Image Open Access
Lipoma of the Pancreas Diagnosed by EUS-FNA
Kosuke Minaga1,2*, Yukitaka Yamashita1 and Yoshito Uenoyama1
1Department of Gastroenterology and Hepatology, Japanese Red Cross Society Wakayama Medical Center, Wakayama, Japan
2Department of Gastroenterology and Hepatology, Kinki University Faculty of Medicine, Osaka-sayama, Japan
- *Corresponding Author:
- Kosuke Minaga
Department of Gastroenterology and Hepatology
Kinki University Faculty of Medicine, Osaka-sayama
377-2 Ohno-Higashi, Osaka-Sayama 589-8511, Japan
Tel: +81-72-3660221
Fax: +81-72-3672880
E-mail: kousukeminaga@med.kindai.ac.jp
Received date: May 14, 2015; Accepted date: May 15, 2015; Published date: May 21, 2015
Citation: Minaga K, Yamashita Y, Uenoyama Y (2015) Lipoma of the Pancreas Diagnosed by EUS-FNA. J Gastrointest Dig Syst 5:i105. doi: 10.4172/2161-069X.1000i105
Copyright: © 2015 Minaga K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Keywords
Lipoma of the pancreas; Endoscopic ultrasound-guided fine-needle aspiration; Pancreatic mesenchymal tumor
Clinical Image
Pancreatic mesenchymal tumors are infrequent and account for approximately 1-2 % of all pancreatic tumors [1]. Lipoma of the pancreas is a particularly rare condition, and only 50 cases have been described since the first case report by Bigard et al. in 1989 [2]. Recently, endoscopic ultrasound-guided fine-needle aspiration (EUSFNA) has gained wide acceptance as a safe and well established examination technique for the diagnosis of pancreatic masses. However, only three cases of pancreatic lipoma diagnosed by EUSFNA have been described to date in the literature [3-5]. Herein, we report a case of pancreatic tail lipoma diagnosed by EUS-FNA. A 72- year-old man with an incidental pancreatic mass that was detected by computed tomography (CT) was referred to our hospital.
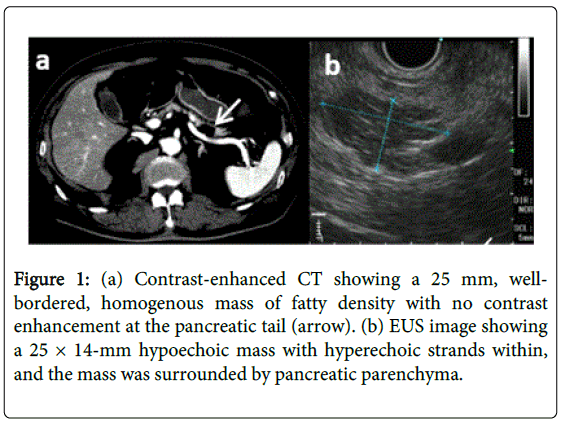
The CT scan demonstrated a well-bordered, homogenous mass of fatty density with no contrast enhancement at the pancreatic tail (Figure 1a). On magnetic resonance imaging, the lesion had highintensity signals on both T1-weighted and T2-weighted axial sequences. Subsequently, EUS was performed to clarify the etiology of the mass using a curved linear array echoendoscope (GF-UCT260; Olympus, Tokyo, Japan). EUS revealed a 25 × 14-mm hypoechoic mass with hyperechoic strands within, and the mass was surrounded by pancreatic parenchyma (Figure 1b).
To exclude malignant tumors such as liposarcoma and lipoblastoma, we performed EUS-FNA by a transgastric approach using a 22-G needle (Expect; Boston Scientific Corporation, Natick, MA, USA). Two passes were made with suction with no postprocedural complications.
Microscopic examination of the EUS-FNA material showed mature adipose cells characterized by a large fat droplet with no atypia, and no malignant cells were identified (Figure 2a and 2b). Thus, we confirmed the diagnosis of a pancreatic lipoma. The patient was conservatively followed up without surgical resection. Follow-up CT, conducted 1 year later, showed no apparent change in size or characteristics of the lesion.
References
- Raut CP, Fernandez-del Castillo C (2003) Giant lipoma of the pancreas: case report and review of lipomatous lesions of the pancreas. Pancreas 26: 97-99.
- Bigard MA, Boissel P, Regent D, Froment N (1989) Intrapancreatic lipoma. First case in the literature. Gastroenterol Clin Biol 13: 505-507.
- Di Matteo FM, Shimpi L, Pandolfi M, Rabitti C, Fabio C, et al. (2006) EUS diagnosis of pancreatic lipoma: a case report. Gastrointest Endosc 64: 146-148.
- Suzuki R, Irisawa A, Hikichi T, Shibukawa G, Takagi T, et al. (2009) Pancreatic lipoma diagnosed using EUS-FNA. A case report. JOP 10: 200-203.
- Pausawasdi N, Apisarnthanarak P, Pongpaibul A, Charatcharoenwitthaya P (2012) Pancreatic lipoma diagnosed by EUS-FNA. Gastrointest Endosc 76: 668-669.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 14754
- [From(publication date):
June-2015 - Apr 05, 2025] - Breakdown by view type
- HTML page views : 10182
- PDF downloads : 4572