FAD General Functioning | 0.04 (0.63) | 0.15 (0.18) | -0.05(0.67) | 0.10(0.42) |
| Avoidance/Fusion | -0.05 (0.56) | 0.03 (0.70) | -0.09(0.45) | 0.17(0.18) |
| Previous psychological treatment | -0.21 (0.04)* | -0.16 (0.12) | -0.20(0.2) | -0.02(0.91) |
*=significant at p<0.05
Table 3: Baseline predictors of CSR correlations with CSR at post and 2YFU using ITT. All variables are mean continuous scores apart from gender, socioeconomic status, ethnicity, psychiatric co-morbidity and previous psycholgical treatment, which are categorical variables.
| FAD General | SES | Gender | age | ethnicity | Psychological Input pre | co-morbid disorder | MASC Child Total T-score pre | MASC Parent Total T-score pre | CDI Total T-score pre | AFQ-Y Total score pre | CGAS score pre | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Functioning pre | ||||||||||||
| FAD General Functioning pre | 1 | 0.094 | -0.006 | 0.114 | -0.011 | -0.007 | -0.18 | 0.071 | 0.043 | 0.124 | 0.043 | -0.029 |
| -0.09 | -0.29 | -0.94 | -0.2 | -0.9 | 0.948 | -0.04 | -0.42 | -0.63 | -0.16 | -0.63 | -0.74 | |
| SES | 0.094 | 1 | 0.016 | 0.065 | 0.2 | -0.143 | 0.005 | 0.06 | 0.076 | -0.013 | 0.013 | -0.173 |
| -0.29 | -0.86 | -0.47 | -0.02 | -0.16 | -0.96 | -0.5 | -0.39 | -0.88 | -0.89 | -0.05 | ||
| Child's gender | -0.006 | 0.016 | 1 | 0.06 | -0.003 | 0.121 | 0.134 | -0.124 | -0.04 | 0.158 | -0.036 | -0.061 |
| -0.94 | -0.86 | -0.49 | -0.97 | -0.24 | -0.12 | -0.16 | -0.65 | -0.07 | -0.68 | -0.49 | ||
| Child's age at first presentation | 0.114 | 0.065 | 0.06 | 1 | 0.17 | -0.188 | 0.027 | 0.018 | -0.054 | 0.035 | -0.036 | -0.026 |
| -0.2 | -0.47 | -0.49 | (0.05)* | .(06) | -0.76 | -0.84 | -0.54 | -0.69 | -0.69 | -0.78 | ||
| Ethnic background | -0.011 | 0.2 | -0.003 | 0.17 | 1 | -0.187 | -0.015 | -0.169 | -0.048 | -0.082 | -0.074 | 0.042 |
| -0.9 | -0.02 | -0.97 | (0.05)* | -0.06 | -0.86 | (0.05)* | -0.59 | -0.35 | -0.4 | -0.63 | ||
| Psychological Input prior to group | -0.007 | -0.143 | 0.121 | -0.188 | -0.187 | 1 | 0.024 | 0.039 | -0.167 | 0.044 | 0.066 | -0.048 |
| -0.95 | -0.16 | -0.24 | -0.06 | -0.06 | -0.82 | -0.7 | 0.1 | -0.67 | -0.52 | -0.64 | ||
| Presence of a co-morbid disorder | -0.18 | 0.005 | 0.134 | 0.027 | -0.015 | 0.024 | 1 | 0.004 | -0.013 | 0.006 | 0.157 | -0.004 |
| (0.04)* | -0.96 | -0.12 | -0.76 | -0.86 | -0.82 | -0.96 | -0.88 | -0.94 | -0.08 | -0.97 | ||
| MASC Child Total T-score pre | 0.071 | 0.06 | -0.124 | 0.018 | -0.169 | 0.039 | 0.004 | 1 | 0.48 | 0.525 | 0.582 | -0.144 |
| -0.42 | -0.51 | -0.16 | -0.84 | -0.05 | -0.7 | -0.96 | (0.00)* | (0.00)* | (0.00)* | -0.1 | ||
| MASC Parent Total T-score pre | 0.043 | 0.076 | -0.04 | -0.054 | -0.048 | -0.167 | -0.013 | 0.48 | 1 | 0.142 | 0.287 | -0.081 |
| -0.63 | -0.39 | -0.65 | -0.54 | -0.59 | -0.1 | -0.88 | (0.00)* | .(11) | (0.00)* | -0.36 | ||
| CDI Total T-score pre | 0.124 | -0.013 | 0.158 | 0.035 | -0.082 | 0.044 | 0.006 | 0.525 | 0.142 | 1 | 0.641 | -0.143 |
| -0.16 | -0.88 | -0.07 | -0.69 | -0.35 | -0.67 | -0.94 | (0.00)* | -0.11 | (0.00)* | -0.1 | ||
| AFQ-Y Total score pre | 0.043 | 0.013 | -0.036 | -0.036 | -0.074 | 0.066 | 0.157 | 0.582 | 0.287 | 0.641 | 1 | -0.145 |
| -0.63 | -0.89 | -0.68 | -0.68 | -0.4 | -0.52 | -0.08 | (0.00)* | (0.00)* | (0.00)* | -0.1 | ||
| CGAS score pre | -0.029 | -0.173 | -0.061 | -0.026 | 0.042 | -0.048 | -0.004 | -0.144 | -0.081 | -0.143 | -0.145 | 1 |
| -0.74 | (0.05)* | -0.49 | -0.77 | -0.63 | -0.64 | -0.97 | -0.1 | -0.36 | -0.1 | -0.1 |
*significant at p<0.05.
Table 4: Intercorrelations of predictor variables for ITT treatment groups combined.
Power analysis
On the basis of the mean CSR, our sample size had the statistical power to show that an effect size (d) of 0.65 or larger would be statistically significant for the completer analyses and an effect size of 0.50 or larger for the ITT analyses in between group comparisons (power=80%, significance <0.05, two-tailed tests). For the regression analysis, our sample size had the statistical power to show that a correlation coefficient (r) of >0.35 was significant.
Results
Pre-treatment comparisons
As previously reported there were no significant differences across groups for any socio-demographic variable (ps>=0.13).
Main outcomes
Means and standard deviations are presented in Table 2. Effect sizes for within- and between-group change from pre- to post are listed by group in Table 5 (and at follow-up within text. Effect sizes for Cohen’s d for within-group differences were calculated using the mean differences of pre- and post-scores for within-groups divided by the baseline standard deviation (SD; [44]). Effect sizes for comparison between the treatment groups were performed using Cohen’s d but using the pooled standard deviations of the two groups. Cohen’s criteria for effect sizes was used for this study, with 0.2=small, 0.5=medium, and 0.8=large. To determine whether there were significant demographic differences between those children who completed the 2YFU and those who completed treatment, we conducted a number of t tests and chi square analyses. Results showed that the two groups did not differ in terms of gender, χ2 (1, N=111)=2.39, ethnicity, χ2 (4, N=111)=4.90, previous psychological treatment χ2 (2, N=111)=5.08, treatment group type χ2 (1, N=111)=0.18, receiving psychotropic medication χ2 (1, N=111)=0.78, and co-morbid axis 1 disorder χ2 (1, N=111)=0.03 (all ps>0.08). Independent t-tests demonstrated no significant differences between those followed up long term and those not in terms of age (t=1.51, df=109, p=0.56), pre-treatment ADIS CSR (t=0.54, p=0.59), or MASC (t=-0.85, 109, p=0.39).
| Measure and condition | ES 3MFU to 2YFU within (d) | ES 2YFU ACT vs. CBT (d) |
|---|---|---|
| ADIS Clinical Severity Rating | ||
| ACT | -0.04 (-0.48-0.39) | 0.40 (-0.04-0.85)(ITT) |
| CBT | 0.02(-0.43-0.46) | 0.20 (-0.25-0.66) (completers) |
| MASC Child | ||
| ACT | 0.01 (-0.43-0.45) | 0.15 (-0.29- .60) |
| CBT | -0.06 (-0.05-0.38) | |
| MASC PARENT | ||
| ACT | 0.23 (-0.21-0.68) | 0.23 (0.10-0.59) |
| CBT | -0.13 (-0.58-0.31) | |
| CALIS-Parent Interference | ||
| ACT | 0.0 (-0.44-0.43) | 0.44 (0.01-0.42) |
| CBT | - 0.04 (0.04 -0.40) | |
| CALIS-Family Interference | ||
| ACT | 0.21 (0.23-0.66) | 0.42 (0.03-0.86) |
| CBT | 0.05(-0.4-0.49) | |
| AFQ-Avoidance Fusion | ||
| ACT | -0.08(-0.52-0.36) | 0.11(-0.33-0.55) |
| CBT | -0.06(-0.50-0.38) |
Note: ADIS=Anxiety Disorders Interview Schedule for Children; MASC=Multidimensional Anxiety Scale for Children; CALIS=Child Anxiety Life Interference Scale; AFQY=Avoidance and Fusion Questionnaire for Youth. Pre=Pre-treatment; Post=Posttreatment; ACT=Acceptance and Commitment therapy; CBT=Cognitive behavioural therapy; WLC=Waitlist control d=Cohen’s d, Δ=Glass’s delta, ES=Effect Size
Table 5: Effect sizes (ES) of outcome measures for within and between groups for the three groups using intention-to-treat. Confidence intervals for main outcomes are in parentheses.
ADIS-IV Anxiety disorder diagnosis and clinical severity (CSR)
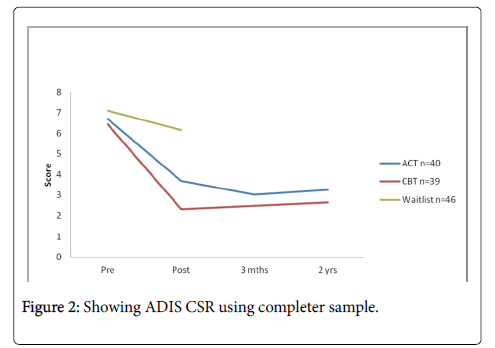
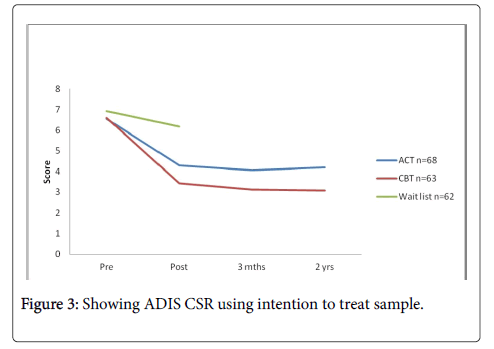
Figures 2 and 3 show the changes over time in CSR means using ITT and completer analyses respectively. There were significant main effects for time for CSR based on both completer (F3,73.49=99.64, p<0.001 ) and the ITT samples (F3,127.90=78.29, p<0.001). Post hoc comparisons comparing 3MFU versus 2YFU results revealed no significant differences for either ACT (p=0.70, d=-0.04) or CBT (p=0.74, d=0.02). There were significant group effects for completers (F1,73.96=3.94, p=0.051 F1,128.67=6.33, p=0.013-ITT ), but no significant group x time interactions (F3,127.90=2.49, p=0.07 for ITT; F3,73.49=1.44, p=0.24 for completers). There were significant treatment group differences at the 2YFU for ITT (p=0.02, d=0.40) but not completers (p=0.38, d=0.20).
Anxiety (MASC-C/P)
MASC-C results showed no significant main effect for groups (F1,129.02=2.98, p=0.87), but significant improvements in scores over time (F3,128.91=28.90, p<0.001). There was no significant group x time interaction (F3,128.91=0.99, p=0.39). Post hoc comparisons comparing 3MFU versus 2YFU results revealed no significant differences for either ACT (p=0.97, d=0.01) or CBT (p=0.68, d=-0.06).There were no significant treatment group differences at the 2YFU (p=0.53, d=0.15). Similar results were found for MASC –P, no significant main effect for groups (F1,129.16=1.53, p=0.22), but significant time improvement effects (F3,128.02=28.47, p<0.001). There was no significant group x time interaction (F3,128.03=.33, p=0.80). Post hoc comparisons comparing 3MFU versus 2YFU results revealed no significant differences for either ACT (p=0.66, d=0.01) or CBT (p=0.70, d=-0.06).
Anxiety life interference (CALIS-P/F)
The CALIS-P showed a significant group (F1,114.00=5.59, p=0.02), and time main effect (F3,114.00=26.05, p<0.001). There was no significant group x time interaction (F3,114.00=0.92, p=0.43). For the CALIS-F, there was a significant time effect (F1,114.00=12.37, p<0.001), but not group (F1,114.00=2.31, p=0.13) or interaction (F3,114.00=0.78, p=0.51). Post hoc comparisons comparing 3MFU versus 2YFU results revealed no significant differences for either ACT (p=0.12) or CBT (p=0.67) for CALIS-P. There were significant treatment group differences at the 2YFU, with a moderate effect size favoring ACT over CBT (p=0.05, d=0.42 for CALIS-F, p=0.02, d=0.42 for CALIS-P).
Acceptance and defusion (AFQ-Y)
For the AFQ-Y, there was no significant group main effect (F1,128.18=0.31, p=0.58), or interaction (F3,126.72=1.06, p=0.37). There was a significant improvement over time overall (F3,126.72=26.67, p<0.001). Post hoc comparisons comparing 3MFU versus 2YFU results revealed no significant differences for either ACT (p=0.59, d=-0.08) or CBT (p=0.58, d=-0.06). There were no significant treatment group differences at the 2YFU (p=0.55, d=0.11).
Anxiety life interference (CALIS-P/F)
The CALIS-P showed a significant group (F1,114.00=5.59, p=0.02), and time main effect (F3,114.00=26.05, p<0.001). There was no significant group x time interaction (F3,114.00=0.92, p=0.43). For the CALIS-F, there was a significant time effect (F1,114.00=12.37, p<0.001), but not group (F1,114.00=2.31, p=0.13) or interaction (F3,114.00=0.78, p=0.51). Post hoc comparisons comparing 3MFU versus 2YFU results revealed no significant differences for either ACT (p=0.12) or CBT (p=0.67) for CALIS-P. There were significant treatment group differences at the 2YFU, with a moderate effect size favoring ACT over CBT (p=0.05, d=0.42 for CALIS-F, p=0.02, d=0.42 for CALIS-P).
Acceptance and defusion (AFQ-Y)
For the AFQ-Y, there was no significant group main effect (F1,128.18=0.31, p=0.58), or interaction (F3,126.72=1.06, p=0.37). There was a significant improvement over time overall (F3,126.72=26.67, p<0.001). Post hoc comparisons comparing 3MFU versus 2YFU results revealed no significant differences for either ACT (p=0.59, d=-0.08) or CBT (p=0.58, d=-0.06). There were no significant treatment group differences at the 2YFU (p=0.55, d=0.11).
Clinical significance
Clinical significance was determined with the Jacobson and Truax [45] model. It is commonly accepted to report clinical significance for those who completed the study [46], thus analysis of recovery rates was based on completers. Due to the large amount of variables in this study, clinical significance is presented for the ADIS-IV only. Groups were analysed according to those who scored less than 4 (i.e. the cutoff for no longer meeting criteria for an anxiety disorder) on the CSR. The percentage of children who no longer met criteria for an anxiety disorder at post were 31.5% for ACT and 45% CBT, at 3MFU 37% ACT and 54.4% CBT, and at the 2YFU 45% ACT and 60 % CBT were diagnosis free. Chi-square analyses identified no significant differences between ACT and CBT in the frequency of children without an anxiety diagnosis across time (p=0.33 post, p=0.07 3MFU, p=0.65 2YFU).
Multiple regression results
Intention to treat analyses: Correlations between all of the predictor and outcome variables are presented in Table 4, and inter-correlations of the predictors in Table 5. A preliminary analysis revealed none of the subtests of the FAD were significantly correlated with CSR post or 2YFU, so for brevity only FAD General Functioning results are presented in Table 3.
Post ITT results: Outcome variable CSR post correlated significantly with CSR pre (r=0.20, p<0.05) and age (r=0.18, p=0.05). These predictors were added into a regression analysis with CSR post the criterion variable. Together, the predictors explained 6.2% of the variance in CSR post scores, which was significant (F2,128=4.22, p0.05). CSR pre, B=0.51, (SE=0.25) (95% CI 0.02-1.00), b=0.18, t (2,128)=2.06, p<0.05, was a significant unique predictor of CSR post, predicting 3.2% but age just dropped out as a uniquely significant predictor, B=0.15, (SE=0.09) (95% CI -0.02-0.32), b=0.15, t=1.73, p=0.08).
2YFU ITT results: For ACT at the 2YFU, none of the predictor variables significantly correlated with outcome. For CBT, only CDI pre (r=0.34, p<0.001) and taking antidepressant medication (ANTI, r=-0.28, p<0.05) significantly correlated with CSR 2YFU. Together CDI and ANTI contributed 17% to variance in regression scores, which was significant (F2,59=6.24, p<0.05). CDI, B=.078, (SE=.03), (95% CI 0.01-0.18), t=2.60, p<0.05, b=0.31, was a significant predictor, with unique variance 10.3%. ANTI, B=-2.08, (SE=1.01), (95% CI -4.1-0.45), t=-2.05, p<0.05, b=-0.25, was also a significant unique predictor, explaining 6.7% of variance in scores.
Completer analyses
Post completers: Outcome variable CSR post correlated significantly with CSR pre (r=0.24, p<0.05) and MASC-P pre (r=0.31, p=0.01). When both predictors were entered, CSR-pre dropped out as a significant predictor in the regression analysis. Thus, the best model was MASC-pre, explaining 9.3% of the variance in CSR post scores, which was significant (F1,75=7.70, p0.01), B=0.72, (SE=0.26) (95% CI 0.02-1.00), b=0.30, t=2.78, p<0.01.
2YFU completers: None of the baseline variables entered significantly correlated with CSR at 2YFU using completer analyses.
Discussion
The purpose of this paper was to evaluate the long-term effectiveness of group-based ACT for mixed anxiety disorders among children, and identify baseline predictors of outcome. To our knowledge this is the first RCT to investigate ACT for anxiety in children, and with long term follow-up data. The study demonstrated positive findings for both ACT and its comparison group CBT in terms of long-term maintenance of gains, but inconsistent findings regarding predictor outcomes.
For all the measures, improvements at post and 3MFU were maintained at the 2YFU for both ACT and CBT. In support of ACT being an empirically-supported treatment option with long-term benefits for anxious youths, completer analyses showed both ACT and CBT produced highly significant reductions in CSR maintained at 3MFU and 2YFU. Means were neither statistically or clinically different over time overall when comparing ACT and CBT. However, using ITT data, there was a moderate effect size favoring CBT over ACT at the 2YFU, but a small one using completer data. It is possible that there were power limitations related to completer data (around 80% of the sample, N=79) and this is an area for further research. Nonetheless, findings were positive for both groups and this is reinforced by similar improvements on the MASC, as both groups’ mean scores were in the normal range (i.e. not meeting criteria for an anxiety disorder).
Not only were treatment gains maintained for both groups over time, there was evidence of continued improvement with 45% of ACT and 60% of CBT participants diagnosis free at the 2YFU. This is in keeping with the findings of other studies that reported treatment gains to be more evident a few months post treatment [21-23]. Although the proportion of participants diagnosis free at 2YFU was not statistically different, a larger sample size may have increased the power to detect significant findings, as there was a trend towards a greater proportion of CBT participants being diagnosis free. The life interference outcome (CALIS) for both treatments produced similarly positive results, with significant gains maintained at 2YFU. Effect sizes for CALIS outcomes at follow up favored ACT over CBT, which is in keeping with the acute phase findings, and reflects the emphasis of ACT on improving quality of life [47]. However means were not statistically different. This is consistent with the findings of other studies [22,48].
AFQ-Y findings were in line with those emerging up to 3MFU, as previously reported [14], with both ACT and CBT having similarly positive outcomes. This supports the possibility that defusion and restructuring strategies are simply different tools that can be used to change behavior when problematic thoughts and feelings arise, rather than one being superior to the other. However, this being an exploratory study means that such conclusions cannot be drawn. Age was not significantly related to treatment outcomes when comparing treatment groups, with the same pattern of results observed for younger children and adolescents. This result is consistent with the acute phase findings [14], as well as those of Ginsburg, et al. [25] and Hudson, et al. [26], challenging motivational and engagement issues frequently perceived to be present in adolescents [49].
Although the predictor regression analysis identified CSR pre as a predictor at post, this finding did not appear at 2YFU for either ITT or completer analyses. The literature, though mixed, does support pre anxiety severity as a predictor of treatment success [16]. In our study, a closer inspection of CSR-pre scores indicates that around 80% of the participants in our study were in the severe category pre-treatment, limiting the extent to which severity could be fully tested as a predictor. On the positive side however, the finding that participants’ outcomes were as a group so greatly improved and maintained in the long term is an impressive result for both treatments.
It is curious that baseline depressive mood score (CDI) and antidepressant treatment emerged as significant predictors for the ITT analysis at 2YFU for CBT, but there were no significant predictors for ACT using ITT or for either group using completer 2YFU. These findings give some support to those of previous studies that found that children with comorbid disorders were more likely to have poorer outcomes following anxiety treatment with CBT [26]. Antidepressant treatment has not been studied closely apart from the CAMS study [25], hence its predictive value for long term outcomes is unclear. It is logical that children with higher severity or who have not responded previously would be more likely to have been taking antidepressant drug treatment, but our study does not provide firm evidence for this hypothesis- these variables were not significant predictors in any other analysis conducted in this study, and given they only contributed around 17% of the variance in outcome scores, their validity as a predictor remains tentative. In fact, none of the significant predictors explained more than 10% of the variance in outcome in any analysis, so it appears that in spite of the broad areas of baseline predictors explored, a good model explaining variance in CSR outcome scores could not be identified, particularly in the long term. Thus, the question as to why treatment is ineffective in some children or why some children relapse still remains unclear. It may also be that a power problem for the 2YFU ITT analysis may have contributed to nonsignificant findings, since both treatment groups were analysed separately and sample size was reduced. The study was powered to detect a medium effect size for ITT and medium to large for completers. As it is likely that the effect size difference would be small for ACT versus CBT, a larger sample size likely is needed to confirm the current findings.
A possible explanation for age being a predictor at post ITT analysis but not completer is that ITT is a conservative measure, resulting in greater power to detect significant findings. Furthermore, the unique contribution of age to ITT post CSR variance was small. These findings are in line with other studies that have failed to identify age as a consistent predictor of outcomes [25,26].
Family functioning did not emerge as a significant predictor, in contrast to Ginsburg, et al. [25] who found that children whose parents reported that their family had clear rules, more trust, and higherquality interactions at baseline were more likely to be in remission at long-term follow-up.
Limitations
Methodological limitations in this study have been discussed previously [14]. Further limitations specific to the long term follow up are that only three quarters of those who completed treatment were assessed at the 2YFU, and around one quarter of those had received further treatment. This limits the extent to which longer term outcomes can be attributed to treatment received in this study. However, compared with most long-term follow-up studies of children treated for anxiety disorders, this is a high success rate. A more normal distribution of pre-treatment severity may have increased the study’s ability to determine the effect of this variable in explaining variance in scores. It may also be that having a greater severity pre-treatment means that more intensive or longer treatment is needed for superior outcomes.
An additional limitation is that we did not measure parental psychopathology- only family functioning was measured. Our measure of family functioning relied solely on a self-report questionnaire which may have led to underreporting of parent symptoms, thus reducing the strength of this variable as a unique predictor of child outcome [50,51]. Another weakness is that we did not measure income as indicator of SES, so our measure was rudimentary.
Our study also did not assess the wait list control group beyond the immediate post treatment period (due to ethical issues of withholding treatment). Thus we cannot dismiss the possibility that maturation or the passage of time may have improved symptoms. However, this pattern is not supported by evidence-based research, with anxiety disorders in children considered gateway disorders in predicting adult mental health problems [25,52-55].
The finding that 25% of the sample received additional psychological treatment over the follow up period prevented us being able to examine the absolute and relative effectiveness of the two treatments [56-60]. The decision to retain the participants’ data who had received treatment since therapy was based on two factors: one was that these participants had higher severity levels at the 2YFU than those who had not sought further treatment, and excluding their data may have biased findings in favor of a positive treatment effect. Secondly, this was a naturalistic follow up rather than a focus only on those who did not seek extra treatment following therapy. The finding that those who had sought further treatment were more likely to be those who had relapsed or not benefited from treatment in the first place is not surprising, since they would likely have sought further treatment for the problem. As alluded to above, it may be that the reason there was no such relationship found between CSR pre and seeking treatment following this study’s intervention is that the majority of participants were in the severe category pre- treatment [61-79].
Implications for research, policy and practice
To our knowledge this is the largest RCT to date evaluating ACT for children with anxiety. We had limited power to detect treatment group differences, so larger sample sizes are needed to adequately compare the effectiveness of ACT versus CBT, or for that matter, any active treatment given that they are small effect sizes that are likely to be detected. It may also shed further light on whether it matters what type of treatment is used [51].
Notwithstanding the above limitations, our study suggests that the beneficial effects of both ACT and CBT for anxiety disorders in children and young people are maintained two years post treatment, with more children diagnosis free over time. Additional variables and more rigorous measures of some of the predictors may need to be explored to identify predictors of long term outcomes.
References
- Goldstein RB, Olfson M, Wickramaratne PJ, Wolk SI (2006) Use of outpatient mental health services by depressed and anxious children as they grow up. Psychiatr Serv 57: 966-975.
- Creswell C, Waite P, Cooper PJ (2014) Assessment and management of anxiety disorders in children and adolescents. Arch Dis Child 99: 674-678
- Piacentini J, Bennett S, Compton SN, Kendall PC, Birmaher B, et al. (2014) 24- and 36-week outcomes for the Child/Adolescent Anxiety Multimodal Study (CAMS). J Am Acad Child Adolesc Psychiatry 53: 297-310.
- Fletcher L, Hayes SC (2005) Relational frame theory, acceptance and commitment therapy, and a functional analytic definition of mindfulness. J Rational-Emotive & Cogn-Behav Ther 23: 315-336.
- Otte C (2011) Cognitive behavioral therapy in anxiety disorders: current state of the evidence. Dialogues Clin Neurosci 13: 413-421.
- Swain J, Hancock K, Hainsworth C, Bowman J (2013) Acceptance and commitment therapy in the treatment of anxiety: a systematic review. Clin Psychol Rev 33: 965-978.
- Armstrong AB, Morrison KL, Twohig MP (2013) A preliminary investigation of Acceptance and Commitment Therapy for adolescent obsessive-compulsive disorder. J Cogn Psychot 27: 175-190.
- Brown FJ, Hooper S (2009) Acceptance and Commitment Therapy (ACT) with a learning disabled young person experiencing anxious and obsessive thoughts. J Intellectual Disabil 13: 195-201.
- Woidneck MR, Morrison KL, Twohig MP (2014) Acceptance and Commitment Therapy for the Treatment of Posttraumatic Stress Among Adolescents. Behav Modif 38: 451-476.
- Swain J, Hancock K, Dixon A, Bowman J (2014) Acceptance and Commitment Therapy for children: A systematic review of intervention studies. J Contextual Behav Sci 4: 73-85.
- Ruiz FJ (2012) Acceptance and Commitment Therapy versus traditional Cognitive Behavioural Therapy: A systematic review and meta-analysis of current empirical evidence. Int J Psychol Psychol Ther 12: 333-357.
- Arch JJ, Eifert GH, Davies C, Plumb JC, Rose RD, et al. (2012) Randomized clinical trial of Cognitive Behavioral Therapy (CBT) versus Acceptance and Commitment Therapy (ACT) for mixed anxiety disorders. J Consult Clin Psychol 80: 750-765.
- Forman EM, Shaw JA, Goetter EM, Herbert JD, Park JA, et al. (2012) Long-term follow-up of a randomized controlled trial comparing Acceptance and Commitment Therapy and standard Cognitive Behavior Therapy for anxiety and depression. Behav Ther 43: 801-811.
- Hancock K, Swain J, Hainsworth C, Dixon A, Koo S, et al. (2016) Acceptance and Commitment Therapy versus Cognitive Behavior Therapy for Children With Anxiety: Outcomes of a Randomized Controlled Trial. J Clin Child Adolesc Psychol
- Barmish AJ, Kendall PC (2005) Should parents be co-clients in cognitive-behavioral therapy for anxious youth? J Clin Child Adol Psychol 34: 569-81.
- Compton SN, March JS, Brent D, Albano AM, Weersing VR, et al. (2004) Cognitive-behavioral psychotherapy for anxiety and depressive disorders in children and adolescents: an evidence-based medicine review. J Am Acad Child Adolesc Psychiatry 43: 930-959.
- Walkup JT, Albano AM, Piacentini J, Birmaher B, Compton SN, et al. (2008) Cognitive behavioral therapy, sertraline, or a combination in childhood anxiety. New Eng J Med 359: 2753-66.
- Kendall PC, Southam-Gerow MA (1996) Long-term follow-up of a cognitive-behavioral therapy for anxiety-disordered youth. J Consult Clin Psychol 64: 724-730.
- Barrett PM, Duffy AL, Dadds MR, Rapee RM (2001) Cognitive-behavioral treatment of anxiety disorders in children: long-term (6-year) follow-up. J Consult Clin Psychol 69: 135-141.
- Kendall PC (1994) Treating anxiety disorders in children. Results of a randomized clinical trial. J Consult Clin Psychol 62: 100-110.
- Hayes L, Boyd CP, Sewell J (2011) Acceptance and Commitment Therapy for the Treatment of Adolescent Depression: A Pilot Study in a Psychiatric Outpatient Setting. Mindfulness 2: 86-94.
- Metzler C, Biglan A, Noell J, Ary D, Ochs L (2000) A randomized controlled trial of a behavioural intervention to reduce high-risk sexual behaviour among adolescents in high-risk sexual behaviour among adolescents in STD clinics. Behav Ther 31: 27-54.
- Wicksell RK, Melin L, Lekander M, Olsson GL (2009) Evaluating the effectiveness of exposure and acceptance strategies to improve functioning and quality of life in longstanding pediatric pain – A randomized controlled trial. Pain 141: 248-257.
- Burke CA (2010) Mindfulness-based approaches with children and adolescents: A preliminary review of current research in an emergent field. J Child Family Stud 19: 133-144.
- Ginsburg GS, Becker EM, Keeton CP, Sakololsky D, Piacentini J, et al. (2008) Psychological inflexibility in childhood and adolescence: Development and evaluation of the Avoidance and Fusion Questionnaire for Youth. Psychol Assess 20: 93-102.
- Hudson JL, Lester KJ, Lewis CM, Tropeano M, Creswell C, et al. (2013) Predicting outcomes foloowing cognitive behaavior therapy in child anxiety disorders: the influence of genetic, demongraphic and clinical information. J Child Psychol Psychiat 54: 1086-1094.
- Kazdin AE (2007) Mediators and mechanisms of change in psychotherapy research. Annu Rev Clin Psychol 3: 1-27.
- Kernan WN, Viscoli CM, Makuch RW, Brass LM, Horwitz RI (1999) Stratified randomization for clinical trials. J Clin Epidemiol 52: 19-26.
- Swain J, Hancock K, Dixon A, Koo S, Hainsworth C, et al. (2013) Acceptance and Commitment Therapy for anxious children and adolescents: Study protocol for a randomized controlled trial. Trials 14: 140-152.
- Albano AM, Silverman WK (1996) Anxiety Disorders Interview Schedule for DSM-IV Child Version: Clinician's Manual. Oxford University Press, New York.
- Grills AE, Ollendick TH (2003) Multiple informant agreement and the Anxiety Disorders Interview Schedule for parents and children. J Am Acad Child Adolesc Psychiatry 42: 30-40.
- Shaffer D, Gould MS, Brasic J, Ambrosini P, Fisher P, et al. (1983) A children's global assessment scale (CGAS). Arch Gen Psychiat 40: 1228-1231.
- March JS, Sullivan K (1999) Test-retest reliability of the Multidimensional Anxiety Scale for Children. J Anxiety Disord 13: 349-358.
- Rynn MA, Barber JP, Khalid-Khan S, Siqueland L, Dembiski M, et al. (2006) The psychometric properties of the MASC in a pediatric psychiatric sample. Anxiety Disord 20: 139-157.
- Carey MP, Faulstich ME, Gresham FM, Ruggiero L, Enyart P (1987) Children's Depression Inventory: construct and discriminant validity across clinical and nonreferred (control) populations. J Consult Clin Psychol 55: 755-61.
- Saylor CF, Finch AJ Jr, McIntosh JA (1988) Self-reported depression in psychiatric, pediatric and normal populations. Child Psychiat Human Develop 18: 250-4.
- Lyneham HJ, Sburlati ES, Abbott MJ, Rapee RM, Hudson JL, et al. (2013) Psychometric properties of the Children’s Anxiety Life Interference Scale (CALIS). J Anxiety Disord 27: 711- 719.
- Silverman WK, Saavedra LM, Pina AA (2001) Test-Retest reliability of anxiety symptoms and diagnoses with the Anxiety Disorders Interview Schedule for DSM-IV: Child and parent versions. J Am Acad Child Adolesc Psychiatry40: 937-944.
- Australian Bureau of Statistics (2013) Socio-economic Indexes for Areas (SIEFA). Technical Paper 2011.
- Epstein NB, Baldwin LM, Bishop DS (1983) The McMaster Family Assessment Device. J Marital Fam Ther 9: 171-180.
- Devilly CJ, Borkovec TD (2000) Psychometric properties of the credibility/expectancy questionnaire. J Behav Ther Exp Psychiatry 31: 73-86.
- Norton P (2012) A randomized clinical trial of transdiagnostic cognitive-behavioral treatments for anxiety disorder by comparison to relaxation training. Behav Ther 43: 506-517.
- McGrath KB, Forman EM, Herbert JD (2013) Development and validation of of the ACT/CT Adherence and Competence Rating Scale. Manuscript in preparation.
- Jacobson NS, Truax P (1991) Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. J Consult Clin Psychol 59: 12-9.
- Forman EM, Chapman JE, Herbert JD, Goetter EM, Yuen EK, et al. (2012) Using session-by-session measurement to compare mechanisms of action for Acceptance and Commitment Therapy and Cognitive Therapy. Behav Ther 43: 341-354.
- Hayes SC (2004) Acceptance and Commitment Therapy, Relational Frame Theory and the third wave of behavioural and cognitive therapies. Behav Ther 35: 639-665.
- Segool NK, Carlson JS (2008) Efficacy of cognitive-behavioral and pharmacological treatments for children with social anxiety. Depress Anxiety 25: 620-631.
- Oetzel K, Bolton S, David G (2003) Therapeutic Engagement with Adolescents in Psychotherapy. Psychother: Theor, Res, Pract, Training 40: 215-225.
- Bögels SM, Brechman-Toussaint ML (2006) Family issues in child anxiety: attachment, family functioning, parental rearing and beliefs. Clin Psychol Rev 26: 834-56.
- James AC, James G, Cowdrey FA, Soler A, Choke A (2015) Cognitive behavioural therapy for anxiety disorders in children and adolescents (review). Cochrane Lib 6: 1-85.
- Bluett EJ, Homan KJ, Morrison KL, Levin ME, Twohig MP (2014) Acceptance and commitment therapy for anxiety and OCD spectrum disorders: an empirical review. J Anxiety Disord 28: 612-624.
- Cox W, Pavletich H (2015) 11h Annual Demographia International Housing Affordability Survey.
- O'Brien K, Larson C, Murrell A (2008) Third-wave behavior therapies for children and adolescents: progress, challenges and future directions. In: Hayes LAGSC (Edn), Acceptance and mindfulness treatments for children and adolescents. New Harbinger and Context Press Publications, Oakland, CA.
- Gaudiano BA (2011) A review of Acceptance and Commitment Therapy (ACT) and recommendations for continued scientific advancement. Sci Rev Ment Health Pract 8: 5-22.
- Butler AC, Chapman JE, Forman EM, Beck AT (2006) The empirical status of cognitive-behavioral therapy: a review of meta-analyses. Clin Psychol Rev 26: 17-31.
- Coyne LW, McHugh L, Martinez ER (2011) Acceptance and commitment therapy (ACT): Advances and applications with children, adolescents, and families. Child Adolesc Psychiatr Clin N Am 20: 379-399.
- Dunlop WP, Cortina JM, Vaslow JB, Burke MJ (1996) Meta-analysis of experiments with matched groups or repeated measures designs. Psychol Meth 1: 170-177.
- Ellis A (1962) Reason and emotion in psychotherapy. Lyle Stuart, New York.
- Harris R (2009) ACT made simple: An easy-to-read primer on Acceptance and Commitment Therapy. New Harbinger Publications, Inc., California.
- Hedges LV (1981) Distribution theory for Glass's estimator of effect size and related estimators. J Educ Stat 6: 107-128.
- Herbert JD, Forman EM (2011) The evolution of cognitive behavior therapy: The rise of psychological acceptance and mindfulness. In: Forman JD (Edn), Acceptance and mindfulness in cognitive behavior therapy: Understanding and applying the new therapies. (pp. 3-25). John Wiley and Sons, New Jersey.
- Hofmann SG, Asmundson GJ (2008) Acceptance and mindfulness-based therapy: new wave or old hat? Clin Psychol Rev 28: 1-16.
- Hofmann SG, Meuret AE, Rosenfield D, Suvak MK, Barlow DH, et al. (2007) Preliminary evidence for cognitive mediation during cognitive behavioural therapy of panic disorder. J Consult Clin Psychol 75: 374-379.
- Kraemer HC, Wilson GT, Fairburn CG, Agras WS (2002) Mediators and moderators of treatment effects in randomized clinical trials. Arch Gen Psychiatry 59: 877-883.
- Landgraf JM, Abetz L, Ware JE (1999) The CHQ User's Manual. Health Act, Boston, MA.
- Lee J, Semple RJ, Rosa D, Miller L (2008) Mindfulness-based cognitive therapy for children: Results of a pilot study. J Cogn Psychother 22: 15-28.
- Luoma JB, Hayes SC, Walser RD (2007) Learning ACT: An Acceptance and Commitment therapy Skills-Training Manual for Therapists. New Harbinger Publications Inc., Oakland, CA.
- Masuda A, Cohen LL, Wicksell RK, Kemani MK, Johnson A (2011) A case study: Acceptance and commitment therapy for pediatric sickle cell disease. J Pediat Psychol 36: 398-408.
- Meuret AE, Rosenfield D, Hofmann SG, Seidel A, Bhaskara L (2010) Respiratory and cognitive mediators of treatment change in panic disorder: evidence for intervention specificity. J Consult Clin Psychol 78: 691-704.
- Najman JM, Bampton M (1991) An ASCO based occupational status hierarchy for Australia: A research note. Aus New Zeal J Sociol 27: 218-230.
- Nilsen TS, Eisemann M, Kvernmo S (2013) Predictors and moderators of outcome in child and adolescent anxiety and depression: A systematic review of psychological treatment studies. Eur Child Adol Psychiat 22: 69-87.
- Rapee RM, Lyneham HJ, Schniering CA, Wuthrich V, Abbott MJ, et al. (2006) The Cool Kids® Child and Adolescent Anxiety Program Therapist Manual. Centre for Emotional Health, Macquarie University, Sydney.
- Seligman LD, Ollendick TH (2011) Cognitive-behavioral therapy for anxiety disorders in youth. Child Adolesc Psychiatr Clin N Am 20: 217-238.
- Semple RJ, Lee J, Rosa D, Miller LF (2010) A randomized trial of mindfulness-based cognitive therapy for children: Promoting mindful attention to enhance social-emotional resiliency in children. J Child Fam Stud 19: 218-229.
- Semple RJ, Reid EF, Miller L (2005) Treating anxiety with mindfulness: An open trial of mindfulness training for anxious children. J Cogn Psychother 19: 379-392.
- Smits JA, Rosenfield D, McDonald R, Telch MJ (2006) Cognitive mechanisms of social anxiety reduction: an examination of specificity and temporality. J Consult Clin Psychol 74: 1203-1212.
- Thulin U, Svirsky L, Serlachius E, Andersson G, Ost LG (2014) The effect of parent involvement in the treatment of anxiety disorders in children: a meta-analysis. Cogn Behav Ther 43: 185-200.
- Wuthrich VM, Rapee RM, Cunningham MJ, Lyneham MJ, Hudson JL, et al. (2012) A randomized controlled trial of the Cool Teens CD-rom computerised program for adolescent anxiety. J Am Acad Child Adolesc Psychiatry 51: 261-270.
Citation: Hancock K, Swain J, Hainsworth C, Koo S, Dixon A (2016) Long Term Follow up in Children with Anxiety Disorders Treated with Acceptance and Commitment Therapy or Cognitive Behavioral Therapy: Outcomes and Predictors. J Child Adolesc Behav 4: 317. DOI: 10.4172/2375-4494.1000317
Copyright: © 2016 Hancock K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 14902
- [From(publication date): 10-2016 - Apr 04, 2025]
- Breakdown by view type
- HTML page views: 13820
- PDF downloads: 1082