Review Article Open Access
Leptospirosis: An Infectious Emerging Waterborne Zoonosis of Global Significance
Mahendra Pal1* and Angesom Hadush21Addis Ababa University, College of Veterinary Medicine, Ethiopia
2College of Veterinary Medicine, Samara University, Samara, Ethiopia
- *Corresponding Author:
- Prof. Dr Mahendra Pal
Ex-Professor of Veterinary Public Health
Addis Ababa University
College of Veterinary Medicine
Debre Zeit, Ethiopia
Tel: +251114338450
E-mail: palmahendra2@gmail.com
Received Date: March 04, 2017; Accepted Date: March 09, 2017; Published Date: March 15, 2017
Citation: Pal M, Hadush A (2017) Leptospirosis: An Infectious Emerging Waterborne Zoonosis of Global Significance. Air Water Borne Dis 6: 133. doi: 10.4172/2167-7719.1000133
Copyright: © 2017 Pal M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Air & Water Borne Diseases
Abstract
Leptospirosis, caused by Leptospira interrogans, is a highly infectious emerging water borne zoonosis of global significance. It is an enigmatic life threatening disease, which results into high morbidity and mortality, particularly in poor resource nations. Disease is endemic in many countries of the world including India. Currently, over one million people are affected with leptospirosis worldwide annually. Leptospirosis presents an occupational hazard of the persons who have direct or indirect contact with the urine of infected animals. The common mode of transmission of the disease is exposure to and ingestion of urine contaminated water. Clinical signs in humans may vary from asymptomatic to severe stage with a range of non-specific symptoms. Rodents are the chief reservoir of Leptospira, and organisms are excreted in urine, thus contaminating the environment including water. Disease is endemic in tropical regions of the world with maximum cases in young male adults during the rainy season. Pollution of city water supply may result in outbreak of disease. Severe epidemics of leptospirosis are related to water recreational activities. The diagnosis of disease is confirmed by detection of serum antibodies against Leptospira and also by isolation of the pathogen from clinical specimens such as blood, cerebrospinal fluid and urine. Early treatment with antibacterial antibiotics may shorten the duration of fever and reduce the severity of the disease. As leptospirosis is attributed to physical contact with contaminated water supplies, environmental detection is important in the development of adequate control measures. There is a need to develop an effective surveillance system to monitor the trends of disease. Sincere attempts should be made to estimate the annual burden of cases and deaths due to leptospirosis. Additional studies on the epidemiology, diagnosis, chemotherapy and vaccines are required to control this life threatening zoonosis.
Keywords
Animals; Developing countries; Emerging water borne zoonosis; Leptospirosis; Public health; Surveillance
Introduction
In the last decades, several zoonoses of diverse etiologies have emerged from developing as well as developed nations of the world [1]. A plethora of factors are responsible for the emergence and reemergence of zoonosis [1]. Among these, leptospirosis ( cane cutter’s fever, cane field fever, harvest fever, hemorrhagic jaundice, mud fever, rat catcher’s disease, rice field worker’s fever, swamp fever, swine herd’s disease, Weil’s disease) is a most commonly occurring zoonotic disease of worldwide distribution, and carries significant morbidity and mortality [2]. Globally, leptospirosis is estimated to cause 1.03 million cases and 58,900 deaths every year [3]. The disease is caused by the corkscrew-shaped bacterium Leptospira interrogans, found in aquatic environment [2]. The first description of leptospirosis goes back to the year 1886 when Adolf Weil of Germany reported an acute infectious disease with jaundice, nephritis and enlargement of spleen in a human patient [2]. After two decades, a spirochete in a patient with Weil’s disease that died from ‘yellow fever’ was recovered and named Spirocheta interrogans as a causative agent. The same spirochete was later isolated independently in both Japan and Germany and was named as Spirocheta icterohaemorrhagiae. Two years later, this organism showed difference from other spirochetes and was reclassified into a new genus called Leptospira [4,5].
Leptospirosis is essentially water borne infection, as several outbreaks of disease have been recorded during rainy season. There appears to be direct correlation between the amount of rainfall and incidence of disease [2]. It is an emerging and re-emerging zoonosis in many regions of India. Disease is most commonly encountered in tropical regions during rainy seasons and in temperate regions in the late summer and early fall [6]. The reservoir of pathogenic leptospirosis is the renal tubules of wild and domestic animals. The organisms are usually shed in the urine of infected animals for about a month after infection. Infection in humans occurs following exposure to contaminated water sources [2,7]. Human infection occurs through exposure to Leptospira organisms via cuts and scrapes, passage across the conjunctiva and mucous membranes [1,8,9].
Leptospirosis is commonly diagnosed in several animal species such as cattle, dogs, goats, horses, pigs, and sheep [1,2]. A large number of sylvatic and domestic animals serve as reservoir of Leptospira. Human infections are caused by L. interrogans of which there are over 200 known pathogenic serovars [1]. Several modes of transmission are involved in leptospirosis [1]. Disease is transmitted by direct and indirect contact. Milk and milk products contaminated by the urine of rat urine may become a potential threat to human health. The spectrum of disease ranges from subclinical infection to a severe syndrome of multi-organ dysfunction characterized by fever, headache, myalgia, jaundice, hepatomegaly and convulsions [2,4,10]. Leptospirosis is recognized as an occupational hazard in industries related to agriculture, sewer maintenance, and animal husbandry, and results from direct or indirect contact with the urine of infected animals [2].
Outbreaks of leptospirosis have been associated with common water events such as water flooding, swimming, and other water sports as well as occupational exposure involved predominantly with farming and drinking contaminated water [11-14]. Both pathogenic and saprophytic strains of leptospirosis have been isolated from water sources including rivers and lakes as they are able to survive in moist soil and fresh water for long periods of time. Leptospires require fresh water to remain viable in the environment and can survive for several months in running water but only several weeks in stagnant water, while some halophilic strains may be recovered from brackish and salt water [11,15-17]. Therefore, objective of this paper is to review leptospirosis as emerging water borne zoonosis of global significance.
Etiology
Leptospirosis is caused by spirochaetes from the genus Leptospira currently contains 20 species containing nine pathogenic, six saprophytic, and five intermediate species [18]. The organism, Leptospira was first observed in 1907 from the renal tissue of a patient at postmortem. The spirochete Leptospira interrogans, has 20 serogroups and more than 280 serovars [1]. Leptospires are thin, obligate aerobe, fine spiral shaped organisms with hooked ends having two or more axial filaments that are responsible for the motion of the spirochete, and are visualized under dark field microscopy. The epidemiology of most serovars is poorly studied but certain serovars have been linked strongly to specific animal reservoirs [6]. Some of the serotypes are present globally, while others are confined to certain areas. Commonly known serovars are L. interrogans serovars Pomona (swine), L.interrogans Bratislava (swine), L. interrogans Canicola (dogs), L.interrogans Bovis (cattle), L. interrogans Autumnalis (raccoons), and Icterohemorrhagiae and Copenhageni (rats) [7,9]. The organism is sensitive to common disinfectants and antiseptic, and easily killed at 60°C in 10 seconds. The case fatality range from 3 to over 50% [WHO, 2003].
Transmission
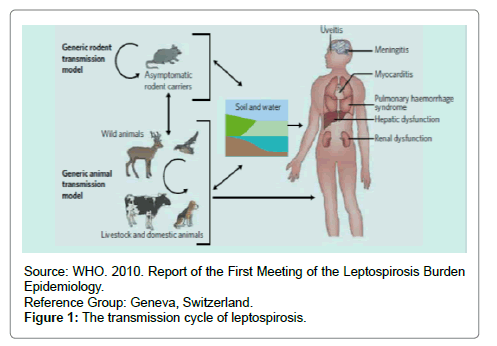
Rodents play an important role in the transmission of leptospirosis. Animals shed the organisms in their urine for long periods. However, lifelong renal carrier state is observed in rodents [2]. Carrier animals may excrete up to 100 million leptospires in the urine. Water, soil, and food contaminated by urine of carriers/ infected animals are the major sources of human infection (Figure 1). Humans can acquire infection through various routes. The common mode of transmission is exposure to and ingestion of urine contaminated water [1]. High rainfall and warm climatic conditions provide suitable environment for the survival of Leptospira and when humans come into contact with such water, the organisms enter the body through abraded skin or mucosa of eye, nose and throat and initiate the infection. Over flooding of water during rainy season creates an ideal environment for the transmission of Leptospira. The exposure of swimmers to water contaminated by the urine of rodents and dogs can lead to serious outbreaks of leptospirosis. Ingestion of urine contaminated foods can also result in the infection [2]. Veterinarians become infected by handling the urine and tissues of infected animals. Infections of abattoir workers occur through contact with infected blood and body fluids of animals [1,2].
Clinical Spectrum
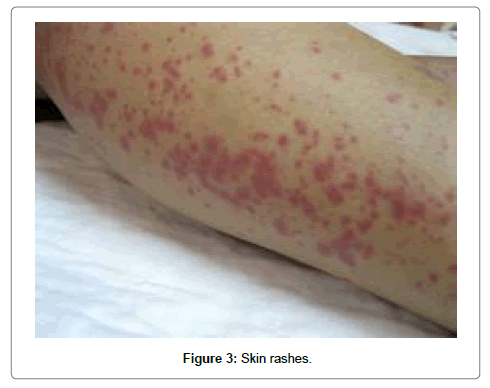
The incubation period of leptospirosis is 7-14 days. Clinical manifestations comprise fever, chills, rigors, severe headache, muscle aches, jaundice (Figure 1), anorexia, conjunctival suffusion (Figure 2a), arthralgia, myalgia, vomiting, diarrhea, abdominal pain, photophobia, red eye (Figures 2b and 2c), mucosal rash, skin rash (Figure 3), cough, breathlessness, chest pain, haemoptysis, anuria, oliguria, hypotension, cough, bradycardia, stiff neck, delirium, meningitis, splenomegaly, lymphadenopathy, and hepatomegaly [1,2,6,10].
Death can occur due to serious organ and vital system dysfunctions mainly kidney failure and pulmonary hemorrhage [2]. The extent of damage is dependent on the virulence of the organism and host susceptibility evidenced by laboratory findings which showed significant differences in hemoglobin concentration, blood cell counts and concentrations of protein in mild and severe conditions [11,19].
Epidemiology
Leptospirosis has a complex epidemiology as many animals serve as reservoir of infection. The annual burden of leptospirosis is largely underestimated because of inadequate surveillance. Globally, leptospirosis is estimated to cause 1.03 million cases and 58,900 deaths [3]. Disease is recorded in both sexes with predominance in young adult males, and in urban and rural settings. It is an important occupational zoonosis of agriculture workers, sewer workers, mine workers, slaughterhouse employees, butchers, dairy farmers, veterinarians, animal handlers, kennel attendants, sanitary workers, construction workers, military personnel’s and fishermen [2]. Travelers are exposed to leptospirosis through activities involving contact with water, soil, and animals. Many animals including pets, farm animals, or wildlife can spread the disease. There is always a risk of infection for people who have contact with infected animals or soil/water where the organisms are present. People who work outdoors or with animals may be at increased risk for infection. In addition, those involved in outdoor freshwater activities such as swimming, rafting and kayaking may also face an increased risk [18].
A plethora of factors such as rain fall, humidity, ambient temperature, pH, surface water, soil salinity, and forest cover influence the survival of organisms. Leptospires prefer fresh water to survive for several months in running water but has also a possibility to survive for several weeks in stagnant water and some halophilic strains may be recovered from brackish and salt water [11,12-14]. Recently, two strains of Leptospira kmetyi (MS432 and MS422) were shown to survive for 3 days in both artificial and natural seawater and for four days when mixed with soil. This finding warns of the possible risks of the leptospiral infections in areas prone to ocean storm surges or tsunami [18].
High rainfall and warm climatic conditions provide optimal environments for the survival of organisms in which peoples from developing countries are at higher risk. Most communities in such areas collect water from natural water bodies such as rivers, streams, or underground aquifers, and then store this water for long periods of time in a reservoir. It is globally being recorded as an epidemic threat in developing countries in and around the rainy season. In urban setting, flooding of roads during heavy rains expose the persons to Leptospira infection. However, in rural areas, farmers working in rice fields are at high risk of acquiring infection. The annual incidence of this disease is estimated at 10 to 100 per 100,000 in tropical regions and 0.1–1.0 per 100,000 in temperate areas [18].
Diagnosis
The clinical diagnosis of leptospirosis must be supported by a variety of laboratory tests such as microbiological, immunological, and molecular techniques [1,19]. Examination of freshly voided urine by dark field microscopy for pathogen, direct demonstration of leptospires in clinical specimens with Giemsa, silver impregnation and immune peroxidase methods, detection of serum antibodies against Leptospira by microscopic agglutination test (MAT), IgM enzyme linked immunosorbent assay (ELISA) and LEPTO dipstick, isolation of leptospires from blood within the first 7 days of an acute infection, from cerebrospinal fluid between the forth and tenth day of an infection and from urine after the 10th day on several media such as EMJH medium, Fletcher’s medium, Korthop’s medium, Stuart’s medium are helful to confirm an unequivocal diagnosis of disease [1,2,7]. Very recently, molecular based tool such as PCR, RFLP can be tried in the diagnosis of leptospirosis [9]. Direct demonstration of the organism in urine by dark field microscopy is the simplest method to diagnose leptospirosis [2].
Currently, it is difficult to detect pathogenic Leptospira in water samples due to filtering problems with the volume of the sample water and leptospiral concentration in the sample and the number of other potential bacteria present in water samples, which can contaminate culture media [18]. There is an acute need to develop simple, easy, sensitive, specific and low cost technique that can be routinely employed by poor resource countries to diagnose leptospirosis in humans and animals.
Leptospirosis is a protean disease and hence should be differentiated from dengue fever, malaria, yellow fever, influenza pneumonia, typhoid fever, hepatitis, borreliosis, and brucellosis [20].
Treatment
Basically, early treatment with antibiotics may reduce mortality, clinical impacts, and leptospiruria rate when compared to placebo, although very few studies are available to provide clear guidelines for treatment of disease [21]. A number of antibiotics such as ampicillin, cefotaxime, ceftriaxone, chlorampheicol, doxcycline, erythromycin, and streptomycin can be given in less severe cases, however, for severe cases, penicillin is considered as drug of choice [7]. It is important to mention that therapy should be started as soon as the diagnosis of disease is confirmed to have good prognosis [22]. Dihydostrptomycin is recommended to eliminate the organisms in the carrier animals [1]. It is emphasized to develop a safe, potent, and cheap vaccine, which can be widely used to protect the susceptible population especially of endemic regions.
Prevention and Control
The complete elimination of disease seems unfeasible as many species of rodents serve as reservoir of infection. Hence, proper strategies for prevention of leptospirosis are based on awareness of leptospirosis epidemiology and transmission mechanisms. It is possible to prevent the disease by reducing exposure and implement protective measures, immunization, and pre- or post-exposure chemoprophylaxis. Housing construction that prevents entry of rodents from invading residential living areas and water sources greatly reduces risk of infection. Swimming in contaminated water, and walking barefoot in flood water should be avoided [1]. Flood control projects and avoiding water supply contamination by animals would greatly reduce the potential for the outbreaks of leptospirosis [1,2,18,19].
Occupational activities that put workers at risk through exposure to contaminated water or infected animals should be identified. Personal protective equipment such as gloves, boots, goggles, and overalls for workers in high-risk occupations are important to prevent exposure of infection. Source reduction through immunization of agricultural and companion animals with killed whole-cell vaccines is an extremely important strategy for reducing the risk of human leptospirosis. Diagnosis and treatment of infected animals and immunization of uninfected companion and agricultural animals is a critical measure for leptospirosis prevention. In addition, immunization of humans with killed, whole-cell vaccines can be done restricted to individuals in high-risk occupations including tourists and in response to floods and epidemics [1,19]. It is advised to impart health education of various occupational groups about the source of infection, mode of transmission, severity of disease, and environmental hygiene [1]. Emphasis is laid to identify the contaminated water bodies so that public can be informed not to visit such sites.
Conclusion
Currently, leptospirosis has been recognized as a major public health problem, especially in developing nations of the world. It can lead to potentially fatal infections of the kidney, liver, brain, lung or heart. Many domestic and wild animals are responsible for the transmission of the disease to humans. The disease is considered as occupational hazard of the persons whose daily activities are associated with animals and their products and agricultural practices using contaminated water sources. Epidemic of leptospirosis occurs following migration of rats into urban areas during flood. It is imperative to confirm an unequivocal diagnosis of disease by employing standard laboratory techniques. As severe hemorrhagic pulmonary syndrome carries high mortality of above 74%, emphasis is given on early diagnosis and prompt therapy to prevent the fatal consequences. Chemoprophylaxis with doxycycline is recommended in high risk groups in endemic areas. There is a need to undertake detailed epidemiological studies in humans and animals so that proper strategies can be planned to control leptospirosis, which has emerged as an important life threatening direct anthropozoonosis.
Acknowledgements
We are very grateful to Prof.Dr R.K.Narayan for critically reviewing our manuscript. Thanks are due to Anubha for her excellent computer help. Acknowledgement is also given to authors of various papers from whom the materials are taken as reference for the preparation of this manuscript.
References
- Pal M (2007) Zoonoses (2ndedn). Satyam Publishers, Jaipur, India.
- Pal M (1996) Leptospirosis: A contemporary zoonosis. The Veterinarian 20: 11-12.
- Costa F, Hagen JE, Calgano J, Kane M, Torgerson P,etal. (2015) Global morbidity and mortality of leptospirosis: A systematic review.PloSNegl Tropical Disease 9: e0003898.
- Akhilanand C (2016)Leptospirosis-An indian experience. Air and Water Borne Diseases 5:S1.
- Kmety E,Dikken H (1993) Classification of the species Leptospirainterrogans and the history of its serovars. University Press Groningen, Groningen.
- Devishree RA (2015) Management of leptospirosis: A short review. Journal of PharmaciticalScience and Research 7:759-761.
- Heymann D (2004) Control of communicable diseases manual. American Public Health Association. KIT Biomedical Research, pp: 306-309.
- Levett P (2005) Leptospirosis. In: G Mandell, J Bennett, R Dolin (eds.). Principles and Practice of Infectious Diseases.
- Deanna H (2006)Leptospirosis: A waterborne zoonotic disease of global importance. Georgia Epidemiology Report 22: 8.
- Levett PN (2001) Leptospirosis. ClinMicrobiol Rev 14: 296-326.
- Faine S, Adler B, Bolin C,Perolat P (1999) Leptospira and Leptospirosis (2nd edn). Medical Science, Melbourne. pp: 17–166.
- Cacciapuoti B, Ciceroni L,Maffei C, Di Stanislao, F CalegariL,et al. (1987) A waterborne outbreak of leptospirosis. Am J Epidemiol 126: 535-545.
- Wynwood SJ, Craig SB, Graham GC, Blair BR, Burns MA,et al. (2014) The emergence of LeptospiraborgpeterseniiserovarArborea as the dominant infecting serovar following the summer of natural disasters in Queensland, Australia 2011. Trop Biomed 31:281-285.
- Morgan J, Bornstein SL,Karpati AM, Bruce M, Bolin CA, et al. (2002) Outbreak of leptospirosis among triathlon participants and community residents in Springfield, Illinois, 1998. Clin Infect Dis 34:1593-1599.
- Trueba G, Zapata S, Madrid K, Cullen P,Haake D (2004) Cell aggregation: A mechanism of pathogenic Leptospira to survive in fresh water. International Microbiology 7: 35-40.
- Smith DJ, Self HR (1955) Observations on the survival of LeptospiraaustralisA in soil and water. J Hyg 53: 436–444.
- Khairani-Bejo S, Bahaman AR,Zamri-Saad M,Mutalib AR (2004) The survival of LeptospirainterrogansSerovarHardjo in the Malaysian environment. J Anim Vet Adv 3:123-129.
- Sarah JW, Glenn CG, Steven LW,Trudi AC, David BM,et al. (2014) Leptospirosis from water sources. Pathog Glob Health 108:335-338.
- Craig SB, Graham GC, Burns MA,Dohnt MF,Smythe LD,et al. (2009) Haematological and clinical-chemistry markers in patients presenting with leptospirosis: A comparison of the findings from uncomplicated cases with those seen in the severe disease. Annual Tropical Medicine and Parasitology 103: 333-341.
- W.H.O (2003) Human Leptospirosis: Guidance for diagnosis, surveillance and control. World Health Organization and International Leptospirosis Society, WHO library Cataloguing-in Publication Data, Malta.
- Guidugli F, Castro AA,Atallah AN(2006)Antibiotics for leptospirosis. The Cochrane Database of Systematic Reviews.
- David AH,Paul NL(2015) Leptospirosis in humans. Curr Top MicrobiolImmunol 387: 65-97.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 11691
- [From(publication date):
March-2017 - Apr 17, 2025] - Breakdown by view type
- HTML page views : 10528
- PDF downloads : 1163