Leclercia adecarboxylata, An Emerging Pathogen: A Narrative Review
Received: 30-Oct-2023 / Manuscript No. JIDT-23-118830 / Editor assigned: 02-Nov-2023 / PreQC No. JIDT-23-118830(PQ) / Reviewed: 16-Oct-2023 / QC No. JIDT-23-118830 / Revised: 23-Nov-2023 / Manuscript No. JIDT-23-118830(R) / Published Date: 30-Dec-2023 DOI: 10.4172/2332-0877.1000573
Abstract
Leclercia adecarboxylata is a gram negative, motile, facultative-anaerobic, oxidase-negative, mesophilic bacillus belonging to the Enterobacteriaceae family. L. adecarboxylatawas first described by H. Leclerc in 1962, and previously known as “Enteric group 410” or “Escherichia adecarboxylata”, since Leclercia spp. shares several structural and microbiological properties with the genus Escherichia. Due to those similarities, L. adecarboxylatainfections might be more common than what believed so far, since past clinical cases might have been erroneously defined as Escherichia spp. infections. L. adecarboxylatais a member of the normal gut flora in animals, has been isolated from water, food, and other environmental sources, can be found in a variety of specimens and is involved in a wide range of clinical syndromes commonly related to immunocompromised hosts. Although most of Leclercia spp isolates show high susceptibility to antibiotics, some multi-resistant strains have been reported in literature. Here, we narratively review the most original and relevant articles available in literature to provide a state of art to the current knowledge of this emerging pathogen.
Keywords: Leclercia adecarboxylata; Emerging pathogen; Infection; Treatment; Resistance; Multi-drug resistant
Introduction
Leclercia adecarboxylata is a gram-negative bacillus firstly described by H. Leclerc in 1962, and previously known as “Enteric group 410” or “Escherichia adecarboxylata” [1], since Leclercia spp. shares a lot of structural and microbiological characteristics with the genus Escherichia. Due to those similarities, L. adecarboxylatainfections might be more common than what believed so far since past clinical cases might have been erroneously defined as Escherichia spp. infections. Moreover, most bacterial assays often could not distinguish these morphologically and metabolically similar bacteria [2,3]. In present days, the availability of more sensitive testing methods (e.g.: DNA hybridization, computer identification studies) like Matrix Assisted Laser Desorption/Ionization Time of Flight (“MALDI-TOF”) mass spectrometry allowed a more precise species identification, eventually leading to the present categorization [4]. Given this increasing number of accurate identifications, L. adecarboxylatahas been recently recognized as an emerging bacterium [4].
Hence, we decided to review the most original and relevant articles available in the literature to provide a state of art to the current knowledge of this emerging pathogen.
Literature Review
References for this review were identified from PubMed, Embase, and Cochrane with the following research term combination: “Leclercia adecarboxylata” OR “Leclercia” OR “Leclercia infection”. Only papers in English were included. The final reference list was generated based on timeline, originality, and relevance to the scope of this Review.
Etiology and microbiology
Leclercia adecarboxylata is a gram-negative, motile, facultative- anaerobic, oxidase-negative, mesophilic bacillus belonging to the Enterobacteriaceae family [4]. It shares many structural and microbiological properties with the genus Escherichia [1,4], but, thanks to more sensitive testing methods such as DNA hybridization and computer identification studies, a reclassification of this bacteria was achieved [4]. However, L. adecarboxylataand Escherichia also harbor some differences: in particular, unlike Escherichia strains, Leclercia might occasionally test positive for urease hydrolysis and differ for malonate utilization and production of yellow pigment; they also grow in the presence of potassium cyanide and, unlike Escherichia, resulting negative to lysine and ornithine decarboxylase tests [5].
Given its low virulence, L. adecarboxylatararely causes monomicrobial infection, mostly in immunocompromised patients, while it is thought that this pathogen generally requires other coinfecting microorganisms to establish infection in immunocompetent subjects [2]. In the setting of polymicrobial infections, the most co-pathogens found are Enterococci, Acinetobacter, Pseudomonas aeruginosa, Klebsiella, Fusarium and Staphylococcus epidermidis [3,6]. Some cases of monomicrobial infection were also described in immunocompetent patients even without significant underlying comorbidities: particularly, only in one case the patient reported a clinical history of chronic diseases [7], while in the other cases no medical history was observed [8-10].
Leclercia adecarboxylata shows generally high susceptibility to antibiotics, however, some Multidrug-Resistant (MDR) strains have been widely described even in local outbreaks [2,6,11-13]. Particularly, specimens harbouring blaTEM-1 and blaCTX-M group 1 and intl1 genes (dfrA12-orfF-aadA2) as genetic determinants for resistance might become difficult-to-treat pathogens [11].
Epidemiology
L. adecarboxylata is a ubiquitous microorganism, which may be found in both aquatic environments and soil, as well as in the commensal gut flora of certain animals [1]. Asymptomatic carriage or colonization in healthy individuals is also described, rising concerns in regards to the spreading of the infection to immunocompromised people [14].
Prolonged antibiotic therapies, invasive interventions to the gastrointestinal tract, concomitant use of immunomodulators and the simultaneous presence of vascular graft or hemodialysis catheter could represent a risk factor for developing L. adecarboxylatainfections.
Indeed, several articles associate L. adecarboxylatawith haematological malignancies, solid cancer in general, or immunomodulator therapy. Moreover, several other underlying conditions might favor L. adecarboxylatainfections: for instance, wounds may be represented an access into the tissue, thus easing the pathogenicity as well as catheters in catheter-related bacteraemia or peritonitis could be developed in patients undergoing dialysis or chemotherapy [2]. A recent L. adecarboxylataoutbreak was reported in 25 patients receiving total parenteral nutrition (TPN): this pathogen was isolated after an extensive epidemiological investigation in one sealed, unopened bottle of TPN belonging to the same batch administered to all patients [12].
Clinical manifestations and diagnosis
L. adecarboxylata is implicated in several clinical syndromes, such as endocarditis [4,15,16], bacteraemia [2,7], wound infection and cellulitis [10,17,18], pharyngeal and peritonsillar abscesses [9], urinary tract infections [19], pneumonia [20] and peritonitis [21,22]. Cases of keratitis with corneal abscess from L. adecarboxylatainfection have also been reported in patients with a history of exposure to the aquatic environment [17]. Most of the cases described regards immunocompromised adults, however, wound infections and peritonitis were reported even in immunocompetent children [18,21]. Two cases of pediatric septic arthritis of the knee caused by L. adecarboxylata, following an injury with residual foreign bodies, were reported in otherwise healthy Australian children without any significant pre-existing condition [23].
Other common clinical presentations are catheter-associated urinary tract infections in males, with translocation through the genitourinary tract, ventilator-associated pneumonia, peritonitis and vascular graft infections. Bacteremia can also occur after translocation across the intestinal mucosal barrier, in the setting of megacolon, prolonged antibiotic therapies or mucosal alterations due to invasive interventions to the gastrointestinal tract [2,14,24]. As reported before, most infections have been linked to immunosuppression, but also to the simultaneous presence of central vascular catheter [7] as it appears from several reports, catheters could be considered as important reservoirs for L. adecarboxylatabloodstream infection regardless of the patients’ immune status [6,11,25]. In light of this, Dotis, et al., recently conducted a systematic review of the case reports in international literature, identifying 13 cases of peritonitis in patients with peritoneal dialysis. All the patients included had a favourable outcome and showed a good response to the antibiotic therapy [26].
Currently, considering the wide distribution and use of MALDI- TOF, the diagnosis of a L. adecarboxylatainfection does not require any significant clinical or microbiological efforts. This pathogen might be isolated also from several biological specimens, such as blood culture, wound pus, faeces, urine, gallbladder, peri-ciliary and ciliary abscesses, synovial fluid, peritoneal fluid from peritoneal dialysis, sputum, cerebrospinal fluid, catheters, skin wounds, peritoneal fluid and abscesses (e.g.: peritonsillar and periovarian) [7].
Treatment
The isolates more commonly mentioned in literature usually show a high susceptibility to antibiotics [2,3] and might be controlled with a variety of antibiotics, such as beta-lactams, witnessing therapeutic to therapeutic failures or needing second line treatments. [11]. A more comprehensive evaluation regarding natural antimicrobial susceptibility patterns was reported by Stock et al from 94 L. adecarboxylatastrains, collected from several human specimens: the bacteria were naturally resistant to numerous antibiotic molecules, such as oxacillin, clarithromycin, erythromycin, roxithromycin, ketolides, rifampin, glycopeptides, streptogramins, fusidic acid, lincosamides, penicillin G, and fosfomycin but susceptible to most beta-lactams, quinolones, aminoglycosides, tetracyclines, nitrofurantoin folate pathway inhibitors, azithromycin and chloramphenicol.
However, some multi-resistant strains have been reported in the literature. Recently a case of Catheter-Related Bloodstream Infection (CRBSI) was described in a patient affected by gastric and duodenal diffuse large B-cell lymphoma with TPN through a tunneled central venous catheter. A multi-drug resistant L. adecarboxylatawas isolated from either peripheral and CVC blood culture, with an antibiogram showing full resistance to amoxicillin/clavulanate, fosfomycin, and trimethoprim-sulfamethoxazole [13]. In addition, Extended-Spectrum Beta-Lactamase (ESBL), New Delhi Metallo-Beta-Lactamase 1 (NDM)-producing and carbapenem-resistant L. adecarboxylataare also described. Three cases of ESBL producer isolates were in fact reported: the first case was described from a patient with acute myeloid leukaemia [27], the second in a 47-year-old female with breast cancer [11] and the third one in a 50-year-old female with end-stage renal disease [6]. In relation to NDM-producing L. adecarboxylata, two cases were reported: the first regarding a patient hospitalized for a foot trauma-related injury [28] while the second concerned an outbreak of 25 patients in intravenous TPN [12]. Regarding carbapenem-resistant L. adecarboxylatastrain, one case was reported from a healthy newborn in China, with a resistance pattern to both meropenem and ertapenem [29]. However, as only case reports and case series report resistant L. adecarboxylatastrains, it is impossible to infer whether risk factors are implicated in this concerning process.
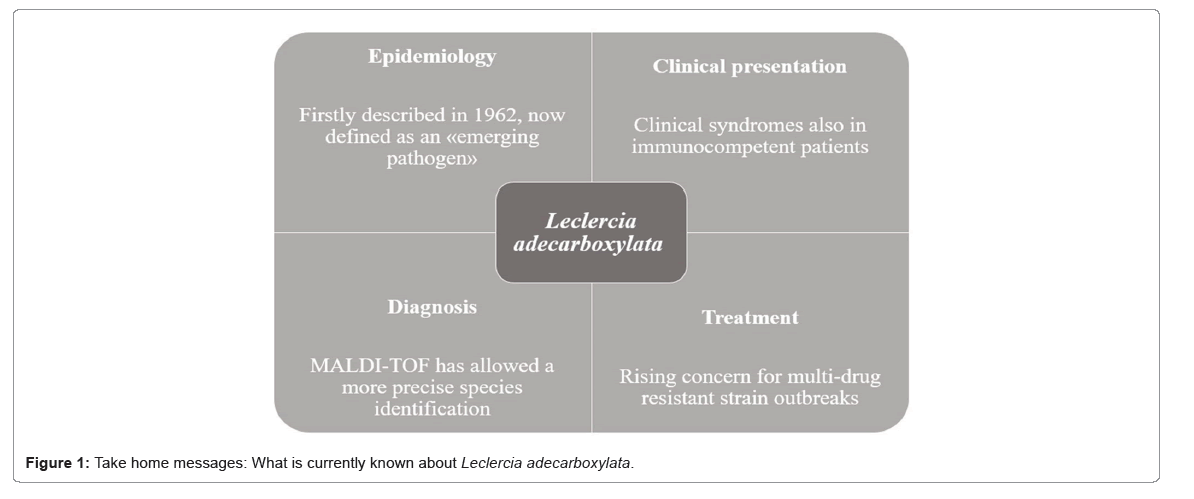
Regarding treatment options, there are no shared guidelines nor any recommendation for L. adecarboxylatainfections. Most isolates described are sensitive towards most of all tested antibiotics [2]. However, as described by Spiegelhauer et al., several strains of L. adecarboxylatadisplayed resistance to ampicillin (9/30 isolates resistant) and inherent resistance to fosfomycin, unlike other Enterobacteriaceae (8/10 isolates resistant) [30], so these antibiotics should not be used as the first line for treatment. Stock et al. described the natural susceptibility patterns of L. adecarboxylata, showing that most of the isolated strains were sensible to beta-lactams suggesting that Leclercia could be treated with this antibiotic class [11]. Lastly, in regards to infection where a graft is present (e.g. Tenckhoff or vascular catheter), a strict recommendation to remove the catheter is uncertain; although some evidence suggests that removal was necessary to achieve therapeutic success [31], the ability of L. adecarboxylatato produce biofilm remains unknown, even if the role of L. adecarboxylatain catheter-related bloodstream infections is increasing (Figure 1) [2].
Discussion
Infections caused by L. adecarboxylatahave likely been underestimated for decades due to the difficulty in identifying the microorganism, leading to underreporting in the medical literature [29,32-40]. An electronic search was employed to find the published articles which reported L. adecarboxylatainfections throughout the United States National Library of Medicine, PubMed (last accessed October 2023). All prospective studies, retrospective studies, case series, or case reports published in peer-reviewed medical journals, regarding the search topic were included. We excluded articles published in non-English languages, pre-print or ahead of print analysis, pre- clinical studies (including in vitro or animal model studies), short communications, letters to the editor, and commentaries. Our findings are summarized in Table 1.
| First author | Year | Type of study | Number of patients | Age | Immunestatus | Type of infection | Resistance spectrum |
|---|---|---|---|---|---|---|---|
| Spiegelhauer MR [2] | 2019 | Case report | 1 | Adult | Immunocompromised | Pneumonia | Monoresistance [TMP/SMX] |
| Forrester JD [32] | 2012 | Case report | 1 | Adult | Immunocompetent | CRBSI | No resistance detected |
| Hurley EH [18] | 2013 | Case report | 1 | Pediatric | Immunocompetent | BSI | NA |
| Temesgen Z [33] | 1997 | Case series | 5 | Adult | Immunocompetent (4), immunocompromised (1) | ABSSSI (3), BSI (1), Pneumonia (1) | No resistance detected (3), NA (2) |
| Savage PM [34] | 2023 | Case report | 1 | Adult | Immunocompetent | ABSSSI | NA |
| Shaikhain T [7] | 2021 | Case report | 1 | Adult | Immunocompetent | BSI | No resistance detected |
| De Mauri A [25] | 2013 | Case report | 1 | Adult | Immunocompromised | CRBSI | No resistance detected |
| Keyes J [35] | 2020 | Case series | 2 | Pediatric | Immunocompetent (1), Immunocompromised (1) | ABSSSI (1), UTI (1) | No resistance detected (1) Monoresistance [ampicillin] (1) |
| Myers KA [36] | 2011 | Case report | 1 | Pediatric | Immunocompetent | BSI | No resistance detected |
| Harper H [37] | 2022 | Case report | 1 | Adult | Immunocompromised | CRBSI | NA |
| Bronte Anaut M [38] | 2022 | Case report | 1 | Pediatric | Immunocompetent | BSI | No resistance detected |
| Aarab A [39] | 2021 | Case report | 1 | Pediatric | Immunocompetent | BSI | ESBL-producer |
| Matsuura H [40] | 2018 | Case report | 1 | Adult | Immunocompent | BSI | No resistance detected |
| Tan R [41] | 2022 | Case report | 1 | Adult | Immunocompetent | IE | No resistance detected |
| Sethi K [42] | 2013 | Case report | 1 | Pediatric | Immunocompetent | BSI | No resistance detected |
| Mayfield CK [43] | 2019 | Case report | 1 | Adult | Immunocompetent | ABSSSI | No resistance detected |
| Grantham WJ [44] | 2015 | Case report | 1 | Pediatric | Immunocompetent | ABSSSI | No resistance detected |
| Malik K [4] | 2021 | Case report | 1 | Adult | Immunocompetent | IE | No resistance detected |
| Kaushik M [45] | 2020 | Case report | 1 | Adult | Immunocompetent | ABSSSI | Monoresistance [ampicillin] |
| Li J [46] | 2021 | Case report | 1 | Adult | Immunocompetent | UTI | No resistance detected |
| Anuradha M [8] | 2014 | Case reports | 2 | Adult | Immunocompetent | ABSSSI (1) Vaginosis (1) | No resistance detected (1), Monoresistance [fosfomycin] (1) |
| Jean SS [47] | 2013 | Case report | 1 | Adult | Immunocompetent | BSI | No resistance detected |
| Kashani A [24] | 2014 | Case report | 1 | Adult | Immunocompetent | BSI | No resistance detected |
| Arasu R [48] | 2022 | Case series | 2 | Pediatric | Immunocompetent | Septic arthritis (1) | No resistance detected (1), Monoresistance [cefazolin] (1) |
| Lonneman MK [49] | 2020 | Case report | 1 | Adult | Immunocompetent | ABSSSI | No resistance detected |
| Adapa S [50] | 2019 | Case report | 1 | Adult | Immunocompromised | Abdominal infection | No resistance detected |
| Hess B [10] | 2008 | Case report | 1 | Adult | Immunocompetent | ABSSSI | No resistance detected |
| Garza-González E [12] | 2021 | Case series | 25 | Adult | NA | BSI | NDM-1-producer |
| Broderick A [17] | 2019 | Case report | 1 | Adult | Immunocompetent | ABSSSI | No resistance detected |
| Merza N [51] | 2019 | Case report | 1 | Adult | Immunocompetent | BSI | No resistance detected |
| Hassan I [52] | 2020 | Case report | 1 | Pediatric | Immunocompetent | SBP | No resistance detected |
| Gómez-Arroyo B [53] | 2020 | Case report | 1 | Adult | Immunocompetent | PJI | NA |
| Householder NA [54] | 2022 | Case report | 1 | Adult | Immunocompetent | Arthritis | No resistance detected |
| Alosaimi RS [6] | 2020 | Case report | 1 | Adult | Immunocompromised | CRBSI | ESBL-producer |
| Voulalas G [55] | 2016 | Case report | 1 | Adult | Immunocompetent | Mycotic aneurysm | No resistance detected |
| Nelson MU [56] | 2013 | Case report | 1 | Pediatric | Immunocompetent | BSI | No resistance detected |
| Sanchez Porto A [57] | 2014 | Case report | 1 | Adult | Immunocompromised | BSI | No resistance detected |
| Colangelo C [13] | 2023 | Case report | 1 | Adult | Immunocompromised | CRBSI | Multi-drug resistance [amoxicillin, fosfomycin, TMP/SMX] |
| Atas DB [58] | 2017 | Case report | 1 | Adult | Immunocompromised | Abdominal infection | NA |
| Marina VP [59] | 2011 | Case report | 1 | Adult | Immunocompromised | CRBSI | No resistance detected |
| Shah A [60] | 2011 | Case report | 1 | Pediatric | Immunocompromised | ABSSSI | No resistance detected |
| Eiland EH [61] | 2013 | Case report | 1 | Adult | Immunocompetent | Pneumonia | Multi-drug resistance [ampicillin, gentamycin, TMP/SMX] |
| Michael Z [62] | 2013 | Case report | 1 | Adult | Immunocompetent | ABSSSI | Penicillinase-procucer |
| Papacharalampous G [63] | 2015 | Case report | 1 | Adult | Immunocompetent | Mycotic aneurysm | No resistance detected |
| Jover-Sáenz A [64] | 2008 | Case report | 1 | Adult | Immunocompetent | Abdominal infection | No resistance detected |
| Keren Y [65] | 2014 | Case report | 1 | Adult | Immunocompetent | ABSSSI | No resistance detected |
| Haji S [66] | 2014 | Case report | 1 | Adult | Immunocompetent | BSI | No resistance detected |
| Allawh R [67] | 2015 | Case report | 1 | Adult | Immunocompetent | ABSSSI | No resistance detected |
| Fattal O [68] | 2000 | Case report | 1 | Pediatric | Immunocompromised | Abdominal infection | No resistance detected |
| de Baere T [69] | 2001 | Case series | 2 | Adult | Immunocompetent | Abdominal infection (1), BSI (1) | No resistance detected (1), Monoressitance [ampicillin] (1) |
| Tam V [70] | 2012 | Case report | 1 | Adult | Immunocompetent | ABSSSI | No resistance detected |
| Riazzo C [28] | 2017 | Case report | 1 | Adult | Immunocompetent | ABSSSI | NDM-1 producer |
| Bali R [9] | 2013 | Case report | 1 | Adult | Immunocompetent | ABSSSI | No resistance detected |
| Prakash MR [71] | 2015 | Case series | 3 | Adult | Immunocompetent (2), immunocompromised (1) | Pneumonia | No resistance detected (2), Monoressitance [ampicillin] (1) |
| Lee B [72] | 2009 | Case report | 1 | Adult | Immunocompetent | IE | No resistance detected |
| Chao CT [73] | 2014 | Case report | 1 | Adult | Immunocompromised | Peritonitis | No resistance detected |
| Longhurst CA [74] | 2001 | Case report | 1 | Pediatric | Immunocompromised | BSI | No resistance detected |
| García-Fulgueiras V [75] | 2014 | Case report | 1 | Adult | Immunocompetent | Osteomyelitis | Penicillinase-producer |
| Dalamaga M [76] | 2008 | Case report | 1 | Adult | Immunocompetent | BSI | Multi-drug ressitant [ampicillin, tobramycin, TMP/SMX] |
| Shin GW [11] | 2012 | Case report | 1 | Adult | Immunocompromised | CRBSI | Multi-drug ressitant [penicillins and cephalosporines, tobramycin, TMP/SMX] |
| Kim HM [77] | 2008 | Case report | 1 | Adult | Immunocompromised | Abdominal infection | Monoresistance [ampicillin] |
| Fernández-Ruiz M [78] | 2009 | Case series | 2 | Adult | Immunocompromised | CRBSI | No resistance detected |
| Mazzariol A [79] | 2003 | Case report | 1 | Adult | Immunocompromised | BSI | ESBL-producer |
| Sawamura H [80] | 2005 | Case report | 1 | Adult | Immunocompetent | Pyelonephritis | No resistance detected |
Note: CRBSI: Catheter-Related Bloodstream Infection; BSI: Bloodstream Infection; ABSSSI: Acute Bacterial Skin and Skin Structure Infection; IE: Infective Endocarditis; UTI: Urinary Tract Infection; TMP/SMX: Cotrimoxazole; ESBL: Extended-Spectrum Beta-Lactamase; NDM: New Delhi Metallo-Beta-Lactamase; VIM: Verona Integron–Encoded Metallo-Beta-Lactamase; NA: Not Available.
A total of 160 papers were identified through our search, but, eventually, only 64 were included as describing a clinical case of L. adecarboxylatainfection. While 99 patients were affected by a generally multi-sensible L. adecarboxylatainfection, the number of multi-drug resistant strain is rising over time [41-62]. Among the documented cases of pediatric infection, even a colonization of a carbapenem- resistant L. adecarboxylataisolated from a healthy newborn has been reported in 2023 [29,63-70]. All things considered; it is hard and incorrect to define L. adecarboxylataas an “opportunistic pathogen” as often happen in literature [71-80], even if most of the infections occur in immunocompromised hosts.
Carbapenems are always considered when treating a multidrug- resistant Gram-negative bacterial infection, but carbapenem-resistant Enterobacteriaceae have become a major public health threat, leading to severe infections, limited treatment options, and mortality rates of 26%- 44% [29]. As previously shown despite most cases of L. adecarboxylatainfection are susceptible to common antibiotics, some drug-resistant strains have recently been detected in literature [29]. Moreover, even animal studies raise concern on the emergence of resistant strain of L. adecarboxylataas suggested by a recent paper regarding a genomic investigation of a multiple fluoroquinolone-resistance from a diseased synanthropic pigeon [81,82].
Conclusion
L. adecarboxylata infections occur rarely in immunocompetent patients and the pathogen usually shows good sensibility patterns to most antimicrobial agents. However, severe infections from difficult-to- treat strains are increasing. Given the absence of specific guidelines on L. adecarboxylatamanagement and treatment, there is a need to create a multicentric international network sharing experiences to increase knowledge about this emerging pathogen.
Author Contributions
Conceptualization, E. F.; writing-original draft preparation, M.D.G., G.T., C.C., and E.F.; validation, M.D.G., G.T., C.C., and E.F.; investigation, M.D.G., G.T., C.C., and E.F.; data curation, M.D.G., G.T., C.C., and E.F.; writing-review & editing, M.D.G., G.T., C.C., S.C., F.C., A.C., F.C., and E.F.; visualization, M.D.G., G.T., C.C., S.C., F.C., A.C., F.C., and E.F.; supervision, A.C., F.C., and E.F. All authors have read and agreed to the published version of the manuscript.
Funding
None to declare, this research received no external funding or financial support
Transparency Declarations
None to declare, all authors have no competing interests.
References
- Zayet S, Lang S, Garnier P, Pierron A, Plantin J, et al. (2021) Leclercia adecarboxylata as emerging pathogen in human infections: clinical features and antimicrobial susceptibility testing. Pathogens 10:1399.
[Crossref] [Google Scholar] [PubMed]
- Spiegelhauer MR, Andersen PF, Frandsen TH, Nordestgaard RLM, Andersen LP (2019) Leclercia adecarboxylata: a case report and literature review of 74 cases demonstrating its pathogenicity in immunocompromised patients. Infect Dis (Lond) 51:179-188.
[Crossref] [Google Scholar] [PubMed]
- Gajdács M, Ábrók M, Lázár A, Terhes G, Burián K (2020) Leclercia adecarboxylata as an emerging pathogen in human infections: A 13-year retrospective analysis in Southern Hungary. J Infect Dev Ctries 14:1004-1010.
[Crossref] [Google Scholar] [PubMed]
- Malik K, Davie R, Withers A, Faisal M, Lawal F (2021) A case of Leclercia adecarboxylata endocarditis in a 62-year-old man. IDCases 24: e01091.
[Crossref] [Google Scholar] [PubMed]
- Feucherolles M, Cauchie HM, Penny C (2019) MALDI-TOF Mass spectrometry and specific biomarkers: Potential new key for swift identification of antimicrobial resistance in foodborne pathogens. Microorganisms 7:593.
[Crossref] [Google Scholar] [PubMed]
- Alosaimi RS, Muhmmed Kaaki M (2020) Catheter-related ESBL-producing Leclercia adecarboxylata septicemia in hemodialysis patient: an emerging pathogen? Case Rep Infect Dis 2020:7403152. doi: 10.1155/2020/7403152. PMID: 32089912; PMCID: PMC6996699.
[Crossref] [Google Scholar] [PubMed]
- Shaikhain T, Al-Husayni F, Al-Fawaz S, Alghamdi EM, Al-Amri A, et al. (2021) Leclercia adecarboxylata bacteremia without a focus in a non-immunosuppressed patient. Am J Case Rep 22:e929537.
[Crossref] [Google Scholar] [PubMed]
- Anuradha M (2014) Leclercia adecarboxylata isolation: case reports and review. J Clin Diagn Res 8:DD03-04.
[Crossref] [Google Scholar] [PubMed]
- Bali R, Sharma P, Gupta K, Nagrath S (2013) Pharyngeal and peritonsillar abscess due to Leclercia adecarboxylata in an immunocompetant patient. J Infect Dev Ctries 7:46-50.
[Crossref] [Google Scholar] [PubMed]
- Hess B, Burchett A, Huntington MK (2008) Leclercia adecarboxylata in an immunocompetent patient. J Med Microbiol 57:896-898.
[Crossref] [Google Scholar] [PubMed]
- Shin GW, You MJ, Lee HS, Lee CS (2012) Catheter-related bacteremia caused by multidrug-resistant Leclercia adecarboxylata in a patient with breast cancer. J Clin Microbiol 50:3129-3132.
[Crossref] [Google Scholar] [PubMed]
- Garza-González E, Bocanegra-Ibarias P, Rodríguez-Noriega E, González-Díaz E, SilvaSanchez J, et al. (2021) Molecular investigation of an outbreak associated with total parenteral nutrition contaminated with NDM-producing Leclercia adecarboxylata. BMC Infect Dis 21:235.
- Colangelo C, Tiecco G, Di Gregorio M, Capone S, Allegri RL, et al. (2023) A rare case of multidrug-resistant Leclercia adecarboxylata catheter-related bloodstream infection and an updated brief literature review. Mediterr J Hematol Infect Dis 15:e2023052.
[Crossref] [Google Scholar] [PubMed]
- Tan R, Yu JQ, Wang J, Zheng RQ (2022) Leclercia adecarboxylata infective endocarditis in a man with mitral stenosis: A case report and review of the literature. World J Clin Cases 10: 10670-10680.
[Crossref] [Google Scholar] [PubMed]
- Dudkiewicz B, Szewczyk E (1993) Etiology of bacterial endocarditis in materials from cardiology and cardiac surgery clinics of the Lodz Academy. Med Dosw Mikrobiol 45:357-359.
[Google Scholar] [PubMed]
- Lee B, Sir JJ, Park SW, Kwak CH, Kim SM, et al. (2009) A case of Leclercia adecarboxylata endocarditis in a woman with endometrial cancer. Am J Med Sci 337:146-147.
[Crossref] [Google Scholar] [PubMed]
- Broderick A, Lowe E, Xiao A, Ross R, Miller R (2019) Leclercia adecarboxylata folliculitis in a healthy swimmer-An emerging aquatic pathogen? JAAD Case Rep 5:706-708.
[Crossref] [Google Scholar] [PubMed]
- Hurley EH, Cohen E, Katarincic JA, Ohnmacht RK (2015) Leclercia adecarboxylata infection in an immunocompetent child. R I Med J (2013) 2015 98:41-44.
[Google Scholar] [PubMed]
- Li J, Park A, Fulmer BR, Garg T (2021) Leclercia adecarboxylata urinary tract infection in a patient with bladder cancer and recurrent hematuria. Urol Case Rep 36:101579.
[Crossref] [Google Scholar] [PubMed]
- Ravikumar R, Patra N, Indiradevi B (2015) Hospital-acquired pneumonia due to Leclercia adecarboxylata in a neurosurgical centre. J Postgrad Med 61:123-125.
[Crossref] [Google Scholar] [PubMed]
- Hassan I, Gupta P, Ray P, Tiewsoh K (2020) Leclercia adecarboxylata causing spontaneous bacterial peritonitis in a child with nephrotic syndrome: a case report and review of literature. J Lab Physicians 12: 222-224.
[Crossref] [Google Scholar] [PubMed]
- Adapa S, Konala VM, Nawaz F, Javed T, Dhingra H, et al. (2019) Peritonitis from Leclercia adecarboxylata: an emerging pathogen. Clin Case Rep 7:829-831.
[Crossref] [Google Scholar] [PubMed]
- Hobby G, Mandavilli K, Singh M (2017) A case report of Leclercia adecarboxylata peritonitis in a peritoneal dialysis patient with review of the literature. Int J Nephrol Kidney Fail 3:1-2.
[Crossref] [Google Scholar] [PubMed]
- Kashani A, Chitsazan M, Che K, Garrison RC (2014) Leclercia adecarboxylata bacteremia in a patient with ulcerative colitis. Case Rep Gastrointest Med 2014:457687.
[Crossref] [Google Scholar] [PubMed]
- de Mauri A, Chiarinotti D, Andreoni S, Molinari GL, Conti N, et al. (2013) Leclercia adecarboxylata and catheter-related bacteraemia: review of the literature and outcome with regard to catheters and patients. J Med Microbiol 2013 Oct;62(Pt 10):1620-1623.
[Crossref] [Google Scholar] [PubMed]
- Dotis J, Kondou A, Karava V, Sotiriou G, Papadopoulou A, et al. (2023) Leclercia adecarboxylata in peritoneal dialysis patients: a systematic review. Pediatr Rep 15:293-300.
[Crossref] [Google Scholar] [PubMed]
- Mazzariol A, Zuliani J, Fontana R, Cornaglia G (2003) Isolation from blood culture of a Leclercia adecarboxylata strain producing an SHV-12 extended-spectrum beta-lactamase. J Clin Microbiol 41:1738-1739.
[Crossref] [Google Scholar] [PubMed]
- Riazzo C, López-Cerero L, Rojo-Martín MD, Hoyos-Mallecot Y, Fernández-Cuenca F, et al. (2017) First report of NDM-1-producing clinical isolate of Leclercia adecarboxylata in Spain. Diagn Microbiol Infect Dis 88:268-270.
[Crossref] [Google Scholar] [PubMed]
- Meng S, Miao BB, Li J, Yin JW, Liu ZL, et al. (2023) Isolation of Leclercia adecarboxylata producing carbapenemases in a newborn female. Biomed Environ Sci 36:874-879.
[Crossref] [Google Scholar] [PubMed]
- Tamura K, Sakazaki R, Kosako Y, Yoshizaki E (1986) Leclercia adecarboxylata gen. nov., comb. nov., formerly known as escherichia adecarboxylata. Curr Microbiol 13:179-184.
- Ghosh R, Misra R, Prasad KN, Prasad N (2016) Peritonitis by Leclercia adecarboxylata in a patient with continuous ambulatory peritoneal dialysis: the first case report from India. Int J Res Med Sci 4:1254-1256.
- Forrester JD, Adams J, Sawyer RG (2012) Leclercia adecarboxylata bacteremia in a trauma patient: case report and review of the literature. Surg Infect (Larchmt) 13:63-66.
[Crossref] [Google Scholar] [PubMed]
- Temesgen Z, Toal DR, Cockerill FR (1997) Leclercia adecarboxylata infections: case report and review. Clin Infect Dis 25:79-81.
[Crossref] [Google Scholar] [PubMed]
- Savage PM, Savage TJ, Kruse DL, Stone PA (2023) Leclercia adecarboxylata and pseudomonas oryzihabitans infection after achilles tendon repair: a case report and literature review. J Foot Ankle Surg 62:742-745.
[Crossref] [Google Scholar] [PubMed]
- Keyes J, Johnson EP, Epelman M, Cadilla A, Ali S (2020) Leclercia adecarboxylata: an emerging pathogen among pediatric infections. Cureus 12:e8049.
[Crossref] [Google Scholar] [PubMed]
- Myers KA, Jeffery RM, Lodha A (2012) Late-onset Leclercia adecarboxylata bacteraemia in a premature infant in the NICU. Acta Paediatr 101:e37-9.
[Crossref] [Google Scholar] [PubMed]
- Harper H, Logan J, Kubat R, Jones M (2022) Leclercia adecarboxylata catheter-related bacteraemia in an immunocompromised patient. BMJ Case Rep 15:e247496.
[Crossref] [Google Scholar] [PubMed]
- Bronte Anaut M, Arredondo Montero J, García Abellás P, de Uribe Viloria M, Regojo Zapata RM (2022) Fulminant sepsis caused by Leclercia adecarboxylata in a premature neonate: case report and review of the literature. Pediatr Infect Dis J 41:e220-e222.
[Crossref] [Google Scholar] [PubMed]
- Aarab A, Saddari A, Noussaiba B, Ayyad A, Messaoudi S, et al. (2021) Leclercia adecarboxylata invasive infection in a patient with Hirschsprung disease: a case report. Ann Med Surg (Lond) 71:102927.
[Crossref] [Google Scholar] [PubMed]
- Matsuura H, Sugiyama S (2018) Sepsis and Leclercia adecarboxylata. QJM 111:733-734.
- Sethi K, Barker EM, Metlay LA, Caserta MT, Daugherty LE (2014) Leclercia adecarboxylata sepsis and cerebral herniation. J Pediatric Infect Dis Soc 3:e1-3.
[Crossref] [Google Scholar] [PubMed]
- Mayfield CK, Haglin JM, Konda SR, Tejwani NC, Egol KA (2019) Post-operative orthopedic infection with monomicrobial Leclercia adecarboxylata: a case report and review of the literature. JBJS Case Connect 9:e0297.
[Crossref] [Google Scholar] [PubMed]
- Grantham WJ, Funk SS, Schoenecker JG (2015) Leclercia adecarboxylata musculoskeletal infection in an immune competent pediatric patient: an emerging pathogen? Case Rep Orthop 2015:160473.
[Crossref] [Google Scholar] [PubMed]
- Kaushik M, Mittal A, Tirador K, Ibrahim H, Drake S (2020) Leclercia adecarboxylata causing necrotizing fasciitis in an immunocompetent athlete injecting illicit testosterone supplements. Cureus 12:e11196.
[Crossref] [Google Scholar] [PubMed]
- Li J, Park A, Fulmer BR, Garg T (2021) Leclercia adecarboxylata urinary tract infection in a patient with bladder cancer and recurrent hematuria. Urol Case Rep 36:101579.
[Crossref] [Google Scholar] [PubMed]
- Jean SS, Lee WS, Bai KJ, Lam C, Hsu CW, et al. (2016) Leclercia adecarboxylata bacteremia in a patient with long-term use of nonsteroidal anti-inflammatory drugs. J Microbiol Immunol Infect 49:452-454.
[Crossref] [Google Scholar] [PubMed]
- Arasu R, Ewe YH, Sundaram A, Foley DA, Campbell AJ, et al. (2022) Two cases of Leclercia adecarboxylata septic arthritis in immunocompetent paediatric patients. Access Microbiol 4:000325.
[Crossref] [Google Scholar] [PubMed]
- Lonneman MK, Devasahayam RJ, Phillips CJ (2020) Leclercia adecarboxylata causing necrotising soft tissue infection in an immunocompetent adult. BMJ Case Rep 13:e235633.
[Crossref] [Google Scholar] [PubMed]
- Adapa S, Konala VM, Nawaz F, Javed T, Dhingra H, et al. (2019) Peritonitis from Leclercia adecarboxylata: an emerging pathogen. Clin Case Rep 7:829-831.
[Crossref] [Google Scholar] [PubMed]
- Merza N, Lung J, Taha A, Qasim A, Frost J, et al. (2019) Leclercia adecarboxylata cholecystitis with septic shock in immunocompetent patient. Case Rep Crit Care 2019:5057071.
[Crossref] [Google Scholar] [PubMed]
- Hassan I, Gupta P, Ray P, Tiewsoh K (2020) Leclercia adecarboxylata causing spontaneous bacterial peritonitis in a child with nephrotic syndrome: a case report and review of literature. J Lab Physicians 12:222-224.
[Crossref] [Google Scholar] [PubMed]
- Gómez-Arroyo B, González-Donapetry P, Rico-Nieto A, Falces-Romero I (2020) Leclercia adecarboxylata isolates in a tertiary-care hospital: a propos of the first case of prosthetic joint infection. Enferm Infecc Microbiol Clin (Engl Ed) 38:503-505.
[Crossref] [Google Scholar] [PubMed]
- Householder NA, Harris CS, Kugler KM, Oakes DA, Powell SE (2022) Monomicrobial joint infection by Leclercia adecarboxylata in an immunocompetent patient after knee arthroscopy: a case report. JBJS Case Connect 12:1-5.
[Crossref] [Google Scholar] [PubMed]
- Voulalas G, Makris S, Papacharalampous G, Maltezos C (2016) Mycotic aneurysm due to Leclercia adecarboxylata: a complication of vertebral osteomyelitis. Ann Vasc Surg 33:229.e1-5.
[Crossref] [Google Scholar] [PubMed]
- Nelson MU, Maksimova Y, Schulz V, Bizzarro MJ, Gallagher PG (2013) Late-onset Leclercia adecarboxylata sepsis in a premature neonate. J Perinatol 33:740-742.
[Crossref] [Google Scholar] [PubMed]
- Sanchez Porto A, Casas Ciria J, Roman Enri M, Garcia Collado S, Bachiller Luque MR, et al. (2014) Leclercia adecarboxylata bacteraemia in an immunocompromised patient with metabolic syndrome. Infez Med 22:149-151. PMID: 24955804.
[Google Scholar] [PubMed]
- Atas DB, Velioglu A, Asicioglu E, Arikan H, Tuglular S, et al. (2017) Polymicrobial peritonitis with Leclercia adecarboxylata in a peritoneal dialysis patient. Saudi J Kidney Dis Transpl 28:181-182.
[Crossref] [Google Scholar] [PubMed]
- Marina VP, Abidi S, Malhotra D (2011) Leclercia adecarboxylata, an unusual hemodialysis catheter-related infection. Int Urol Nephrol 43:1257-1258.
[Crossref] [Google Scholar] [PubMed]
- Shah A, Nguyen J, Sullivan LM, Chikwava KR, Yan AC, et al. (2011) Leclercia adecarboxylata cellulitis in a child with acute lymphoblastic leukemia. Pediatr Dermatol 28:162-164.
[Crossref] [Google Scholar] [PubMed]
- Eiland EH, Siddiqui H, Goode AM, Leeth SD (2013) Pneumonia due to multidrug-resistant Leclercia adecarboxylata. Am J Health Syst Pharm 70:940-941.
[Crossref] [Google Scholar] [PubMed]
- Michael Z, McGann PT, Alao O, Stevenson L, Lesho E, et al. (2013) Isolation of Leclercia adecarboxylata from an infected war wound in an immune competent patient. Mil Med 178:e390-e393.
[Crossref] [Google Scholar] [PubMed]
- Papacharalampous G, Galyfos G, Geropapas G, Stamatatos I, Kerasidis S, et al. (2015) Infective aortic aneurysm caused by Leclercia adecarboxylata. Vasa 44:479-482.
[Crossref] [Google Scholar] [PubMed]
- Jover-Sáenz A, Cerezo-Esforzado E, Barcenilla-Gaite F, Garrido-Calvo S, Porcel-Pérez JM (2008) Leclercia adecarboxylata cholecystitis in a patient with metabolic syndrome. Surg Infect (Larchmt) 9:411-412.
[Crossref] [Google Scholar] [PubMed]
- Keren Y, Keshet D, Eidelman M, Geffen Y, Raz-Pasteur A, et al. (2014) Is Leclercia adecarboxylata a new and unfamiliar marine pathogen? J Clin Microbiol 52:1775-1776.
[Crossref] [Google Scholar] [PubMed]
- Haji S, Kimura H, Yamashita H (2014) Arthritis and bacteremia due to Leclercia adecarboxylata. Intern Med 53:2659.
[Crossref] [Google Scholar] [PubMed]
- Allawh R, Camp BJ (2015) Isolation of Leclercia adecarboxylata from a patient with a subungual splinter. Dermatol Online J 21:13030.
[Google Scholar] [PubMed]
- Fattal O, Deville JG (2000) Leclercia adecarboxylata peritonitis in a child receiving chronic peritoneal dialysis. Pediatr Nephrol 15:16-17.
[Crossref] [Google Scholar] [PubMed]
- de Baere T, Wauters G, Huylenbroeck A, Claeys G, Peleman R, et al. (2001) Isolations of Leclercia adecarboxylata from a patient with a chronically inflamed gallbladder and from a patient with sepsis without focus. J Clin Microbiol 39:1674-1675.
[Crossref] [Google Scholar] [PubMed]
- Tam V, Nayak S (2012) Isolation of Leclercia adecarboxylata from a wound infection after exposure to hurricane-related floodwater. BMJ Case Rep 2012:bcr-2012-007298.
[Crossref] [Google Scholar] [PubMed]
- Prakash MR, Ravikumar R, Patra N, Indiradevi B (2015) Hospital-acquired pneumonia due to Leclercia adecarboxylata in a neurosurgical centre. J Postgrad Med 61:123-125.
[Crossref] [Google Scholar] [PubMed]
- Lee B, Sir JJ, Park SW, Kwak CH, Kim SM, et al. (2009) A case of Leclercia adecarboxylata endocarditis in a woman with endometrial cancer. Am J Med Sci 337:146-147.
[Crossref] [Google Scholar] [PubMed]
- Chao CT, Hung PH, Huang JW, Tsai HB (2014) Cycler cassette rupture with Leclercia adecarboxylata peritoneal dialysis peritonitis. Perit Dial Int 34:131-132.
[Crossref] [Google Scholar] [PubMed]
- Longhurst CA, West DC (2001) Isolation of Leclercia adecarboxylata from an infant with acute lymphoblastic leukemia. Clin Infect Dis 32:1659.
[Crossref] [Google Scholar] [PubMed]
- García-Fulgueiras V, Seija V, Aguerrebere P, Cordeiro NF, Vignoli R (2014) First report of a clinical isolate of Leclercia adecarboxylata harbouring multiple resistance genes in Uruguay and review of the literature. J Glob Antimicrob Resist 2:77-81.
[Crossref] [Google Scholar] [PubMed]
- Dalamaga M, Pantelaki M, Karmaniolas K, Daskalopoulou K, Migdalis I (2009) Isolation of Leclercia adecarboxylata from blood and burn wound after a hydrofluoric acid chemical injury. Burns 35:443-445.
[Crossref] [Google Scholar] [PubMed]
- Kim HM, Chon CY, Ahn SH, Jung SJ, Han KH, et al. (2008) Fatal spontaneous bacterial peritonitis by Leclercia adecarboxylata in a patient with hepatocellular carcinoma. Int J Clin Pract 62:1296-1298.
[Crossref] [Google Scholar] [PubMed]
- Fernández-Ruiz M, López-Medrano F, García-Sánchez L, García-Reyne A, Ortuño de Solo T, et al. (2009) Successful management of tunneled hemodialysis catheter-related bacteremia by Leclercia adecarboxylata without catheter removal: report of two cases. Int J Infect Dis 13:e517-518.
[Crossref] [Google Scholar] [PubMed]
- Mazzariol A, Zuliani J, Fontana R, Cornaglia G (2003) Isolation from blood culture of a Leclercia adecarboxylata strain producing an SHV-12 extended- spectrum beta-lactamase. J Clin Microbiol 41:1738-1739.
[Crossref] [Google Scholar] [PubMed]
- Sawamura H, Kawamura Y, Yasuda M, Ohkusu K, Takahashi Y, et al. (2005) A clinical isolate of Leclercia adecarboxylata from a patient of pyelonephritis. Kansenshogaku Zasshi 79:831-835.
[Crossref] [Google Scholar] [PubMed]
- Hutton W, Allman E, McKeown C, Singer AC, Roberts AP (2023) Complete genome sequence of mcr-9 containing Leclercia adecarboxylata. Microbiol Resour Announc 12:e0048123.
[Crossref] [Google Scholar] [PubMed]
- Sano E, Fontana H, Esposito F, Cardoso B, Fuga B, et al. (2023) Genomic analysis of fluoroquinolone-resistant Leclercia adecarboxylata carrying the ISKpn19-orf-qnrS1-ΔIS3-blaLAP-2 module in a synanthropic pigeon, Brazil. J Glob Antimicrob Resist 33:256-259.
[Crossref] [Google Scholar] [PubMed]
- Stock I, Burak S, Wiedemann B (2004) Natural antimicrobial susceptibility patterns and biochemical profiles of Leclercia adecarboxylata strains. Clin Microbiol Infect 10:724-733.
[Crossref] [Google Scholar] [PubMed]
Citation: Di Gregorio M, Tiecco G, Colangelo C, Corbellini S, Caccuri F, et al. (2023) Leclercia adecarboxylata, An Emerging Pathogen: A Narrative Review. J Infect Dis Ther 11: 573 DOI: 10.4172/2332-0877.1000573
Copyright: © 2023 Di Gregorio M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 234
- [From(publication date): 0-0 - Nov 21, 2024]
- Breakdown by view type
- HTML page views: 198
- PDF downloads: 36