Case Report Open Access
Liver Transplantation for High Output Heart Failure Secondary to HHT: A Case Report and Review of the Literature
Saleh Elwir1*, Cindy M. Martin2, Srinath Chinnakotla3, Mark Reding4, John Lake1 and Mohamed Hassan1
1Division of Gastroenterology, Hepatology and Nutrition, University of Minnesota, Minneapolis, Minnesota, USA
2Cardiovascular Division, University of Minnesota, Minneapolis, Minnesota, USA
3Division of Transplantation, University of Minnesota, Minneapolis, Minnesota, USA
4Division of Hematology, Oncology and Transplantation, University of Minnesota, Minneapolis, Minnesota, USA
- *Corresponding Author:
- Saleh Elwir MD
Gastroenterology and Hepatology Fellow
Division of Gastroenterology, Hepatology and Nutrition
University of Minnesota, 406 Harvard St. SE
MMC 36, Minneapolis, MN, 55455, USA
Tel: 612-625-8999
Fax: 612-625-5620
E-mail: elwir001@umn.edu
Received date: August 11, 2015 Accepted date:August 31, 2015Published date: September 07, 2015
Citation: Elwir S, Martin CM, Chinnakotla S, Reding M, Lake J, et al. (2015) Liver Transplantation for High Output Heart Failure Secondary to HHT: A Case Report and Review of the Literature. J Gastrointest Dig Syst 5:331. doi:10.4172/2161-069X.1000331
Copyright: © 2015 Elwir S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Liver involvement in hereditary hemorrhagic telangiectasia (HHT) can lead to high output heart failure. We report a case of a patient with HHT who developed high output heart failure that failed to respond to maximal medical therapy who eventually underwent liver transplantation with resolution of symptoms.
Keywords
Hereditary hemorrhagic telangiectasia; Heart failure; Liver transplantation
Abbreviations
HHT: Hereditary Hemorrhagic Telangiectasia; AVM: Arteriovenous Malformations; RA: Right Atrium; PA: Pulmonary Pressure; PCWP: Pulmonary Capillary Wedge Pressure; CO: Cardiac Output; CI: Cardiac Index; NA: Not Available
Introduction
Hereditary hemorrhagic telangiectasia (HHT) (also known as Osler-Weber-Rendu syndrome) is an autosomal dominant disease characterized by the presence of angiodysplastic lesions (telangiectasias and arteriovenous malformations (AVM)) that affect many organs [1,2]. These lesions can affect the skin, nasal cavity, gastrointestinal tract, liver, lung and brain [2,3]. Symptoms depend on the location and extent of lesions with the most common presenting symptoms including epistaxis and gastrointestinal bleeding [2].
A definite diagnosis is made when three of the following criteria is met: presence of telangiectasias; epistaxis; visceral lesions and a firstdegree relative with HHT [2,4]. Liver involvement can lead to high output heart failure, portal hypertension and biliary tract disease [1,5]. We report a case of a patient with HHT who developed high output heart failure that failed to respond to maximal medical therapy who eventually underwent liver transplantation with resolution of symptoms.
Case Report
A 54-year-old female patient with a past medical history of HHT was evaluated for progressive heart failure symptoms. The patient developed symptoms of shortness of breath and fluid overload at the age of 52. Hemodynamic evaluation noted the presence of high output heart failure and evidence of an A-V shunt in the liver (Table 1).
| Time of Right Heart Catheterization | Mean RA Pressure | PA Pressure (mean) | PCWP (mean) | Fick CO/CI: | Difference in Oxygen Saturation Post and Pre Liver (Hepatic O2 step-up) |
|---|---|---|---|---|---|
| At Presentation | 27 | 67/33 (47) | 29 | 8.65/3.87 | 4% |
| After aggressive diuresis and medical management | 26 | 58/33 (44) | NA | 7.96/3.44 | NA |
| After two embolization procedures | 26 | 60/32 (46) | 30 | 10.9/4.9 | 7% |
| 3 Months later | 23 | 55/28 (38) | 24 | 10/4.5 | 20% |
| After first cycle of Bevacizumab | 15 | 50/28 (36) | 22 | 7.5/3.4 | 2% |
| 4 Months later | 21 | 57/24(35) | 25 | 10.7/4.9 | 12% |
Table 1: Summary of hemodynamic evaluation results through the course of treatment. Abbreviations: RA: Right Atrium; PA: Pulmonary Pressure; PCWP: Pulmonary Capillary Wedge Pressure; CO: Cardiac Output; CI: Cardiac Index; NA: Not Available.
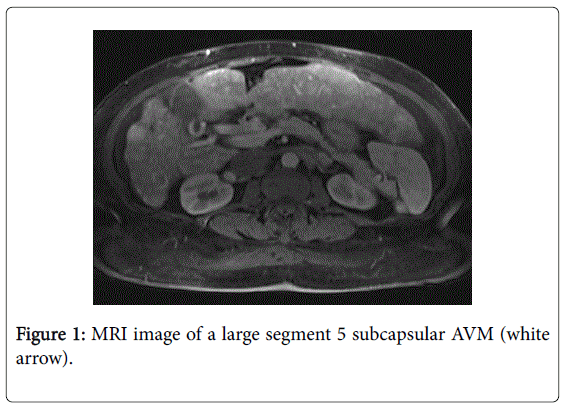
Further evaluation noted a large burden of hepatic AVMs (Figure 1). She underwent intensive medical management for her heart failure as well as three sessions of AVM embolization. She had only transient improvement in her heart failure symptoms after each treatment. She was subsequently treated with bevacizumab, an angiogenesis inhibitor, with an improvement of her hemodynamic status and resolution of the hepatic gradient (difference in oxygen saturation in the inferior vena cava post and pre liver). A few months later, her diuretic requirements increased again and repeat hemodynamic evaluation noted redemonstration of the hepatic gradient. She underwent another cycle of therapy with bevacizumab.
However, due to recurrent symptoms despite the use of bevacizumab and intensive medical therapy, liver transplant was offered to be the only option that would offer her long-term resolution of symptoms. She was evaluated for liver transplantation and was listed. An appeal was made to the regional review board and she was granted MELD exception points. She subsequently underwent deceased donor liver transplant (Figure 2). She tolerated the procedure well and her post-operative course was uneventful. By two months post-transplant, all of her cardiac symptoms had resolved and diuretics were stopped.
Discussion
Liver involvement occurs in up to 78% of the patients with HHT when evaluated by various imaging studies. However only 8% of such patients are symptomatic [6]. Liver involvement is characterized by diffuse vascular malformations throughout the liver that result in multiple types of shunting: hepatic artery to hepatic vein, hepatic artery to portal vein, and portal vein to hepatic vein [5,7]. Hepatic artery-to-hepatic-vein shunting is usually the predominant type. Patients can present as high output cardiac failure, portal hypertension and/or biliary tract disease. These types of complications can occur successively or concurrently [7,8].
The biliary tree obtains its blood supply from the peribiliary plexus that arises from the hepatic artery. Arteriovenous shunts may cause hypoperfusion of the peribiliary plexus and ischemic necrosis of extrahepatic or intrahepatic bile ducts, or both, with the subsequent development of biliary strictures [1]. On rare occasions, ischemic biliary necrosis may occur and affect large segments of the liver [9]. Portal hypertension results when shunting between the hepatic artery and portal vein occurs [1]. Portal hypertension may also develop secondary to nodular regenerative hyperplasia. Focal nodular hyperplasia can also develop [3].
High output cardiac failure is the most common clinical presentation in patients with hepatic involvement [5,8,10]. Shunting of blood from the hepatic artery to the hepatic vein results in a hyperdynamic circulation and leads to high output heart failure [4,7,8,11]. Therapeutic approaches toward symptomatic intrahepatic shunts depends on type of shunt and associated symptoms [1,7]. Patients with heart failure are initially treated with conventional medical therapy such as diuretics and beta blockers [7]. In the past, ligation of the hepatic artery or shunt embolization was attempted [1,5,8,10]. Although amelioration or resolution of symptoms has been reported in most of the cases, this effect is generally only transient and treatment maybe associated with significant morbidity and mortality, mostly in the form of biliary and/or hepatic necrosis [8,10]. In the largest case series by Chavan et al, 20 patients with HHT underwent staged embolization of the hepatic artery. Ischemic cholecystitis and cholangitis were observed in four patients (20%). Focal areas of hepatic necrosis were noted in three of these four patients with multiple biliary abscesses and biliary sepsis in one of them [12]. An expert panel recommended that hepatic artery embolization be avoided in patients with liver AVMs as it is only a temporizing procedure, and is associated with significant morbidity and even mortality [4].
Recently bevacizumab, an anti–vascular endothelial growth factor (VEGF) monoclonal antibody, has been used in the treatment of HHT [13]. Treatment with bevacizumab was associated with a decrease in cardiac output and reduced duration and number of episodes of epistaxis [13]. Bevacizumab was also used in HHT patients with ischemic cholangiopathy with imaging evidence of improvement in the biliary disease and clinically, it obviated need for liver transplantation [14].
Liver transplantation is a treatment option in patients with HHT [4,15]. Indications for transplant include biliary necrosis and\or heart failure not responding to conventional therapy [4]. In the United States, patients with HHT may be eligible for MELD exception points if they have evidence intractable heart failure or if they develop bile duct necrosis [16].
The outcomes after liver transplant are good with the actuarial 1-, 5-, and 10-year patient and graft survival rates being 82.5% in the largest case series, 40 patients, from the European Liver Transplant Registry [15]. In a study by Boillot et al. the hyperdynamic circulation disappeared after liver transplantation in all patients studied. At time of last follow-up, all patients were asymptomatic and had normal computed tomography of the liver and right heart catheterization 6 months after transplant [17].
The disease can reoccur after transplant. In the series of Lerut et al, two first cousin females, transplanted for mixed cardiac and biliary HHT disease, presented with focal vascular dilatations throughout the allograft at 156 and 84 months post-liver transplant [15].
Our patient initially presented with heart failure that failed to respond to conventional medical therapy. She also failed to obtain a sustained response to AVM embolization and bevacizumab, leaving transplantation as the only viable option. Liver transplantation resulted in an improvement in the symptoms of heart failure as early as two months after transplant.
Patients with HHT benefit from a multidisciplinary approach to their care. Physicians treating patients with HHT should consider referring patients with HHT and intractable heart failure for a liver transplant evaluation.
References
- Garcia-Tsao G, Korzenik JR, Young L, Henderson KJ, Jain D, et al. (2000) Liver disease in patients with hereditary hemorrhagic telangiectasia. N Engl J Med 343: 931-936.
- McDonald J, Wooderchak-Donahue W, VanSant Webb C, Whitehead K, Stevenson DA5, et al. (2015) Hereditary hemorrhagic telangiectasia: genetics and molecular diagnostics in a new era. Front Genet 6: 1.
- Brenard R, Chapaux X, Deltenre P (2010) Large spectrum of liver vascular lesions including high prevalence of focal nodular hyperplasia in patients with hereditary haemorrhagic telangiectasia: the Belgian Registry based on 30 patients. Eur J GastroenterolHepatol 22: 1253-1259.
- Faughnan ME, Palda VA, Garcia-Tsao G, Geisthoff UW, McDonald J, et al. (2011) International guidelines for the diagnosis and management of hereditary haemorrhagic telangiectasia. J Med Genet 48: 73-87.
- Sabbà C, Pompili M (2008) Review article: the hepatic manifestations of hereditary haemorrhagic telangiectasia. Aliment PharmacolTher 28: 523-533.
- Ianora AA, Memeo M, Sabba C, Cirulli A, Rotondo A, et al. (2004) Hereditary hemorrhagic telangiectasia: multi-detector row helical CT assessment of hepatic involvement. Radiology 230: 250-259.
- Dupuis-Girod S, Chesnais AL, Ginon I (2010) Long-term outcome of patients with hereditary hemorrhagic telangiectasia and severe hepatic involvement after orthotopic liver transplantation: a single-center study. Liver Transpl 16: 340-347.
- Garcia-Tsao G (2007) Liver involvement in hereditary hemorrhagic telangiectasia (HHT). J Hepatol 46: 499-507.
- Bauer T, Britton P, Lomas D, Wight DG, Friend PJ, et al. (1995) Liver transplantation for hepatic arteriovenous malformation in hereditary haemorrhagic telangiectasia. J Hepatol 22: 586-590.
- Thevenot T, Vanlemmens C, Di Martino V, Becker MC, Denue PO, et al. (2005) Liver transplantation for cardiac failure in patients with hereditary hemorrhagic telangiectasia. Liver Transpl 11: 834-838.
- Ginon I, Decullier E, Finet G, Cordier JF, Marion D, et al. (2013) Hereditary hemorrhagic telangiectasia, liver vascular malformations and cardiac consequences. Eur J Intern Med 24: e35-39.
- Chavan A, Luthe L, Gebel M, Barg-Hock H, Seifert H, et al. (2013) Complications and clinical outcome of hepatic artery embolisation in patients with hereditary haemorrhagic telangiectasia. EurRadiol 23: 951-957.
- Dupuis-Girod S, Ginon I, Saurin JC, Marion D, Guillot E, et al. (2012) Bevacizumab in patients with hereditary hemorrhagic telangiectasia and severe hepatic vascular malformations and high cardiac output. JAMA 307: 948-955.
- Vlachou PA, Colak E, Koculym A (2013) Improvement of ischemic cholangiopathy in three patients with hereditary hemorrhagic telangiectasia following treatment with bevacizumab. J Hepatol 59: 186-189.
- Lerut J, Orlando G, Adam R, Sabbà C, Pfitzmann R, et al. (2006) Liver transplantation for hereditary hemorrhagic telangiectasia: Report of the European liver transplant registry. Ann Surg 244: 854-862.
- Garcia-Tsao G, Gish RG, Punch J (2006) Model for end-stage liver disease (MELD) exception for hereditary hemorrhagic telangiectasia. Liver Transpl 12: S108-109.
- Boillot O, Bianco F, Viale JP (1999) Liver transplantation resolves the hyperdynamic circulation in hereditary hemorrhagic telangiectasia with hepatic involvement. Gastroenterology 116: 187-192.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 15822
- [From(publication date):
October-2015 - Jul 02, 2025] - Breakdown by view type
- HTML page views : 11200
- PDF downloads : 4622