Lifetime Expectancy in Dementia with Lewy Bodies: Effects of Donepezil Administration and Special Nursing Home Replacement. A Retrospective Analysis in the Tajiri Project
Received: 13-Dec-2017 / Accepted Date: 09-Jan-2018 / Published Date: 16-Jan-2018 DOI: 10.4172/2161-0460.1000416
Abstract
Objective: Cholinesterase inhibitors (ChEIs) can delay the progression of Alzheimer disease (AD). We previously demonstrated a positive effect of donepezil (DNP) administration and a Special Nursing Home (SNH) replacement on lifetime expectancy after the onset of AD. Recently DNP has been indicated for use in the treatment of dementia with Lewy Bodies (DLB); however, the effect on lifetime expectancy remains unclear. Herein, we analyzed the effects of DNP on DLB.
Methods: All outpatients at the Tajiri Clinic with available medical records and death certificates from 1999- 2012 were included in this retrospective analysis. The entry criteria were a diagnosis of dementia based on DSM-IV criteria and diagnosis of DLB using the international consensus criteria; medical treatment for more than 3 months and follow up to less than 1 year before death.
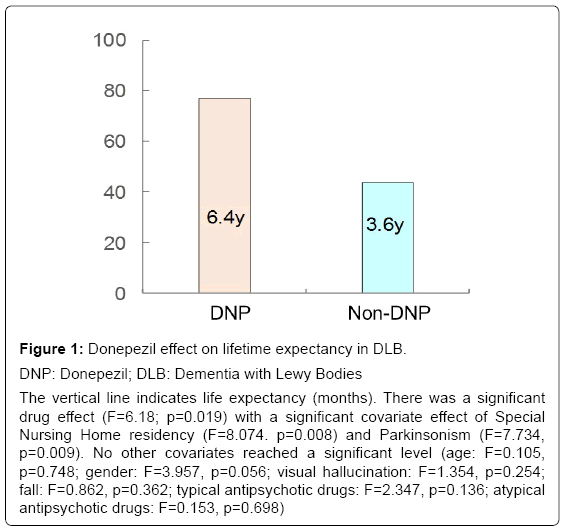
Results: We identified 510 subjects based upon medical records and death certificates, of which 360 had a diagnosis of dementia that met the entry criteria. Of 51 patients diagnosed with DLB, 23 had taken DNP and 28 patients had not undergone drug treatment due to treatment prior to the introduction of DNP in 1999 in Japan. The lifetime expectancies after onset were 6.4 years in the DNP group and 3.6 years in the non-DNP group; with a significant drug effect. However, in contrast with the previous AD data, no significant effect of SNH residency was noted.
Conclusion: Although this report has the limitation that all analyses were retrospective and lacked randomization, we found a positive effect of DNP on lifetime expectancy after the onset of DLB. The lower life expectancy compared with that of AD and the lack of an effect of SNH residency suggest the cholinergic deficiency in DLB is greater than that in AD.
Keywords: Dementia with lewy bodies (DLB); Lifetime expectancy; Donepezil
Abbreviations
AD: Alzheimer Disease; ChEIs: Cholinesterase Inhibitors; DLB: Dementia with Lewy Bodies; DNP: Donepezil; FTLD: Frontotemporal Lobar Degeneration; QOL: Quality of Life; SNH: Special Nursing Home
Introduction
Lifetime expectancy for patients with dementia, especially Alzheimer disease (AD) directly influences medical and care service needs and is a common question posed by families and patients. Brodaty et al. [1] compared mortality and survival in dementia with estimated lifetime expectancies in the general population. Survival after diagnosis of dementia varies considerably and depends on numerous factors and complex interactions among these factors. Relative loss of life expectancy decreases with age at diagnosis and also depends on gender, dementia subtype, and severity stage. A definitive meta-analysis of survival in dementia is precluded by deficiencies in primary studies.
Following AD and vascular dementia (VaD), dementia with Lewy Bodies (DLB) has been reported to be the third main cause of dementia [2]. At present, there are no curative drugs for AD or DLB; however, symptomatic drugs, such as cholinesterase inhibitors (ChEIs), e.g. 1 donepezil (DNP), may delay progression (not biological but symptomatic) of the disease. We previously reported that the visual hallucinations manifested by DLB patients were also improved by DNP [3]. This effect combined with psychosocial interventions such as reality orientation and/or reminiscence approach may increase the quality of life (QOL) of patients likely among AD patients [4]. Beyond delayed progression and increased QOL, the ultimate outcome of drug treatment should be measured in terms of lifetime expectancy.
For such a long-term effect, we previously demonstrated a positive effect of DNP administration and a Special Nursing Home (SNH) replacement on lifetime expectancy after the onset of AD (without DLB) [5]. This may be due to the decreased mortality rate caused by reduction of concomitant diseases such as pneumonia. In the SNH, they can receive sophisticated psychosocial interventions. For AD patients, the similar lifetime expectancies in patients taking DNP at home and those not taking DNP in the SNH indicated a positive health economic effect of the drug; however, the effect for DLB is unclear. Herein, using the same database (1999-2012) with additional database (2013-2017), we re-analyzed the effects of DNP administration and/or SNH replacement on lifetime expectancy in DLB.
Despite the retrospective design, this is the first long-term study of the possible effect of DNP on the lifetime expectancy of patients with DLB. We hypothesized that 1) the drug would exhibit a positive effect on lifetime expectancy, and 2) that SNH residency would also exhibit a positive effect. We analyzed DNP alone, because this drug has been used since 1999 in Japan; whereas other drugs, such as galantamine or memantine, have only been used since 2011, thus preventing us from obtaining long-term data. The combined effect of DNP and SNH residency was also analyzed.
Methods
Subjects
All outpatients from their own homes or the SNH at the Tajiri Clinic from 1999-2017 with available medical records and death certificates were included in this retrospective analysis. The entry criteria were a diagnosis of dementia based on DSM-IV criteria and diagnosis of DLB using the international consensus criteria; medical treatment for more than 3 months; and follow up until less than 1 year before death.
Dementia diagnosis
As described previously [5,6], diagnoses of the dementing diseases were determined during a meeting of two neurologists, a psychiatrist, and a geriatrician. Briefly, AD and VaD were diagnosed according to the NINCDS-ADRDA and the NINDS-AIREN criteria, respectively [7,8]. Dementia with Lewy bodies (DLB) and frontotemporal lobar degeneration (FTLD) were diagnosed based on the respective consensus criteria [9,10]. Other conditions were diagnosed in 20 patients, as described previously [5,6].
Written informed consent was obtained from each patient and from the family of those with dementia at entry according to the Declaration of Helsinki (1991). The study was approved by the ethical committee of Tohoku University Graduate School of Medicine, as well as that of the Osaki-Tajiri SKIP Center.
Analyses
The main outcome was lifetime expectancy (i.e., the number of months between the onset of dementia and death). One-way ANOVA, along with the covariance of age and sex, included the effects of SNH replacement and DNP administration. Spearman’s correlations were used to examine the relationship between DNP use and lifetime expectancy.
Results
Ratio of DLB
We identified 510 subjects with medical records and death certificates, of whom 360 had a diagnosis of dementia that met the entry criteria. Among them, 14.2% (n=51) of patients diagnosed with DLB; 23 had taken DNP and 28 patients had not received the drug due to treatment prior to the introduction of DNP in 1999 in Japan. We classified the subjects into four groups, i.e., the DNP and SNH group (n=12), the DNP and Non-SNH group (n=11), the Non-DNP and SNH group (n=14) and the Non-DNP and Non-SNH group (n=14). Demographics for the groups are shown in Table 1.
| DNP and SNH group | DNP and Non-SNH group | Non-DNP and SNH group | Non-DNP and Non-SNH group | |
|---|---|---|---|---|
| N | 12 | 11 | 14 | 14 |
| Men/Women | 2/10 | 4/7 | 2/12 | 4/10 |
| Age (mean) | 80.1 | 80.5 | 82.8 | 82.8 |
| SD | 8.7 | 6.4 | 6.3 | 6.7 |
DNP: Donepezil; SNH: Special Nursing Home
Table 1: Demographics for four groups.
Causes of death
Table 2 shows the causes of death of the DLB patients. Pneumonia is the most main cause of death, followed by consciousness loss and suffocation.
| DNP and SNH group | DNP and Non-SNH group | Non-DNP and SNH group | Non-DNP and Non-SNH group | |
|---|---|---|---|---|
| N | 12 | 11 | 14 | 14 |
| Pneumonia | 6 | 5 | 4 | 4 |
| Consciousness loss | 4 | 4 | 2 | 2 |
| Aspiration choking | 0 | 0 | 1 | 2 |
| Sleep disturbance | 0 | 0 | 1 | 1 |
| Fracture | 0 | 0 | 1 | 1 |
| Cancer | 0 | 0 | 1 | 1 |
| Stroke | 0 | 1 | 1 | 1 |
| Heart diseases | 2 | 1 | 2 | 2 |
| Others | 0 | 0 | 1 | 0 |
DNP: Donepezil; SNH: Special Nursing Home
Table 2: Causes of death.
Lifetime expectancy
As Figure 1 shows, the lifetime expectancies after the onset were 6.4 years in the DNP group and 3.6 years in the non-DNP group, with a significant difference. However, there was no significant covariate effect of SNH residency. Other covariates did not reach a significant level.
Figure 1: Donepezil effect on lifetime expectancy in DLB.
DNP: Donepezil; DLB: Dementia with Lewy Bodies
The vertical line indicates life expectancy (months). There was a significant drug effect (F=6.18; p=0.019) with a significant covariate effect of Special Nursing Home residency (F=8.074. p=0.008) and Parkinsonism (F=7.734, p=0.009). No other covariates reached a significant level (age: F=0.105, p=0.748; gender: F=3.957, p=0.056; visual hallucination: F=1.354, p=0.254; fall: F=0.862, p=0.362; typical antipsychotic drugs: F=2.347, p=0.136; atypical antipsychotic drugs: F=0.153, p=0.698)
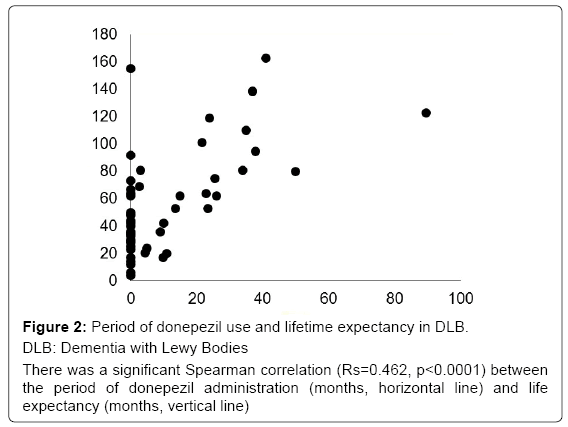
Spearman’s correlation analysis revealed that the relationship between the period of DNP use and lifetime expectancy was significantly positive (biologically meaningful) in the patients, as illustrated in Figure 2.
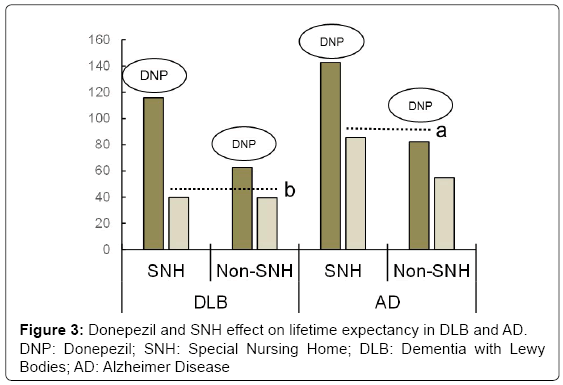
To demonstrate the difference between previous AD data [5] and the current findings, data were classified by both DNP administration and SNH residency (Figure 3). Generally, the lifetime expectancies of DLB groups were lower than those of AD for both DNP, as well as the SNH groups. It is noteworthy that for AD, the expectancy of the DNP group at home (i.e., Non-SNH) was similar to that of the non-DNP group in SNH as reported previously (see the line “a”); however, the DLB group did not exhibit any such SNH effect (see the line “b”).
Discussion
This study reported a positive effect of DNP administration but no effect of SNH replacement on lifetime expectancy after the onset of DLB.
Positive effect of DNP and negative effect of SNH residency on lifetime expectancy
DNP may have a negative effect on aspiration pneumonia, due to the side effect of nausea. Increased gastro-esophageal reflex may also induce pneumonia. This suggests that the effect of DNP on lifetime expectancy is not purely pharmacological. We previously reported [5] that the positive effects of SNH residency on AD were probably due to the following: First, DNP administration can improve psychomotor speed or attention [11,12], which is consistent with the higher mortality in older adults with lower perceptual speed [13]. Second, this improved cognitive function can smoothly lead to psychosocial intervention, and can increase the QOL. Third, their activities of daily living (ADL) are also stimulated. Wattmo et al. [14] found that drug treatment maintained higher self-supported levels of instrumental ADL. Rehabilitation also leads to a long-term effect in decreasing mortality, and particularly improves motor disability and ADL [15] and prevents aspiration pneumonia [16]. Fourth, compared with living at home, there is better management of therapy in a SNH, and finally, there was a better general environment in a SNH (i.e., good temperature and nutrition).
However, in contrast to the hypothesis, there was no significant effect of SNH residency among the DLB patients. Taking into consideration the result of lower life expectancy compared with that of AD, the lack of an effect of SNH residency suggests that the cholinergic deficiency in DLB might be greater than that in AD, although the survival after diagnosis of dementia varies considerably and depends on numerous factors and complex interactions among these factors, as described earlier. We consider that the increase of acetylcholine level approaching a healthy level in the brain might influence the “energy level” of whole body and thus the biological lifetime would be prolonged. Another possibility is that their ADL score was maintained by the drug, and Parkinson syndrome manifested by the disease did not affect the cause of death. Further investigation is needed to clarify these points.
Cause of death
Knowledge of the causes of death is of value in the terminal care of patients with dementia. Cancer, heart disease, pneumonia, and stroke remain the main causes of death among the whole Japanese population (the Ministry of Health, Labor and Welfare 2016), but not in patients with AD or DLB. Stroke and heart disease are vascular diseases that are commonly accompanied by VaD. In contrast, respiratory failure or pneumonia is common in patients with AD. In cases with clinical and pathological diagnoses of dementia and a complete autopsy, Brunnström et al. [17] reported that the two most common causes of death were bronchopneumonia and ischemic heart disease, while cancer was uncommon. Pneumonia as an immediate cause of death in dementia may reflect a terminal stage in which patient care and feeding is difficult to manage effectively.
Although the causes of death were not investigated for DLB, there were several reports on those with Parkinson disease. Specifically, age and inspired motor function [18], dementia and psychosis [19], were related to the death. Our previous findings [5] that DNP administration improved visual hallucination as a kind of psychosis manifested by DLB patients may contribute the elongation of life expectancy.
Wada et al. [20] reported that the use of antipsychotics, the presence of cerebrovascular disease in the basal ganglia, the severity of dementia, and male gender were associated with aspiration pneumonia in AD. However, our investigation of these factors did not support these relationships among patients who did and did not take donepezil (data not shown). Drugs, such as angiotensin-converting enzyme inhibitors, have been reported to improve the swallowing reflex, thus preventing the exacerbation of pneumonia [21]; however, we found no effect of these drugs (data not shown). Thus the longer life expectancy in the DNP group was considered to be due to DNP itself.
Limitation of the study
There appears to be a time bias in the data, in that patients not treated with DNP were managed prior to the introduction of this drug in Japan in the late 1990’s. However, the SNH we used in this study provides sophisticated care for patients not changed over this time period. I would say the NH environment in other countries than Japan might be less beneficial, more use of sedatives and antipsychotics, less help with feeding and toileting, etc.
This report also has the same limitation as all retrospective analyses: i.e., the lack of randomization. The small sample size should also be re-investigated using a larger cohort. The evaluation of a drug effect is essentially dependent on how patients are assigned to the drug or nondrug groups. However, observational studies can help in understanding the associated effects of drugs, since the main bias is carefully considered. We considered that there were no remarkable differences between the DNP and Non-DNP groups with respect to social status, i.e., economic status, or family support. Indeed, the patients were all residents in Tajiri, a typical agricultural town, where they were born, grew up, and got married in the same area. All men analyzed were farmers and all women analyzed were housewives, exhibiting similar life styles. This unique, “pure” social status can exclude the possible confounding effects of social factors.
Conclusion
Although this report has the limitation that all analyses were retrospective and lacked randomization, we found a positive effect of DNP on lifetime expectancy after the onset of DLB. The lower life expectancy compared with that of AD and the lack of an effect of SNH residency suggest the cholinergic deficiency in DLB is greater than that in AD.
Declarations
Ethics approval and consent to participate
The study was approved by the ethical committee (the Institutional Review Board) of Tohoku University Graduate School of Medicine, as well as that of the Osaki-Tajiri SKIP Center.
Acknowledgement
We are grateful to Ms. Yuriko Kato and Keiko Chida for technical assistance. Funding is from the regular laboratory budget, not special grants.
References
- Brodaty H, Seeher K, Gibson L (2012) Dementia time to death: A systematic literature review on survival time and years of life lost in people with dementia. Int Psychogeriatr 24: 1034-1045.
- Meguro K, Ishii H, Yamaguchi S, Ishizaki J, Shimada M, et al. (2002) Prevalence of dementia and dementing diseases in Japan: The Tajiri project. Arch Neurol 59: 1109-1114.
- Satoh M, Ishikawa H, Meguro K, Kasuya M, Ishii H, et al. (2010) Improved visual hallucination by donepezil and occipital glucose metabolism in dementia with Lewy Bodies: The Osaki-Tajiri Project. Eur Neurol 64: 337-344.
- Meguro M, Kasai M, Akanuma K, Ishii H, Yamaguchi S, et al. (2008) Comprehensive approach of donepezil and psychosocial intervention on cognitive function and quality of life for Alzheimer’s disease: The Osaki-Tajiri project. Age Ageing 37: 469-473.
- Meguro K, Kasai M, Akanuma K, Meguro M, Ishii H, et al. (2014) Donepezil and life expectancy in Alzheimer’s disease: A retrospective analysis in the Tajiri project. BMC Neurol 14: 83.
- Meguro K, Akanuma K, Meguro M, Kasai M, Ishii H, et al. (2015) Lifetime expectancy and quality-adjusted life-year in Alzheimer’s disease with and without cerebrovascular disease: Effects of nursing home replacement and donepezil administration - A retrospective analysis in the Tajiri Project. BMC Neurol 15: 227.
- McKhann G, Drachman D, Folstein M, Katzman R, Price D, et al. (1984) Clinical diagnosis of Alzheimer's disease: Report of the NINCDS-ADRDA work group under the auspices of department of health and human services task force on Alzheimer's disease. Neurology 34: 939-944.
- Róman GC, Tatemichi TK, Erkinjuntti T, Cummings JL, Masdeu JC, et al. (1993) Vascular dementia: Diagnostic criteria for research studies: Report of the NINDS-AIREN International Workshop. Neurology 43: 250-260.
- The Lund and Manchester Groups (1994) Clinical and neuropathological criteria for frontotemporal dementia. J Neurol Neurosurg Psychiatry 57: 416-418.
- McKeith IG, Dickson DW, Lowe J, Emre M, O'Brien JT, et al. (2005) Consortium on DLB. Diagnosis and management of dementia with Lewy bodies: Third report of the DLB consortium. Neurology 65: 1863-1872.
- Shimizu S, Hanyu H, Iwamoto T, Koizumi K, Abe K (2006) SPECT follow-up study of cerebral blood flow changes during Donepezil therapy in patients with Alzheimer’s disease. J Neuroimaging 16: 16-23.
- Yoshida T, Ha-Kawa S, Yoshimura M, Nobuhara K, Kinoshita T, et al. (2007) Effectiveness of treatment with donepezil hydrochloride and changes in regional cerebral blood flow in patients with Alzheimer’s disease. Ann Nucl Med 21: 257-265.
- Maier H, Smith J (1999) Psychological predictors of mortality in old age. J Gerontol B Psychol Sci Soc Sci 54: 44-54.
- Wattomo C, Paulsson E, Minthon L, Londos E (2013) A longitudinal study of risk factors for community-based home help services in alzheimer’s disease: The influence of cholinesterase inhibitor therapy. Clin Interv Aging 8: 329-339.
- Langhorne P, Wagenaar R, Partridge C (1996) Physiotherapy after stroke: More is better? Physiother Res Int 1: 75-88.
- Hinchey JA, Shephard T, Furie K, Smith D, Wang D, et al. (2005) Stroke practice improvement network investigators. Stroke 36: 1972-1976.
- Brunnström HR, Englund EM (2009) Cause of death in patients with dementia disorders. Eur J Neurol 16: 488-492.
- Järvelä JT, Rinne JO, Eskola O, Kaasinen V (2014) Mortality in Parkinson's disease is not associated with the severity of early dopaminergic defect. Parkinsonism Relat Disord 20: 894-897.
- Forsaa EB, Larsen JP, Wentzel-Larsen T, Goetz CG, Stebbins GT, et al. (2010) A 12-year population-based study of psychosis in Parkinson disease. Arch Neurol 67: 996-1001.
- Wada H, Nakajoh K, Satoh-Nakagawa T, Suzuki T, Ohrui T, et al. (2001) Risk factors of aspiration pneumonia in Alzheimer's disease patients. Gerontology 47: 271-276.
- Kobayashi S, Hanagama M, Yanai M, Kubo H (2011) Prevention of chronic obstructive pulmonary disease exacerbation by angiotensin-converting enzyme inhibitors in individuals with impaired swallowing. J Am Geriatr Soc 59: 1967-1968.
Citation: Meguro K, Kumai K, Takada J, Chida K, Kato Y (2018) Lifetime Expectancy in Dementia with Lewy Bodies: Effects of Donepezil Administration and Special Nursing Home Replacement. A Retrospective Analysis in the Tajiri Project. J Alzheimers Dis Parkinsonism 8: 416. DOI: 10.4172/2161-0460.1000416
Copyright: ©2018 Meguro K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 7638
- [From(publication date): 0-2018 - Sep 18, 2024]
- Breakdown by view type
- HTML page views: 6962
- PDF downloads: 676