Lithium in the Normal Therapeutic Range: A Potential Sneaky Danger for the Brain. A Case of Slow Tricking Neurotoxicity and a Brief Overview of Literature
Received: 29-Nov-2017 / Accepted Date: 13-Dec-2017 / Published Date: 20-Dec-2017 DOI: 10.4172/2161-0460.1000407
Abstract
In medicine, Lithium salts are known to be useful as a mood-stabilizing drug in the treatment of bipolar disorder and depression. In neurology Lithium is used as prophylaxis of cluster headache. Lithium may induce intoxication with renal failure, thyroid dysfunction, cardiac arrhythmias and neurotoxicity. Toxicity signs are associated with increased serum concentrations (>1.2 mEq/l); however, there have been some reports of neurotoxicity also with therapeutic drug levels. We describe the case of a 70 years old woman who was assuming Lithium for a bipolar disorder with a permanent control of psychiatric symptoms. After 40 years of continued therapy with lithium she developed a rapidly progressive dementia with multifocal brain signs, although lithium serum levels were always normal. She was carefully investigated with regard to the cognitive decline and all possible primary and secondary rapidly progressive dementia were excluded. When the clinical state was quite terminal, all therapies were interrupted and she progressively recovered after withdrawal of lithium therapy.
Keywords: Lithium; Neurotoxicity; Dementia
Introduction
In nature, Lithium is a metal, the lightest metal and the lightest solid element. In biological systems, lithium is present only in trace and the large part of its functions is still unclear. By a pharmacological point of view, Lithium is an orphan drug commonly used in psychiatry as mood-stabilizer and in neurology as prophylaxis of cluster headache. Lithium is assimilated by gastrointestinal tract and largely eliminated by the renal way.
Both systemic and neurological toxicity of lithium is well known. Toxicity during prolonged treatment with lithium is generally labelled as chronic intoxication and generally it results from a progressive lithium accumulation that may be due to renal failure, low sodium intake and/ or reciprocal drug interactions. In these cases, lithium concentration progressively increases reaching toxic levels. In rare cases, lithium toxicity was observed in patients with normal serum concentrations and in these cases the lithium toxicity was labelled as lithium super sensitivity.
Early in the treatment, lithium may cause tremor and this kind of acute intoxication may cause renal failure, thyroid dysfunction, cardiac arrhythmias and, as far as neurotoxicity is concerned, tremor, drowsiness, nystagmus, confusion, ataxia, extrapyramidal symptoms, stuttering [1,2] and even chronic cerebellar atrophy [3]. In the most severe forms of intoxication, seizure, coma and death can occur [4]. Some cases with rapid onset dementia mimicking Creutzfeldt-Jakob disease (CJD) disease both from a clinical and EEG point of view have also been described [5,6]. For these reasons, lithium serum levels must be checked every 3-6 months. In most cases, toxicity signs are associated with serum concentration greater than 1.2 mEq/l; however, there have been some reports of paradoxical neurotoxicity even in the therapeutic range (≤ 1 mEq/l) [7]. A few reports of non-progressive cogwheel rigidity associated with chronic treatment with normal serum levels have also appeared in literature [8]. In these slow-evolving situations, lithiumrelated neuropsychiatric symptoms are difficult to be differentiated from other disorders. Additionally, these situations are more frequent among elderly, which are particularly vulnerable to chronic intoxication.
Furthermore, the use of lithium may increase the prevalence or severity of pre-existing or age-dependent neurological conditions, that are obviously more frequent in old patients. A series of hypothesis have been formulated to explain this lithium toxicity in a nontoxic concentration range: First of all, serum concentrations are not strictly proportional to brain concentrations and it was shown that lithium accumulates in the brain, especially with chronic treatment [9]. Moreover, this cerebral accumulation is not homogeneous with increased uptake in the white matter, the pons and the brainstem. This non uniform accumulation of lithium in some areas of the brain could induce focal toxicity despite therapeutic serum levels.
Longitudinally it may result in territories of high lithiumconcentration that induce neurotoxicity [10]. The consequence of these evidences is that when there is the doubt of lithium-induced toxicity in a lithium treated patient, even in therapeutic range, repeated clinical examinations and serial EEGs are required and a discontinuation in lithium treatment is mandatory to exclude its role in that specific case [11].
Case Report
Lucia is a 74 years old woman with hypothyroidism, hypertension, hypercholesterolemia, diabetes and long standing recurrent Major Depression treated with lithium (the drug was started 40 years before she came to our observation). Familial history is negative for neurologic diseases. In 2006, she began to complain of intentional tremor, for which a trial of suspension of lithium therapy was tried. However, due to the rapid recurrence of depression, lithium was restarted. The psychiatrist advised against stopping lithium again. In 2008, she began to complain of diplopia, memory deficits, anomia, disorientation, apathy and recurrence of depression. In January 2009, the patient underwent a neurological examination: Diplopia had spontaneously subsided but all other symptoms persisted. Lucia exhibited gross postural tremor, hyperkinetic reflexes and rigidity. MMSE was 18/30. At that time, Lucia had stopped for a few weeks an antidopaminergic drug (amisulpride) previously prescribed by her psychiatrist and had begun citalopram and propranolol for tremor. Serial neurological examinations showed relative stability of cognitive impairment but worsening of extrapyramidal signs with bradikinesia, shuffling gait, frequent falls and significant axial and limb rigidity. A trial of dopaminergic drugs (L-Dopa/benserazide and rotigotine) was not beneficial. MRI of March 2010 showed general atrophy and some bilateral lacunae in subependimal and periventricular white matter.
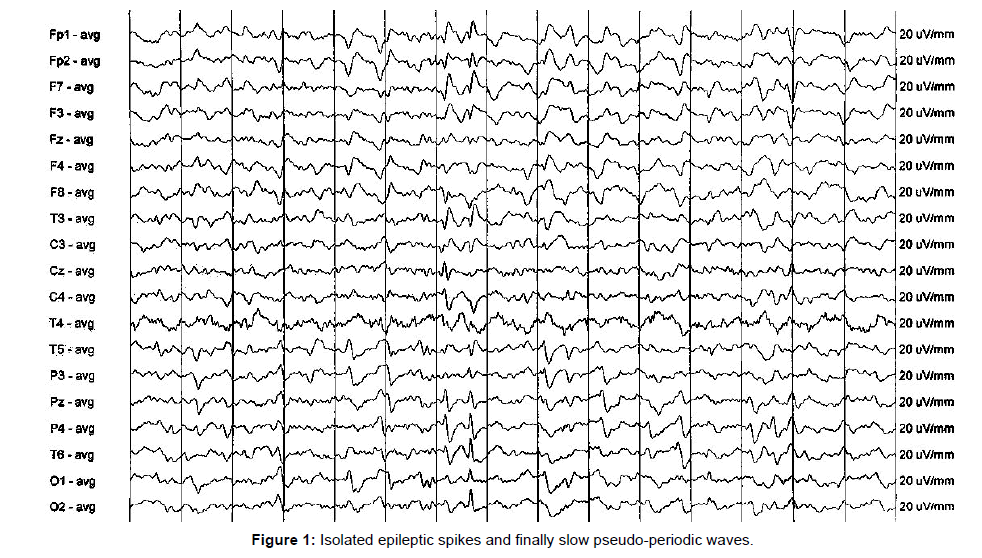
Due to progressive worsening, in October 2010 Lucia was hospitalised. She exhibited working memory and long term memory deficits, reasoning and comprehension impairment, slight impairment of upper gaze excursion, dysarthria and dysphagia, amimia, anosmia, left hand ideomotor apraxia. She also showed bilateral grasping, agraphestesia, postural-intentional tremor, dysmetria and cog-wheel rigidity at all four limbs: All these signs were more pronounced on the left side. Static and dynamic ataxia and bradikinesia were also present. She couldn’t localize tactile and pain stimuli on the left. Sense of motion was spared only at the right foot. Neuropsychological tests showed multiple deficits (memory, executive functions, ideomotor and constructive praxis, closing-in, verbal and written language, calculus). Again, the praxis deficits were prevalent on the left. At the beginning of hospitalization, Lucia was taking lithium 300 mg bid, along with several other drugs (citalopram, levothyroxine, glimepiride, metformin, propranolol, acetylsalicilyc acid, rotigotine, atorvastatin, omeprazole). Lithium serum level was within the normal range at 1.05 mEq/l. Vitamin B12, folic acid, thyroid hormones and neoplastic markers levels were normal. A diagnosis of Corticobasal Degeneration (CBD) was hypothesized. During hospitalization, in absence of any therapeutic change, rapid worsening with marked clinical fluctuations and occasional arm jerks were evident. A first EEG showed severe slowing, isolated epileptic spikes and non-periodical triphasic waves. A second EEG (one week after) showed slow pseudo-periodic waves and posterior sharp waves slightly increased by intermittent photic stimulation. At that point, possible CJD or paraneoplastic encephalitis (there have been a finding of fecal occult blood just before hospitalization) were hypothesized. Levetiracetam 500 mg bid was started and hospitalization in an acute neurological ward was requested for further investigations. During this hospitalization, Lucia underwent a second MRI, which was unchanged; an abdomen and thorax CT scan (negative for neoplasms) and longitudinal EEG evaluation, which showed a progressive diffuse slowing of electric activity with periodic bursts. An antibody screening for vasculitis, autoimmune thyroiditis and paraneoplastic syndromes was negative. CSF examination showed mildly increased proteins (574 mg/dL, range 150-450). 14.3.3 Protein search in CSF and genetic screening for PRNP mutations were negative. While staying in the acute neurological ward Lucia further worsened till definitely bedridden. She also developed severe oro-lingual apraxia and opposition to taking food, thus requiring PEG positioning. Fluctuations of mood from apathy to agitation was present, therefore quetiapine was started. The patient was then transferred to a psychiatric rehabilitation ward at the beginning of February 2011. When she was there, she suffered for persistent hypoglicemia and acute renal failure and was transferred in an acute nephrology ward were she was submitted to one hemodialitic session. At that time, Lucia was described as uncooperative, almost unresponsive, with lower extremities obliged flexion and reduction of motility at the left arm. The acute renal failure was attributed to lithium and metformine; oral treatment for diabetes was replaced by insulin therapy; lithium, however, was maintained. At the end of February 2011, she was transferred to a rehabilitation ward where she was described as severely demented (MMSE: Impossible; Clinical Dementia Rating: 4) and then in a long term facility in April 2011. She was considered to be in terminal condition and all drugs were stopped. Her motor and cognitive condition rapidly improved and in July 2011 PEG was removed and repeated MMSE was 22/30. She then restarted rehabilitation and for the subsequent two years she showed a progressive improvement. At a clinical examination performed at the end of 2013 Lucia was fully cooperative and aware of her clinical history, she could walk with aid, extrapyramidal signs were greatly reduced (only mild bradikinesia, mild postural tremor in the upper limbs, a modest asymmetric rigidity and motor impairment in left hand movement persisted) and MMSE was 24/30. Sensory examination was normal. A neuropsychological test battery administered at the end of 2012 still showed multiple cognitive deficits, but greatly reduced compared with the evaluation performed in October 2010. Actual medications included levothyroxin, insuline, omeprazole, calcium, vitamin D, alendronate, clonazepam and pregabalin. Quetiapine had been stopped 6 months before. Lucia and his husband are obviously very exhausted by the long recent clinical history and they preferred to avoid further medical investigations if not strictly necessary. As of October 2014, her neurological conditions, including MMSE, are stable.
Discussion
Neurotoxicity of lithium is well-known, both acute and chronic; notwithstanding, the case here presented seems to be remarkable for several aspects. Only in a few cases lithium toxicity really mimic dementia and generally these cases have the clinical pattern of a rapidly progressive cognitive decline that develop in a few months [6]. On the contrary, as widely described in the case, in our patient, cognitive deficits had begun a long time before the subacute worsening (October 2010), perfectly mimicking a primary neurodegenerative disorder. Additionally, at a certain point of her story, Lucia showed an asymmetric rigid Parkinsonism associated with apraxia and agraphestesia suggestive of CBD. The discontinuation of lithium therapy was fortuitous and it happened when the cognitive and functional condition of this patient was completely compromised. Notwithstanding this accidental and extremely late removal of the toxic agent, the clinical condition reverted in a more or less complete way.
Even if some neuropsychological impairment was still present in 2013, the cognitive status of Lucia was far better than in January 2009 and the term “dementia” could no longer be applied to that condition (the residual functional handicap was principally due to the residual motor deficits). After stopping lithium, also apraxia and agraphestesia subsided and extrapyramidal signs largely regressed.
Even if we cannot exclude a subjacent neurodegenerative disorder, the improvement and then long-term stability of residual extrapyramidal signs suggest that they could be iatrogenic, too (due to long term lithium therapy associated with neuroleptic drugs in the past). Chronic lithium toxicity has been associated with rigidity development [12]. Performing a DAT scan would be possibly useful for a differential diagnosis, but the patient preferred to delay unessential medical investigations. Another point to be underlined is the fact that in this case, differently than in others [6]. lithium was always in the normal range. According to literature, lithium can be toxic even in the normal range, particularly, as in this case, for elderly people with comorbidities receiving polypharmacy, e.g. antidepressants [13]. It is worth of notice the fact the Lucia’s rapid worsening occurred in absence of recent therapy changes (she had been taking citalopram for at least one year). Other stabilizing therapies can replace lithium. In our case, Major Depression did not come back after lithium withdrawal and the patient’s mood remained stable on low doses of quetiapine, afterwards replaced by low doses of pregabalin. Another lesson to take from this case is the fact that sub-acute lithium toxicity can develop even after decades of therapy. In fact, in our patient signs of chronic toxicity were present since a long time (hypothyroidism with negative thyroid auto-antibodies, rigidity and tremor) and they should have been taken into account by clinicians from the beginning. In the sub-acute phase, the patient not only exhibited neurological deterioration, but she also developed acute renal failure (another possible side effect of lithium therapy that in turn reduces lithium clearance). However, even after this episode, clinicians failed to stop the harmful drug. A possible clue to detect lithium neurotoxicity could be EEG: Lithium can cause different EEG patterns: Slowed basic rhythm, theta waves bursts, intermittent local sharp waves or spikes, spike-and-slow-wave complexes and even periodic sharp waves with or without myoclonic jerks. Lithium intoxication can mimic both the clinical and EEG pattern of CJD [14]. In one case, an EEG pattern mimicking CJD was associated with rapid onset of coma [4]. Our patient showed almost all possible EEG signs due to lithium intoxication: Severe slowing of basic rhythm, isolated epileptic spikes and finally slow pseudo-periodic waves (Figure 1), but it is to note that also these EEG findings are not specific of lithium toxicity and they are seen in wide spectrum of cerebral pathological conditions.
Neurotoxicity of lithium is well-known, both acute and chronic; notwithstanding, the case here presented seems to be remarkable for several aspects. Only in a few cases lithium toxicity really mimic dementia and generally these cases have the clinical pattern of a rapidly progressive cognitive decline that develop in a few months [6]. On the contrary, as widely described in the case, in our patient, cognitive deficits had begun a long time before the subacute worsening (October 2010), perfectly mimicking a primary neurodegenerative disorder. Additionally, at a certain point of her story, Lucia showed an asymmetric rigid Parkinsonism associated with apraxia and agraphestesia suggestive of CBD. The discontinuation of lithium therapy was fortuitous and it happened when the cognitive and functional condition of this patient was completely compromised. Notwithstanding this accidental and extremely late removal of the toxic agent, the clinical condition reverted in a more or less complete way.
Even if some neuropsychological impairment was still present in 2013, the cognitive status of Lucia was far better than in January 2009 and the term “dementia” could no longer be applied to that condition (the residual functional handicap was principally due to the residual motor deficits). After stopping lithium, also apraxia and agraphestesia subsided and extrapyramidal signs largely regressed.
Even if we cannot exclude a subjacent neurodegenerative disorder, the improvement and then long-term stability of residual extrapyramidal signs suggest that they could be iatrogenic, too (due to long term lithium therapy associated with neuroleptic drugs in the past). Chronic lithium toxicity has been associated with rigidity development [12]. Performing a DAT scan would be possibly useful for a differential diagnosis, but the patient preferred to delay unessential medical investigations. Another point to be underlined is the fact that in this case, differently than in others [6]. lithium was always in the normal range. According to literature, lithium can be toxic even in the normal range, particularly, as in this case, for elderly people with comorbidities receiving polypharmacy, e.g. antidepressants [13]. It is worth of notice the fact the Lucia’s rapid worsening occurred in absence of recent therapy changes (she had been taking citalopram for at least one year). Other stabilizing therapies can replace lithium. In our case, Major Depression did not come back after lithium withdrawal and the patient’s mood remained stable on low doses of quetiapine, afterwards replaced by low doses of pregabalin. Another lesson to take from this case is the fact that sub-acute lithium toxicity can develop even after decades of therapy. In fact, in our patient signs of chronic toxicity were present since a long time (hypothyroidism with negative thyroid auto-antibodies, rigidity and tremor) and they should have been taken into account by clinicians from the beginning. In the sub-acute phase, the patient not only exhibited neurological deterioration, but she also developed acute renal failure (another possible side effect of lithium therapy that in turn reduces lithium clearance). However, even after this episode, clinicians failed to stop the harmful drug. A possible clue to detect lithium neurotoxicity could be EEG: Lithium can cause different EEG patterns: Slowed basic rhythm, theta waves bursts, intermittent local sharp waves or spikes, spike-and-slow-wave complexes and even periodic sharp waves with or without myoclonic jerks. Lithium intoxication can mimic both the clinical and EEG pattern of CJD [14]. In one case, an EEG pattern mimicking CJD was associated with rapid onset of coma [4]. Our patient showed almost all possible EEG signs due to lithium intoxication: Severe slowing of basic rhythm, isolated epileptic spikes and finally slow pseudo-periodic waves (Figure 1), but it is to note that also these EEG findings are not specific of lithium toxicity and they are seen in wide spectrum of cerebral pathological conditions.
Conclusion
This case remembers again to clinicians that iatrogenic causes must always be taken into account in the case of more or less rapidly progressive dementia and/or motor deterioration and/or vigilance fluctuations. In all these situations, when the patient is assuming possibly cognitively harmful drugs, they must be stopped, at least for a certain period, even against contrary psychiatric advice. In this case, improvement after stopping lithium was remarkable but incomplete and the consequences of severe osteoporosis due to prolonged bed staying did not disappear.
As previously underlined, in line with other similar reports, when there is the doubt of lithium-induced toxicity in a lithium treated patient, even in therapeutic range, repeated clinical careful examinations and serial EEGs are mandatory and a discontinuation in lithium treatment is required to exclude its toxic role.
References
- Dunne FJ (2010) Lithium toxicity: The importance of clinical signs. Br J Hosp Med (Lond) 71: 206-210.
- Sabillo S, Samala RV, Ciocon JO (2012) A stuttering discovery of lithium toxicity. J Am Med Dir Assoc 13: 660-661.
- Rossi FH, Rossi EM, Hoffmann M, Liu W, Cruz RR, et al. (2017) Permanent cerebellar degeneration after acute hyperthermia with non-toxic lithium levels: A case report and review of literature. Cerebellum 16: 973-978.
- Suda M, Kubota F, Aihara Y, Hiraoka T, Aoyama Y, et al. (2009) A case of lithium intoxication with periodic sharp waves. Pharmacopsychiatry 42: 122-123.
- Mouldi S, Le Rhun E, Gautier S, Devemy M, Deste ´e A, et al. (2006) Lithium-induced encephalopathy mimicking Creutzfeldt-Jakob disease. Rev Neurol (Paris) 162: 1118-1121.
- Mignarri A, Chini E, Rufa A, Rocchi R, Federico A, et al. (2013) Lithium neurotoxicity mimicking rapidly progressive dementia. J Neurol 260: 1152-1154.
- Emilien G, Maloteaux JM (1996) Lithium neurotoxicity at low therapeutic doses. Hypotheses for causes and mechanism of action following a retrospective analysis of published case reports. Acta Neurol Belg 96: 281-293.
- Johnels B, Wallin L, WÃ¥linder J (1976) Extrapyramidal side effects of lithium treatment. Br Med J 2: 642.
- Hillert M, Zimmermann M, Klein J (2012) Uptake of lithium into rat brain after acute and chronic administration. Neurosci Lett 521: 62-66.
- Kemperman CJ, Gerdes JH, De Rooij J, Vencken LM (1989) Reversible lithium neurotoxicity at normal serum level may refer to intracranial pathology. J Neurol Neurosurg Psychiatry 52: 679-680.
- Peng J (2014) Case report on lithium intoxication with normal lithium levels. Shanghai Arch Psychiatry 26: 103-104.
- Shopsin B, Gershon S (1975) Cogwheel rigidity related to lithium maintenance. Am J Psychiatry 132: 536-538.
- West AP, Meltzer HY (1979) Paradoxical lithium neurotoxicity: A report of five cases and a hypothesis about risk for neurotoxicity. Am J Psychiatry 136: 963-966.
- Smith SJ, Kocen RS (1988) A Creutzfeldt-Jakob like syndrome due to lithium toxicity. J Neurol Neurosurg Psychiatry 51: 120-123.
Citation: Farina E, Giani L, Lovati C, Mariani C, Nemni R (2017) Lithium in the Normal Therapeutic Range: A Potential Sneaky Danger for the Brain. A Case of Slow Tricking Neurotoxicity and a Brief Overview of Literature. J Alzheimers Dis Parkinsonism 7: 407. DOI: 10.4172/2161-0460.1000407
Copyright: © 2017 Farina E, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 5932
- [From(publication date): 0-2017 - Apr 02, 2025]
- Breakdown by view type
- HTML page views: 5055
- PDF downloads: 877