Research Article Open Access
Life after the Emergency Services: An Exploratory Study of Well Being and Quality of Life in Emergency Service Retirees
Bracken-Scally. M1*, McGilloway. S1, Gallagher. S2, & Mitchell. J.T3
1Department of Psychology, National University of Ireland Maynooth (NUIM), Ireland
2National Ambulance Service, Health Service Executive, Ireland
3Department of Emergency Health Services, University of Maryland Baltimore County (UMBC), USA
Visit for more related articles at International Journal of Emergency Mental Health and Human Resilience
Abstract
Much is known about the negative impact of emergency services work, but no studies, to date, have investigated its long-term consequences. This cross-sectional study assesses the possible long-term effects on quality of life, of trauma exposure and emergency work in a sample of retirees from the Irish emergency services (n=169) and a comparison group of non-emergency service retirees (n=140). A multi-questionnaire postal survey was administered to assess quality of life (QoL; WHOQOL-BREF), experiences of trauma, and trauma symptoms (PSS-SR). QoL was significantly better in non-emergency retirees, whilst this group also had significantly fewer trauma symptoms. Incidents involving children were identified by a large proportion of emergency retirees as being particularly difficult to manage. The findings address a significant gap in our knowledge around the possible longer term effects of emergency services work in an often neglected sub-group. Factors associated with increased QoL and reduced symptoms of PTSD are discussed, as are some possible recommendations for the future.
Keywords
Emergency services, Trauma exposure, PTSD, Quality of life, Mental health, Healthy ageing
Background
There is an extensive established literature on occupational stress and its impact on overall health and well being. For example, Thoits (2010) stated that stress exposure has a significant impact on the risk of psychological distress, depression and other psychiatric disorders, while Nakao (2010) argued that job stress is also linked to cardiovascular disease and insomnia and often impacts well being by contributing to negative health behaviours. There is a growing interest in traumatic events and their subsequent psychological effects. A considerable body of research has illustrated the negative effects on mental health, both of work-related stress and/or exposure to distressing events (Flett, Kazantzis, Long, et al., 2002; Kazantzis et al., 2010; Wang et al., 2010).
One of the most distinctive characteristics of emergency service work is the reality of regular exposure to trauma; “they see the devastation, smell the odor of lost life, and hear the cries of families and victims alike” (Eriksson, Foy & Larson, 2004, p.246). Confronting such events can result in a tremendous burden (Eriksson et al., 2004). For example, the majority of Irish ambulance personnel report that their health has been affected by a Critical Incident (CI; Gallagher & McGilloway, 2009); this may be defined as a crisis event of intense severity which overwhelms usual coping mechanisms or ways in which people typically cope when faced with day-to-day stress on a regular basis (Everly & Mitchell, 1997). Furthermore, our earlier work found that 42% of ambulance personnel would benefit from formal mental health intervention (Gallagher & McGilloway, 2009). A number of studies have also shown similar effects, including linkages between trauma exposure and general psychopathology, PTSD symptoms, as well as a deterioration in physical health (e.g. Alexander & Klein, 2001; Blaney, 2009; Chamberlin & Green, 2010; Hill & Brunsden, 2009; Marmar et al., 1999; Mitani et al., 2006; Sterud et al., 2006; Ward, Lombard & Gwebushe, 2006).
The effects of trauma can be cumulative and sometimes a reaction to stress does not occur at the time of the incident, but rather may occur days, weeks, months, or even years after the event (Bonanno, Westphal & Mancini, 2011). Such delayed stress responses tend to be incident specific and occur as the direct result of a critical incident (Mitchell & Bray, 1990). Therefore, it is important to consider and study the potentially long term effects, if any, of trauma exposure. For example, in a study of the long-term effect of trauma exposure in military veterans, Schnurr et al. (1998) found that physical symptoms increased by 29% per decade, demonstrating that the impact of trauma may increase in terms of severity of physical symptoms over time. Krause, Shaw and Cairney (2004) also linked trauma exposure with ill health in old age, with trauma occurring between the ages of 18-64 years as most strongly related to health in old age (i.e. when compared to trauma experienced as a child or after 65 years).
Importantly, most people adjust to, and recover successfully from, trauma with the passage of time although the extent to which an individual might be considered resilient (or not), can influence their likelihood of developing longer term mental health problems (King, Vogt & King, 2004). Resilience may be defined as an ability to “rapidly and effectively rebound from psychological and/or behavioural perturbations associated with critical incidents, terrorism, and even mass disasters” (Kaminsky et al., 2007). However, psychopathology only occurs in a minority of those exposed to traumatic events (Peterson, Park, Pole, et al., 2008). It is also important to note that negative outcomes and consequences represent only one of many possible post-trauma outcomes (Shakespeare-Finch, Smith, Gow, et al., 2003) and indeed, a growing body of literature focuses on posttraumatic growth (i.e. an increased development of psychological well being and a universal tendency to pursue accommodation following changes in life; Joseph & Linley, 2008). While a significant amount of research has demonstrated that prior trauma can sensitise individuals to future trauma, other studies have shown that it may also act as a buffer to the impact of any subsequent trauma (King et al., 2004).
However, a question that remains largely unanswered, concerns the longer term residual impact of emergency services work on those who have retired from the emergency services. This study was undertaken as part of a larger study that explored the quality of life and well being of retired emergency services personnel. The objectives of the study reported here are: (1) to ascertain the long-term effects on overall QoL of working in the emergency service; (2) to examine the levels of PTSD symptomatology in emergency service retirees; (3) to explore the kinds of incidents which remain with emergency personnel into retirement; and (4) to investigate factors linked with quality of life and trauma symptoms in a sample of emergency service retirees.
Method
Participants
Both the ambulance and fire services were involved in this cross-sectional study. Access to a population of emergency retirees (n=565) was secured with the assistance of senior personnel in these organisations and each retiree was initially contacted by their former employer to request their consent to have their contact details released to the research team; 38% of this population agreed to be contacted. The non-emergency service population (public sector) was selected because of its similarity to emergency retirees in terms of its predominantly male profile and its relative accessibility. Access to this group (n=507) was secured with the assistance of district leaders who work as part of the retired members associations, and questionnaire packs were posted by these individuals to all retirees.
Measures
A multi-questionnaire postal survey was administered to elicit background details and to assess quality of life (WHOQOL-BREF) and trauma symptomatology (PSS-SR). A Background Questionnaire was devised to elicit information on age, etc as well as perceived resilience (i.e. the extent to which someone is able to recover quickly from unpleasant or damaging events). As part of an investigation of the long term impact of trauma, respondents were also asked to provide details of any incident during their professional or personal lives which they found most difficult to deal with personally.
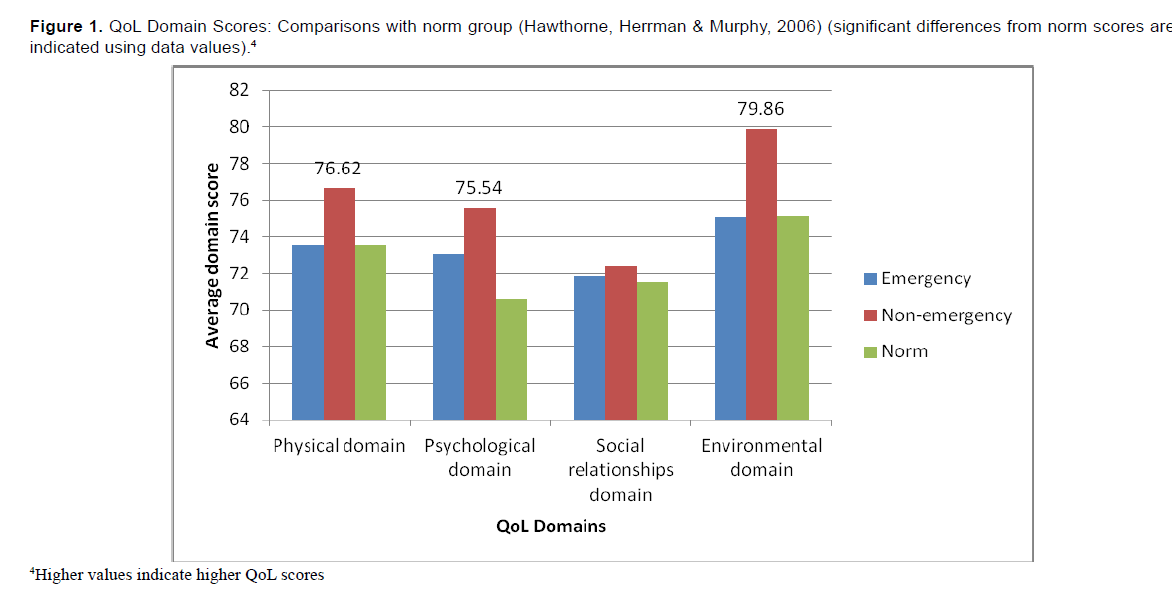
The World Health Organisation Quality of Life BREF (WHOQOL-BREF), an abridged version of the WHOQOL-100 (WHO, 1997), comprises 26 items which assess quality of life and well being within four domains: physical; psychological; social relationships; and environmental (De Maeyer, Vanderplasschen & Broekaert, 2010). Domain scores can be derived, as well as two individual scores for perceptions of quality of life and health. Domain scores indicate an individual’s perception of quality of life in each domain and are scaled positively in that higher scores indicate higher quality of life.
The Post-Traumatic Symptom Scale Self-Report version (PSS-SR) (Foa et al., 1993) is a 17-item tool that examines the occurrence of three clusters of PTSD (re-experiencing, arousal and avoidance) during the previous month. PTSD cases were identified using symptom counts; this establishes the presence of the disorder by counting the number of clinically significant symptoms endorsed. Thus, symptoms are deemed to be clinically significant (i.e. ‘full’ PTSD) if, one or more re-experiencing symptoms is present, as well as three or more avoidance symptoms and two or more arousal symptoms. When just two of these three conditions are present, PTSD symptoms may be categorised as ‘partial’.
The four-item CAGE (Ewing, 1984) was also used to assess levels of problem drinking. This includes questions relating to Cutting down, Annoyance by criticism, Guilty feeling, and Eye openers (Ewing, 1984). This tool has been recommended for use with older adults (Sorocco & Ferrell, 2006). It was important to include an assessment of problem drinking as alcohol use among older adults is common and is liked to a variety of health and social problems (St John et al., 2010), including a negative impact on older adults across physical, social and psychological domains (Bowman & Gerber, 2006).
Results
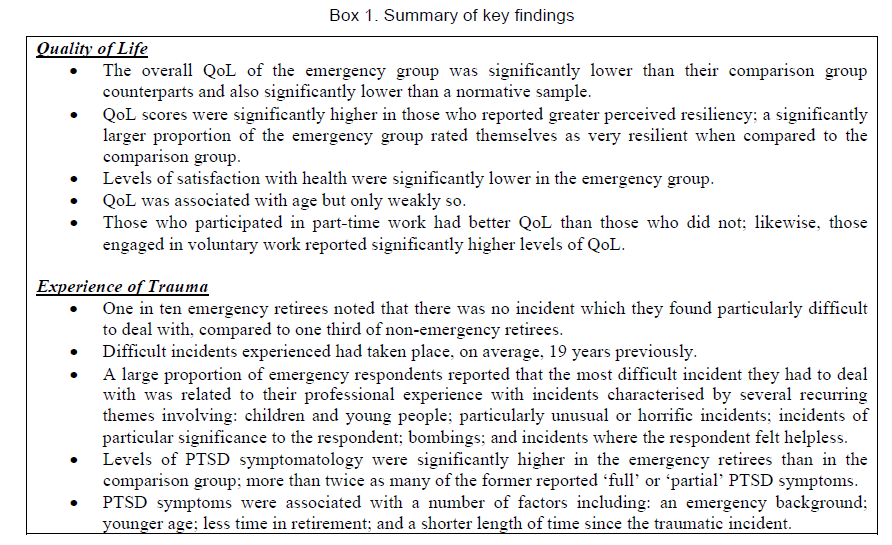
A summary of key findings from the study is presented in Box 1.
Participant Profile
There was a 79% response rate (n=169/213; 114 fire service and 55 ambulance service) amongst those emergency service retirees who agreed to have their contact details released to the research team. By contrast, only 28% of the comparison group returned completed questionnaires (n=140/507). All but three respondents in the total sample were male (97% male) with a similar gender breakdown in both groups, and a mean overall age of approximately 68 years (M=67.80, SD=7.59, Range=41). The mean age for the emergency sample (M=65.17) was marginally lower than the non-emergency sample (M=70.95) but not statistically significantly so. Most respondents were married (85%), with a similar profile with respect to marital status. Respondents had three children on average and four grandchildren. All but three respondents reported that they were receiving a regular income (pension or otherwise, 99%) and, reassuringly, almost three-quarters (72%) believed that their income was sufficient to meet their needs.
Retirement Background
Emergency service participants were retired, on average, 7 years (SD=6.19), while non-emergency participants were retired for an average of 12 years (SD=7.01). A positive, albeit only weak, correlation was found in the emergency group, between QoL and number of years in previous occupation (r=0.19, n=164, p=0.017). Interestingly, the same was true for the non-emergency group (r=0.19, n=135, p=0.027). There was only a weak negative (marginally significant) correlation between the number of years in occupation and total PTSD symptoms in the emergency group (r= -0.150, n=166, p= 0.053).
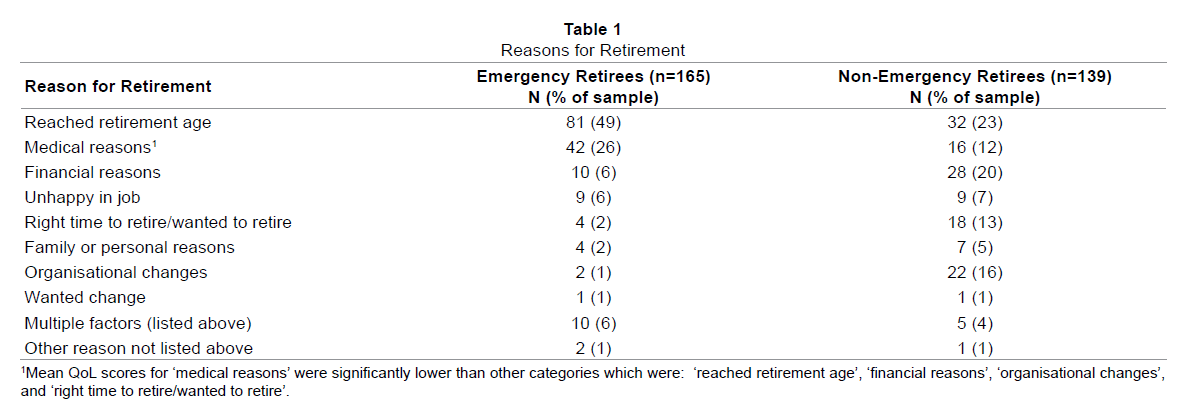
Notably, some respondents outlined more than one reason for retirement, highlighting the complex nature of the decision to retire (Table 1). A statistically significant difference in QoL scores for the categories of reason for retirement was found using a one-way between groups ANOVA (F (2, 20) = 5.5, p<0.005), however the effect size (d=0.15) was quite small. Post-hoc comparisons indicated that the mean QoL score for ‘medical reasons’ (M=397.67, SD=89.81) was significantly lower than a number of other categories including ‘organisational changes’ (M=462.51, SD=71.00), ‘reached retirement age’ (M= 468.29, SD= 67.30), ‘financial reasons’ (M= 477.64, SD=62.93), and ‘right time to retire/wanted to retire’ (M=479.83, SD=76.22) (Table 1).
Quality of Life
Importantly, the mean QoL score in the emergency sample was significantly lower than the test norm score (M=4.17, SD=0.86 versus M=4.3, SD = 0.9; t (165) =-1.97, p=0.05). By contrast, the non-emergency sample reported ‘normal’ scores (M=4.35, SD=0.72) on this dimension. With regard to satisfaction with health, the mean scores of the emergency (3.76 (SD=1.1) and norm groups (M=3.6, SD=0.9) were comparable (p>0.05), although the comparison group obtained significantly higher (above-norm) scores on this dimension (M=4.04, SD=0.81); t (138) = 6.34, p<0.001) (Table 2 for QoL domain scores). There was also a significant difference in total QoL scores for non-emergency (M=464.0, SD=68.11) versus comparison (M=441.52, SD=87.95) participants (t (300) = -2.51, p=0.013, η2= 0.02). There was a weak positive correlation between age and total QoL score (r=0.113, n=299, p=0.051). Regression analysis demonstrated that total PSS-SR score predicted 16.56% of the variance in total QoL score (beta=-0.421, p<0.0005). QoL scores differed significantly based on level of resiliency according to a one-way between groups (Group 1: ‘very resilient’, Group 2: ‘somewhat resilient’ and Group 3: ‘not at all resilient’) ANOVA; F (2,297) = 18.56, p<0.0005, although the effect size (d=0.01) was small. (Figure 1)
Emergency services group: Experience of Traumatic Events
When recounting the incident which respondents had found most difficult to deal with personally13, most emergency respondents outlined incidents related to their professional life (60%). A further 17% recounted an incident related to their personal life while 4% reported numerous incidents related to both their personal and professional lives. Incidents related to personal life (n=29) included: death of a loved one (n=12); personal illness or injury (n=8); marital breakdown or family problems (n=3); and illness or injury of a loved one (n=2). A further four respondents indicated that the death of a loved one was one of several difficult experiences which they had experienced and one respondent highlighted that marital breakdown was also one of several difficult incidents that they had encountered.
Traumatic incidents had taken place, on average, 19 years previously (n=112, Mean=18.60, Min=0.75, Max= 46, SD=12.12). Interestingly, one in ten (17/169) noted that there was no incident which they found particularly difficult to deal with in either their professional or personal life. Reasons for this included: acknowledging dealing with numerous difficult incidents but having no problem in this area (n=6); reporting that they never had a situation which was difficult to deal with (n=4); not recalling any particularly difficult incident (n=2); having no problem in dealing with difficult incidents as it was part of the job (n=2); or stating that there was “too many to worry about” (n=1). Interestingly, all but one of those who felt unaffected by trauma rated themselves as ‘very resilient’ (94%).
A large proportion of respondents reported that the single most difficult incident for them was related to their professional experience. While most of these incidents were in relation to CIs specifically, many others were in relation to events not directly related to CIs. Fifteen respondents reported an event or issue which was related to interpersonal or industrial difficulties including four who alluded to the challenge of a work-related injury. A further two respondents outlined bullying as the most difficult incident with which they had to deal, one of which led to the participant’s decision to retire which they had later regretted.
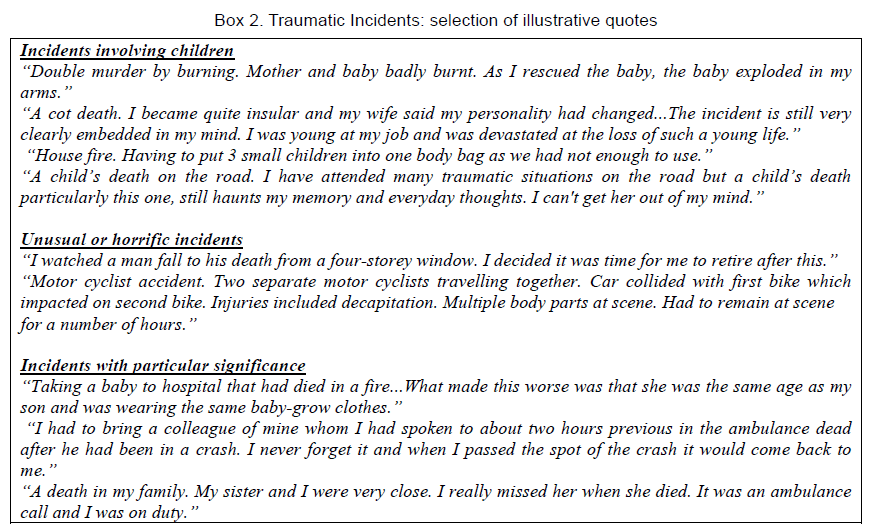
Importantly, a significant proportion of respondents (n=12) referred to a major fire which had occurred 31 years previously, as the most difficult incident they had to deal with14. For example, one respondent stated that they “found it very hard after the initial fire to deal with such a high level of death at such a young age” and that it “left mental scars for months.” A number of difficult incidents described here were characterised by recurring themes involving: children (n=23); particularly unusual or horrific incidents (n=8); incidents with particular significance to respondent (e.g. known victim (n=7), including two respondents who responded to an incident involving a family member); incidents involving young people (including suicide, n=4); bombings (n=3); and incidents where the respondent felt helpless (n=2). Some participants had experienced incidents involving more than one of the above (see Box 2). Incidents involving children or young people, those which were particularly unusual or horrific, and bombings, were themes which also arose in respondents’ descriptions of multiple incidents (Box 2).
Comparison group: Experience of Trauma
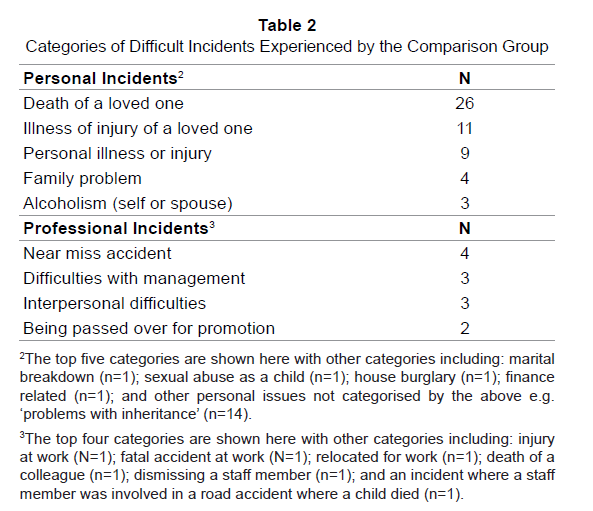
More than half of the non-emergency respondents (in contrast to the above) reported difficult incidents related to their personal life, such as death of a loved one (54%). A further 12% recounted an incident related to their professional life15. As with the emergency retiree group, these incidents had taken place, on average, 19 years previously (n=87, Mean=19.41, Min=0.25, Max=70, SD=15.52). Interestingly, one third of this sample (46/140) noted no specific incident which they found particularly difficult to deal with in either their professional or personal life (Table 2).
Potential Impact of Trauma
A significant difference in levels of PTSD symptomatology (full or partial) across groups was also evident (χ2 (1, n=309) = 10.42, p=0.001, phi=0.19). Importantly, 30% of emergency retirees displayed ‘full’ (11%) or ‘partial’ (19%) PTSD symptoms compared to 14% of non-emergency retirees (6%, and 8%). A moderate negative correlation was found between age and total PTSD symptoms (r= -0.31, n=304, p<0.0005) whilst length of time in retirement and total PTSD symptoms were also negatively correlated, albeit only weakly (r= -0.19, n=297, p=0.001). Likewise, there was a weak negative correlation between the length of time since the traumatic incident and total PTSD symptoms (r= -0.23, n=199, p=0.001).
With regard to specific symptoms, a significant difference was found with respect to re-experiencing symptoms for all those emergency (M=1.63, SD=1.66) versus non-emergency (M=1.14, SD=1.50) retirees who had reported experiencing a difficult incident (t (231) =2.29, p=0.02, η2=0.02). For example, the former typically reported feeling very “emotionally upset” when they recalled the incident (46%) or experiencing unwelcome “upsetting thoughts or images about the incident” (40%). Likewise, arousal scores were significantly higher, albeit not to a large extent, amongst the emergency (M=1.48, SD=1.74) versus non-emergency (M=0.80, SD=1.30) retirees who had experienced a difficult incident (t (229) = 3.18, p=0.002, η2=0.04). There was no significant difference in avoidance scores for the two groups.
Other Findings
Participation in part-time work was marginally higher for emergency retirees (23%) than non-emergency retirees (16%), although this fell short of significance. Interestingly, the most commonly reported form of part-time work in which this group was involved, were forms of work associated with their earlier career, such as delivering occupational first aid, although importantly, these roles did not ordinarily include exposure to critical incidents. Those who participated in part-time work reported significantly higher levels of QoL (M=474.63, SD=76.02) when compared to those who did not (M=445.74, SD=80.67) (t (296) = 2.51, p=0.013, η2= 0.02). A significantly higher proportion of non-emergency retirees (51%) participated in voluntary work when compared to emergency retirees (32%) (χ2 (1, n=303) = 10.27, p=0.001, phi= -0.19). Those engaged in voluntary work also reported significantly higher levels of QoL (M=469.17, SD=67.96) than those not engaged in such work (M=439.92.74, SD=85.74); t (292) = 3.29, p=0.001, η2= 0.03).
Interestingly, a significantly larger proportion of the emergency group (72%) rated themselves as very resilient when compared to their non-emergency counterparts (60%) (χ2 (2, n=305) =10.18, p=0.006, phi=0.18). More than one quarter of the former (28%) rated themselves as ‘somewhat resilient’ compared to 34% of the non-emergency sample, and only 1% of the emergency sample felt that they were not a resilient person compared to 7% of non-emergency retirees. Most respondents (94%) did not display levels of problem drinking (using a cut-off score of two on the CAGE).
Discussion
The principal aim of this study was to explore quality of life, trauma symptomatology and experience of trauma in emergency service retirees in order to ascertain the possible long term effects of trauma exposure and emergency service work. Overall, there were some interesting and useful findings in relation to QoL and levels of PTSD symptoms in those who had retired from the emergency services up to 31 years previously. The higher levels of QoL in the comparison group point toward the potentially detrimental effects on overall QoL of working in the emergency services. Furthermore, more than three times as many non-emergencies as emergency retirees reported that there were no incidents which they found difficult to manage, thereby indicating the considerable difference in trauma exposure between the two groups.
The fact that one in ten of the emergency group reported no difficulty in dealing with any incidents in their lives, suggests that a small minority were more resilient than their colleagues. Likewise, the fact that the great majority of the sample of emergency service retirees rated themselves as ‘very resilient’ is an important finding because resilience (along with other adaptive processes such as self-efficacy) is viewed as an important factor in successful ageing (Lamond et al., 2009). It may be useful, therefore, for emergency organisations to implement training to further foster resiliency in their personnel, to ensure that this develops in the early stages of their career and long before retirement, particularly in light of evidence that this attribute may be acquired through completion of a brief training programme (Everly et al., 2008). Previous research has also demonstrated that emergency personnel demonstrate higher levels of hardiness (Alexander & Klein, 2001), resilience (Gayton & Lovell, 2012) and psychological preparedness (Streb et al., 2013) than the general population. In the current study, higher levels of QoL were also associated with greater resiliency and this is in line with previous research demonstrating a sizeable correlation between resilience and general health and well being (Gayton & Lovell, 2012).
It is interesting to note that resiliency was higher among emergency service retirees when compared to their non-emergency service counterparts and yet the former also reported lower QoL and more severe PTSD symptoms. This may be interpreted in one of two ways. Perhaps a certain level of resiliency would, on the one hand, prevent further, even lower levels of QoL and more severe PTSD symptoms from developing. However, on the other hand, it is possible that the ‘culture’ of emergency service work expects these personnel to present themselves as strong and invincible in the face of trauma, thereby accounting for the higher levels of self-reported resiliency in this study. This is an area in need of further research.
Difficult incidents reported by emergency personnel had taken place on average 19 years previously demonstrating the potential for CIs to remain with personnel long into their retirement from the emergency services. Incidents involving children were repeatedly noted as the most difficult incident to deal with. Incidents where patients were known to the caregiver also elicited considerable distress in a relatively large proportion of this group. Likewise, Declercq et al (2011) found that CIs related to the death or serious injury of children led to distress in 51% of emergency personnel who had experienced such an incident, whilst incidents involving the death of a colleague led to distress in 56% of those who had experienced such an incident.
PTSD symptoms were associated with a number of factors including: an emergency background; younger age; less time in retirement; and a shorter length of time since the traumatic incident. A regression analysis demonstrated that total trauma symptomatology predicted almost one fifth of the variance in total QoL score, which given the multi-dimensional nature of QoL, may be considered quite substantial. Berger et al. (2012) reviewed 28 studies (n=20,000) of rescue personnel and found that the pooled prevalence of PTSD was 10% - much higher than in the general population (1.3-3.5%). Pietrzak et al. (2011) reported a lifetime prevalence of full and partial PTSD of 6.4% and 6.6% respectively in US adults. The figures in the current study are comparable, with a rate of PTSD symptomatology amongst the emergency group of almost twice that seen in the comparison sample (11% versus 6% respectively). Thus, the levels of PTSD symptomatology in the emergency sample are similar to those found in currently employed emergency service personnel. This demonstrates the potentially long term residual impact of emergency services work and trauma exposure on those who have retired from the emergency services, thereby suggesting a minority might be particularly vulnerable in this respect. Screening of all personnel in the pre-retirement period to identify those who may need special support in their retirement may be beneficial. Emergency service organisations could then implement the necessary services (e.g. counselling, guidance and retirement workshops) to deal with this group. It would also be useful, in future research, to examine the prevalence of other mental health problems in this population, such as anxiety and depression as other studies have found that an accumulation of trauma predicts depression and anxiety in older age (e.g. Dulin & Passmore, 2010).
Many retirees, across a number of occupational groups, opt to become volunteers and contribute towards others and unpaid work is common amongst retirees as they fulfil the “working” role in their lives (Lazarus & Lazarus, 2006). The current study found, in line with other research, that QoL was higher for those engaged in voluntary work. For example, Hoyer and Roodin (2009) argue that voluntary work provides a number of health benefits including an increase in life space, satisfaction, well being, and self-efficacy. Brenner and Shelley (1998) highlighted the importance of emphasising the value of voluntary work for retirees, as it can provide purpose and focus, as well as social contact. Therefore, emergency service organisations might consider encouraging participation in voluntary work for employees, both prior to, and within retirement and especially work that involves the application of their knowledge and skills.
According to the literature (e.g. Mitchell and Bray, 1990), emergency service personnel have a different personality type from those working in other occupations; they often have very high personal standards, pride themselves on a perfect job, and become quite frustrated in the face of failure. Furthermore, a large body of work conducted during the 1980s and 1990s has shown that the personalities of ambulance, fire and law enforcement personnel are quite similar (as are their reactions to traumatic events). In addition, irrespective of their position/job role upon retirement, arguably, most if not all would be unlikely to forget their previous experiences ‘on the frontline’; indeed, this is borne out by the current study findings. Pinquart and Schindler (2007) demonstrated that satisfaction in retirement can also vary; while for some, satisfaction declines in retirement and then continues in a stable or trajectory pattern, for others, satisfaction may increase but decline steadily thereafter; others may experience a temporary minor increase in satisfaction on retirement. Therefore, it might be beneficial in the future, to examine the quality of life and PTSD symptoms of emergency service retirees (and a matched comparison group) on a longitudinal basis from the moment of retirement (or just before) and through subsequent months and years in order to track any changes over time and to identify factors associated with such change.
The findings reported here, provide useful information for emergency service organisations in to inform the development and refinement of their retirement policies and procedures. For example, current policies and procedures for emergency personnel in Ireland do not include support for personnel post-retirement and it would be useful to explore the benefits of further developing these policies in this regard. The findings also suggest that trauma should be dealt with before retirement, so it is important that these findings are also considered by emergency service organisations in the enhancement of their psychosocial support systems and policies (e.g. Critical Incident Stress Management; Everly & Mitchell, 1997). It may also be beneficial for such organisations to implement mandatory support following incidents that have been identified as commonly causing distress or difficulties in personnel.
The current study is unique and addresses an important knowledge gap in exploring, for the first time, quality of life following retirement amongst former emergency service personnel, and the potential long term impact of prolonged trauma exposure on emergency service personnel in retirement. However, the cross-sectional nature of the study precluded any before-and-after comparisons or assessments of change over time. Participants also self-selected for study participation and no clinical assessment of PTSD was undertaken. Arguably, the use of self report measures is a limitation of this study, but research on older people has shown that self ratings of health are significantly related to measures of objective health status and are, therefore, a more practical method of gaining information from this population (Ferraro, 1980). Furthermore, as QoL is a subjective experience, it has been argued that it is best assessed by the individual (Skevington, 1999) whilst evidence has also shown that brief screening tools are a viable way of assessing PTSD/PTSD symptoms (Brewin et al., 2002).
Nonetheless, the study findings provide useful insights into the experiences and quality of life of emergency service retirees and in so doing, provide a critical starting point for the exploration of the experiences, health and well being, and QoL amongst an important, but neglected sub-group. The findings also provide important information for emergency service organisations both in Ireland and elsewhere that should help to inform the development of policies and procedures on health and well being, resiliency, and retirement. It is critical, though, that further research is undertaken in order to ensure that those retired from the emergency services do not remain our “forgotten helpers”. Longitudinal studies could be used to more easily establish causality (Lewin, 2012) and to assess changes over time (Gray, 2009). Future research could also consider the nature and extent of training required within emergency services to provide timely, appropriate and effective psychosocial support systems and procedures and also to promote greater resiliency in their frontline personnel.
Acknowledgements
The authors would like to thank all those who supported the development and implementation of this study including both of the emergency services who kindly participated in the study and, in particular, all those who took part in the research. We also gratefully acknowledge the support of the National Ambulance Service CISM Committee.
13Fourteen respondents (8%) did not respond to this question; however eight of these individuals did complete the PSS-SR which would indicate they have experienced a difficult incident.
14Three of these also outlined one or more other difficult incidents
15A further two individuals provided no details.
References
- Alexander, D., & Klein, S. (2001). Ambulance Personnel and Critical Incidents: Impact of Accident and Emergency Work on Mental Health and Emotional Well-Being. The British Journal of Psychiatry, 178, 76-81
- Berger, W., Coutinho, S., Figueira, I., Marques-Portella, C., Luz, M., Neylan, T., et al. (2012). Rescuers at Risk: A Systematic Review and Meta-Regression Analysis of the Worldwide Current Prevalence and Correlates of PTSD in Rescue Workers. Social Psychiatry Psychiatric Epidemiology, 47, 1001-1011
- Blaney, L. (2009). Beyond ‘Knee Jerk’ Reaction: CISM as a Health Promotion Construct. The Irish Journal of Psychology, 30, 37-57
- Bonnano, G.A., Westphal, M., & Mancini, A.D. (2011). Resilience to Loss and Potential Trauma. Annual Review of Clinical Psychology, 7, 511-535
- Bowman, P., & Gerber, S. (2006). Alcohol in the Older Population, Part 2: MAST You Speak the Truth in an AUDIT or Are You Too CAGE-y? The Case Manager, 17, 48-53
- Brenner, H., & Shelley, E. (1998). Adding Years to Life and Life to Years: A Health Promotion Strategy for Older People. National Council on Ageing and Older People: Dublin, Ireland
- Brewin, C., Rose, S., Andrews, B., Green, J., Tata, P., McEvedy, C., et al. (2002). Brief Screening Instrument for Post-Traumatic Stress Disorder. British Journal of Psychiatry, 181, 158-162
- Chamberlin, M., & Green, H. (2010). Stress and Coping Strategies Among Firefighters and Recruits. Journal of Loss and Trauma, 15, 548-560
- Declercq, F., Meganck, R., Deheegher, J., & Van Hoorde, H. (2011). Frequency of and Subjective Response to Critical Incidents in the Prediction of PTSD in Emergency Personnel. Journal of Traumatic Stress, 24, 133-136
- De Maeyer, J., Vanderplasschen, W., & Broekaert, E. (2010). Quality of Life Among Opiate-Dependent Individuals: A Review of the Literature. International Journal of Drug Policy, 21, 364-380
- Dulin, P., & Passmore, T. (2010). Avoidance of Potentially Traumatic Stimuli Mediates the Relationship Between Accumulated Lifetime Trauma and Late-Life Depression and Anxiety. Journal of Traumatic Stress, 23, 296-299
- Eriksson, C., Foy, D., & Larson, L. (2004). When the Helpers Need Help: Early Intervention for Emergency and Relief Services Perosnnel. In Litz, B. (Ed.). Early Intervention for Trauma and Traumatic Loss. London: The Guilford Press
- Everly, G. S., & Mitchell, J. T. (1997). Critical Incident Stress Management (CISM): A New Era and Standard of Care in Crisis Intervention. Elliott City, MD, USA: Chevron
- Everly, G.S., Welzant, V., & Jacobson, J.M. (2008). Resistance and resilience: the final frontier in traumatic stress management. International Journal of Emergency Mental Health, 10, 261-270
- Ewing, J. (1984). Detecting Alcoholism: The CAGE Questionnaire. Journal of the American Medical Association, 252, 1905-1907
- Ferraro, K. (1980). Self-Ratings of Health Among the Old and the Old-Old. Journal of Health and Social Behaviour, 21, 377-383
- Flett, R., Kazantzis, N., Long, N., MacDonald, C., & Millar, M. (2002). Traumatic Events and Physical Health in a New Zealand Community Sample. Journal of Traumatic Stress, 15, 303-312
- Foa, E., Riggs, D., Dancu, C., & Rothbaum, B. (1993). Reliability and Validity of a Brief Instrument for Assessing Post-Traumatic Stress Disorder. Journal of Traumatic Stress, 6, 459-473
- Follette, V., & Pistorello, J. (2007). Finding Life Beyond Trauma: Using Acceptance and Commitment Therapy to Heal from Post-Traumatic Stress and Trauma-Related Problems. New Harbinger Publications Inc: Oakland, Canada
- Gallagher, S. & McGilloway, S. (2009). Experience of Critical Incident Stress Amongst Ambulance Service Staff and Relationship to Psychological Symptoms. International Journal of Emergency Mental Health. 11, 235-248
- Gayton, S., & Lovell, G. (2012). Resilience in Ambulance Service Paramedics and its Relationship with Well-Being and General Health. Traumatology, 18, 58-64
- Gray, D. (2009). Doing Research in the Real World. SAGE: London, UK
- Hawthorne, G., Herrman, H., & Murphy, B. (2006). Interpreting the WHOQOL-BREF: Preliminary population norms and effect sizes. Social Indicators Research, 77, 37-59
- Hill, R., & Brunsden, V. (2009). ‘Heroes’ as Victims: Role Reversal in the Fire and Rescue Service. The Irish Journal of Psychology, 30, 75-86
- Hoyer, W., & Roodin, P. (2009). Adult Development and Aging. Sixth Edition. McGraw Hill: Boston, MA, USA
- Joseph, S., & Linley, P. (2008). Trauma, Recovery and Growth: Positive Psychological Perspectives on Posttraumatic Stress. John Wiley and Sons: New Jersey, USA
- Kaminsky, M., McCabe, O.L., Langlieb, A.M., & Everly, G.S. (2007). An Evidence-Informed Model of Human Resistance, Resilience, and Recovery: The Johns Hopkins’ Outcome-Driven Paradigm for Disaster Mental Health Services. Brief Treatment and Crisis Intervention, 7, 1-11
- Kazantzis, N., Flett, R., Long, N., MacDonald, C., Millar, M., & Clark, B. (2010). Traumatic Events and Mental Health in the Community: A New-Zealand Study. International Journal of Social Psychiatry, 56, 35-49. King, D., Vogt, D., & King, L. (2004). Risk and Resilience Factors in the Etiology of Chronic Posttraumatic Stress Disorder. In Litz, B. (Ed). Early Intervention for Trauma andTraumatic Loss. London: The Guilford Press
- Krause, N., Shaw, B., & Cairney, J. (2004). A Descriptive Epidemiology of Lifetime Trauma and the Physical Health Status of Older Adults. Psychology and Aging, 19, 637–648
- Lamond, A., Depp, C., Allison, M., Langer, R., Reichstadt, J., Moore, D., et al. (2009). Measurement and Predictors of Resilience Among Community-Dwelling Older Women. Journal of Psychiatric Research, 43, 148-154
- Lazarus, R., & Lazarus, B. (2006). Coping with Aging. Oxford University Press: Cary, NC, USA
- Lewin, C. (2012). Understanding and Describing Quantitative Data. In Somekh, B., & Lewin, C. (eds). Theory and Methods in Social Research. Second Edition. SAGE: London, UK
- Marmar, C., Weiss, D., Metzler, T., Delucchi, K., Best, S., & Wentworth, K. (1999). Longitudinal Course and Predictors of Continuing Distress Following Critical Incident Exposure in Emergency Services Personnel. The Journal of Nervous & Mental Disease, 187, 15-22
- Mitani, S., Fujita, M., Nakata, K., & Shirakawa, T. (2006). Impact of Post-Traumatic Stress Disorder and Job-Related Stress on Burnout: A Study of Fire Service Workers. Journal of Emergency Medicine, 31, 7-11
- Mitchell, J., & Bray, G. (1990). Emergency Services Stress. Englewood Cliffs, NJ: Brady
- Nakao, M. (2010). Work-Related Stress and Psychosomatic Medicine. Biopsychosocial Medicine, 4, 4-9
- Peterson, C., Park, N., Pole, N., D’Andrea, W., & Seligman, M. (2008). Strengths of Character and Post-Traumatic Growth. Journal of Traumatic Stress, 21, 214-217
- Pietrzak, R., Goldstein, R., Southwick, S., & Grant, B. (2011). Prevalence and Axis I Comorbidity of Full and Partial Post-Traumatic Stress Disorder in the United States: Results from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Anxiety Disorders, 25, 456-465
- Pinquart, M., & Schindler, I. (2007). Changes of Life Satisfaction in the Transition to Retirement: A Latent Approach. Psychology and Aging, 22, 442-455
- Schnurr, P., Spiro, A., Aldwin, C., & Stukel, T. (1998). Physical Symptom Trajectories Following Trauma Exposure: Longitudinal Findings from the Normative Aging Study. Journal of Nervous and Mental Disease, 186, 522–528
- Shakespeare-Finch, J., Smith, S., Gow, K., Embelton, G., & Baird, L. (2003). The Prevalence of Post-Traumatic Growth in Emergency Ambulance Personnel. Traumatology, 9, 58-70
- Skevington, S. (1999). Measuring Quality of Life in Britain: Introducing the WHOQOL-100. Journal of Psychosomatic Research, 47, 449-459
- Sorocco, K., & Ferrell, S. (2006). Alcohol Use Among Older Adults. The Journal of General Psychology, 133, 453-467
- Sterud, T., Ekeberg, Ø, & Hem, E. (2006). Health Status in the Ambulance Services: A Systematic Review. BMC Health Services Research, 6, 82-92
- St John, P., Snow, W., & Tyas, S. (2010). Alcohol Use Among Older Adults. Reviews in Clinical Gerontology, 20, 56-68
- Streb, M., Haller, P., & Michael, T. (2013). PTSD in Paramedics: Resilience and Sense of Coherence. Behavioural and Cognitive Psychotherapy, Published online at http://journals.cambridge.org/action/displayAbstract?fromPage=online&aid=8929136&fulltextType=RA&fileId=S1352465813000337
- Thoits, P. A. Stress and Health: Major Findings and Policy Implications. Journal of Health and Social Behavior, 51, S41-S53
- Wang, Z., Inslicht, S., Metzler, T., Henn-Haase, C., McCaslin, S., Tong, H., et al. (2010). A Prospective Study of Predictors of Depression Symptoms in Police. Psychiatry Research, 175, 211-216
- Ward, C., Lombard, C., & Gwebushe, N. (2006). Critical Incident Exposure in South African Emergency Services Personnel: Prevalence and Associated Mental Health Issues. Emergency Medicine Journal, 23, 226-231
- World Health Organisation (WHO; 1997). Measuring Quality of Life: The World Health Organisation Quality of Life Instruments. World Health Organisation: Switzerland.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 16154
- [From(publication date):
March-2014 - Jul 14, 2025] - Breakdown by view type
- HTML page views : 11347
- PDF downloads : 4807