Research Article Open Access
Learning Curve for Ultrasound Assessment of the Fetal Heart at Nuchal Scan
Tudorache S1, Florea M1, Dragusin R2, Zorila L1, Patru CL1, Alexandru D3, Cara ML4* and Iliescu DG11Department of Obstetrics and Gynecology, Prenatal Diagnostic, University of Medicine and Pharmacy, Craiova, Dolj, Romania
2University Emergency Hospital, Craiova, Dolj, Romania
3Department of Informatics, University of Medicine and Pharmacy of Craiova, Craiova, Dolj, Romania
4Department of Public Health, University of Medicine and Pharmacy of Craiova, Craiova, Dolj, Romania
- *Corresponding Author:
- Monica Laura Cara
Department of Obstetrics and Gynecology, University Emergency Hospital
University of Medicine and Pharmacy of Craiova, Craiova, Dolj, Romania
Tel: 004 0723 963925
Fax: + 40251502179
E-mail: daimoniquelle@yahoo.com
Received date: January 20, 2017; Accepted date: January 24, 2017; Published date: January 30, 2017
Citation: Tudorache S, Florea M, Dragusin R, Zorila L, Patru CL, et al. (2017) Learning Curve for Ultrasound Assessment of the Fetal Heart at Nuchal Scan. J Clin Diagn Res 5:133. doi: 10.4172/2376-0311.1000133
Copyright: © 2017 Tudorache S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at JBR Journal of Clinical Diagnosis and Research
Abstract
Background: The aim of our study was to evaluate the characteristics of the learning curve of the first trimester (FT) fetal heart scan and to determine the required number of ultrasound examinations for training sonographers to accurately assess the normal fetal heart at 11–13+6 weeks’ gestation, by means of 2D ultrasound.
Methods: We selected four trainees (resident doctors) with theoretical knowledge and limited experience in FT/ST scan but without prior experience in performing first trimester fetal heart assessment. Each of them performed fetal heart ultrasound scanning in a cohort of 100 consecutive fetuses with normal heart during the routine nuchal translucency (NT scan), upon a pre-established protocol. The supervising doctor recorded if the sonographer succeeded in obtaining an informative 2D/2DC duplex sweep of the fetal heart. The time limit for scanning was 10 minutes. The data were analysed in three groups of examinations. Individual learning curves were delineated using moving average method.
Results: For all the trainees, there was a positive relationship between the number of FT scans and the number of good quality acquired clips. Assessment of fetal structures in first trimester can be accurately achieved by an inexperienced trainee after scanning 50 cases on average. The operating time was stabilized after 80 cases in moving average analysis.
Conclusion: Repeated scans increase ability to acquire good quality fetal heart sweep digital clips at the end of the first trimester of pregnancy.
FT fetal heart ultrasound assessment is a relatively simple procedure to learn and, once a moderate degree of experience is gained, should be routinely incorporated into NT scan. Policymakers should decide safety studies in respect to FT Doppler use in order to generalize the technique. After an adequate training the heart assessment does not prolong the nuchal scan.
Keywords
First trimester; Fetal heart; Ultrasound; Screening; Nuchal scan; Congenital heart defects
Introduction
Cardiac scan is preserved mainly to the second trimester, especially due to nowadays guidelines [1,2] and due to technical and financial limitations. Still, fetal nuchal translucency thickness (NT) measurement screening programs are continuously expanding worldwide, due to invaluable benefits in prenatal medicine [3-9].
Besides searching for chromosomal anomalies markers, the end-first trimester (FT) scan grew into the real and most important anomaly scan [10-12]. Recent year’s research proved that almost all major structural anomalies are detectable at this gestational age (GA), less the congenital heart diseases (CHDs) [2,13-15], despite the fact that they are among the most frequent of all congenital anomalies.
Many reasons should convince us to look early in pregnancy at the fetal heart, the most important being probably the early complete development of the heart [16] (unlike other systems eg. central nervous system or the kidneys), making the major CHDs detectable or at least questionable at the end of the FT, with few exceptions.
Another substantial reason is the fact that the majority of CHDs occur in low-risk patients [13,14,17,18]. In our view, at least these two reasons should support the idea of routine screening for CHDs and remove the concept of targeted early heart scan, offered to high-risk patients.
Due to low interest of observers in the FT cardiac area, we are at risk to lower exposure of the observers at FT cardiac anomalies than the true prevalence of CHD in the FT pregnancies. This is why we consider valuable the attempt to study early the normal fetal heart, being demonstrated the fact that if an observer is familiar with normal views of a structure, he will be more likely to suspect an anomaly of that structure, if present [1,2,19,20].
The purpose of this study was to assess the evolution of the learning curve for inexperienced trainees and to investigate the links between practicing and trainee’s success in obtaining interpretable images of the fetal heart.
We hypothesized that repeated scans will increase the different skilled obstetrician’s ability to acquire good quality FT fetal heart sweep digital clips. Another aim was to determine the number of ultrasound examinations necessary for training sonographers to examine accurately the fetal heart at 11–13+6 weeks’ gestation, by means of 2D ultrasound.
Materials and Methods
The study was performed in the Prenatal Diagnostic Unit (PDU) of the University Emergency Hospital Craiova, Romania. In the PDU there are performed on everyday basic nuchal scans. The inclusion criteria were: 11+0 and 13+6 weeks’ pregnancies verified by first-trimester measurement of fetal crown–rump length, low risk for CHD by history, absence of other systems structural abnormalities.
We chose this gestational age due to the general policy that advocates the FT genetic scan. The exclusion criteria were: multiple pregnancies, history of a previous pregnancy with any fetal anomalies, extracardiac anomalies present and patients that did not agree or were unable to give informed consent.
A generation of residents was offered practical training on examination of fetal heart at the end of the FT of pregnancy. The course was a three days intensive theoretical and hands-on course. They were all given practical training on a specific simplified protocol for examination of the fetal heart.
The study period was 12 months. We obtained data from four trainees in Prenatal Diagnostic Unit (PDU), Craiova, University of Medicine and Pharmacy, Romania. The trainees were assigned to two experienced obstetricians (ST, DGI), highly specialized in FT and ST heart scan.
There were three trainees that had the main interest in prenatal diagnostic and one trainee with main interest in other field (obstetrical manoeuvres). Among them, three sonographers were in training for obtaining The Fetal Medicine Foundation’s Certificate of Competence in the 11–14 Week Scan (for NT, NB and the tricuspid valve Doppler interrogation), and one of them had only limited education in FT ultrasound. None of them tried to scan the fetal heart in the first trimester previous to the study period.
Then they were asked to examine the fetal heart under the direct supervision of the trainer.
Ultrasound examinations were performed using a Voluson 730 Expert series and E8 (GE Medical Systems, Zipf, Austria) machine, equipped with 4-8 MHz curvilinear transducer. All scans were performed using speckle reduction imaging (SRI) and CrossXBeam CRI. When using color Doppler the mechanical and thermal indices were kept as low as possible (ALARA principle).
In our Prenatal Diagnostic Unit experience an oblique lateral insonation from the right part of the thorax is considered optimal for the visualization of the essential planes for FT fetal heart study.
Consequently, the FT fetal heart protocol was: the operator waited and focused to other segments of fetal anatomy until the fetus offered a lateral view from the right side of the thorax (or from the right shoulder); the angle beam was narrowed at 15-20 grades; the high definition zoom was then applied, until just the thorax was visualized, and occupied approx. 80% of the screen.
The operator was then allowed to turn on the color flow gate. The color Doppler maximal velocity setting was adjusted with the intention that the great arteries were equal, homogeneous in color and did not demonstrate aliasing.
The trainees were requested to obtain, by a simplified protocol, the cardiac sweep with two cardiac landmarks the inflows (the ventricular filling), the confluence of the two arches and also the normal spatial arrangement between the inflows and the outflows tracts.
This protocol was initially adopted due to constant concerns about first-trimester fetal exposure to ultrasound energy of all ultrasound societies. Its purpose was that the heart study would result in little added exposure of the fetus to ultrasound energy. Moreover, there is increasing evidence that using a simplified protocol reaches roughly the same performance in screening [21,22].
If mentioned variables were visualized by the supervising doctor the cardiac sweep was declared “sufficient” and noted as “yes” in the database. These results were recorded on a predesigned data sheet. The supervisor recorded also when the trainee obtained the sweep (minutes). Maximum time allowed for this manoeuvre was 10 min.
The study protocol was approved by the University Ethics Committee. Informed consent was obtained from all the participants.
Statistical Analysis
The frequency distribution of nominal variables and mean, standard deviation and median of continuous variables are presented as appropriate.
We used a two-way ANOVA test in order to describe a dependent variable (the time required for examination) according to several independent variables (trial number and trainee performing the investigation). Statistical significance level was set at P-values <0.05.
All statistical analyses were performed with IBM SPSS Statistics for Windows, Version 22.0. Software (Armonk, NY: IBM Corp).
Results
Each trainee performed a total of 100 examinations.
Data were analysed in 3 groups of 33 examinations (group A-first third of examinations 1-33, group B-second third of examinations 34-68, group C-last third of examinations 68-100) and in each group the percentage of unsuccessful examinations was calculated.
This failure rate varies among groups, having a decrease tendency till the end of the training program: 12.12%-48.49% (overall 32.65%) for group A, 0%-17.65% (overall 8.09%) for group B and 0% for group C (Table 1).
| T1 | T2 | T3 | T4 | Overall | |
|---|---|---|---|---|---|
| Group A | 12.12% | 30.30% | 39.40% | 48.49% | 32.56% |
| (First third) | (4/33) | 10/33 | 13/33 | 16/33 | (43/132) |
| Group B | 0% | 5.88% | 8.82% | 17.65% | 8,09% |
| (Second third) | (0/34) | (2/34) | (3/34) | (6/34) | (11/136) |
| Group C | 0% | 0% | 0% | 0% | 0% |
| (Last third) | (0/33) | (0/33) | (0/33) | (0/33) | (0/132) |
Table 1: Evolution of failure rate for each trainee during each group of examination.
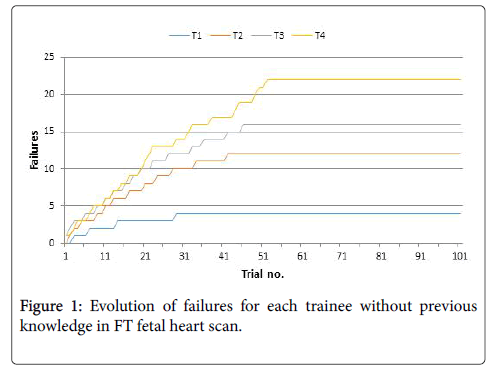
When started the statistical analysis by investigating the failures of the four trainees, we discovered that up to the 50th trial they still tended not be able to complete the investigations. It was also remarkable that in the last third, all four trainees had 100% success rate in identification of normality in required time.
Successful examination of the fetal heart was achieved in all cases by the first trainee after 30 scans, by the second trainee after 42 scans, and by the third trainee after 47 scans ant by the fourth trainee after 53 scans (Figure 1).
Overall operating time decreased from an average time of 9.17 minutes at the beginning of examinations to an average time of 3.80 minutes in the last third of the scans (Table 2).
| T1 | T2 | T3 | T4 | Total | |
|---|---|---|---|---|---|
| No. of trials | 33 | 33 | 33 | 33 | 132 |
| First third | 9.02 ± 1.83 | 9.17 ± 1.68 | 9.17 ± 1.56 | 9.33 ± 1.06 | 9.17 ± 1.55 |
| Last third | 3.95 ± 1.09 | 4.12 ± 1.17 | 3.55 ± 1.15 | 3.58 ± 1.27 | 3.80 ± 1.18 |
Table 2: Mean operating time–comparison between first third and last third of examinations.
We also proceeded to analyse the operating time needed to finalize the cardiac sweep.
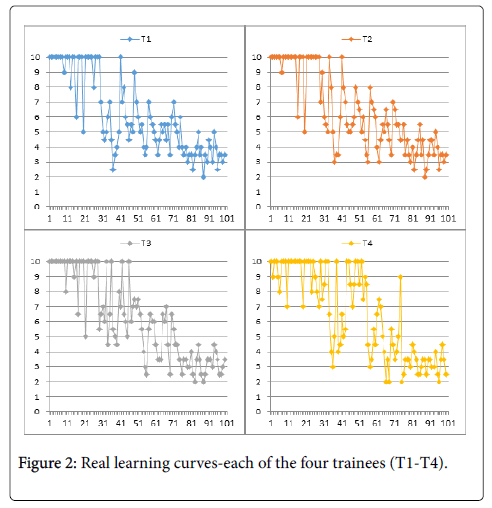
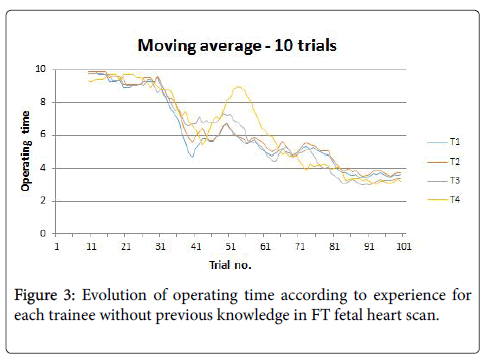
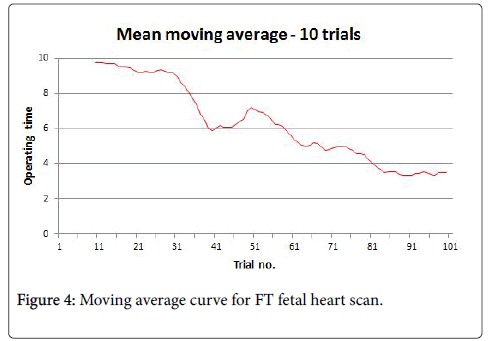
Because real learning curves for each of the four trainee are not very informative for the global trend of the learning process (Figure 2), we computed the moving average for 10 trials, for each of the four trainees (Figure 3) and as an average for all of them (Figure 4).
By analysing the shape of the resulting curves, we discovered that after an initial plateau-like region in the beginning, there is a steep slope at about the 30th trial up to the 40th trial, marking the acquiring of the necessary skill to perform the investigation, followed by a region featuring great variability, up to about the 70th trial, and one featuring less variability, mostly decrease, up to about the 80th trial.
From the 80th trial on, there is a new plateau reached, marking the end of the learning process.
Taking into consideration the above observations, we used a two - way ANOVA test in order to compare the first third (first 33 trials) of the training process with the last third (last 33 trials), to highlight if there is an inter-trainee influence on the learning process or not, or only experience being the main factor to influence the outcome.
The results show that the trainee (p=0.686) or the trainee dependence on number of repetitions (p=0.311) have not a significant statistical influence on the end result, and that only repeating the maneuver influences the outcome of the training (=1.82 x 10-90) (Table 3).
| Source of Variation | SS | df | MS | F | P-value* | F crit |
|---|---|---|---|---|---|---|
| Sample | 1904.1 | 1 | 1904.1 | 1001.58 | 1.82 x10-90 | 3.87804 |
| Columns | 2.82576 | 3 | 0.94192 | 0.49546 | 0.68574 | 2.63986 |
| Interaction | 6.83712 | 3 | 2.27904 | 1.1988 | 0.31074 | 2.63986 |
| Within | 486.682 | 256 | 1.9011 | |||
| Total | 2400.44 | 263 | ||||
| *two-way ANOVA | ||||||
Table 3: Effects of the trainee influence, the trainee dependence on number of repetitions and the repetition of the maneuver on outcome of the training-comparison between first third and last third of examinations.
Discussion
The results from this study indicate good results for all our inexperienced trainees in the ability of demonstrating the main normal features of the heart structures at the end of first trimester of pregnancy.
Our findings demonstrate that for a sonographer without experience in FT fetal heart scanning the minimum number of scans required to become competent in examining the fetal heart is 50 cases. The operating time stabilized after 80 cases in moving average analysis.
At the end of the learning period all four trainees had 100% success rate in identification of normality in required time less than 10 minutes, which leads us to the idea that in experienced hands, FT fetal heart screening is not time-consuming.
Previous studies report that a good sonographer, experienced in NT scanning needs to perform on average 80 examination in order to achieve the level of competence in scanning for ductus venosus [5], 40 examination for frontomaxillary facial angle measurement [6,7] and 80 examination for nasal bone measurement [4]. Compared to this findings, FT scanning fetal heart with color Doppler applied could be faster achieved even by an inexperienced sonographer.
The most striking finding of this research is that in our study the variation of operating time was proved to depend only on the moment of the training (beginning versus end), while the trainee or the influence between moment and trainee (interaction) has no impact on the observed variation.
To our knowledge, there are no reports on the fetal heart scan learning curve in the first trimester. This is probably due to two main factors: the first one is the continuous debate if we should screen for the heart in the first trimester or not; the second is that until present, there is no agreement on the technique of examination of the fetal heart in the FT.
We will try to comment on these two issues: Since 2000, when the early heart scan was sentenced to be “ill-advisable” [23], in the FT scanning a true revolution took place, in terms of systems’ performance and operators’ skills. There were many reports that FT heart study is feasible and achievable in selected high-skilled individuals [10,11,19,24,25]. Yet, professional organisms, in recently elaborated guidelines, state that only “the normal position of the heart on the left side of the chest should be documented” and although “more detailed sonographic assessment of cardiac anatomy has been demonstrated to be feasible at 11 to 13+6 weeks, this is not part of routine assessment” [2]. Moreover, “for safety reasons, use of Doppler is not indicated during routine scanning” [2].
This approach is reasonable, being demonstrated that the detection rates for CHD maintained low, unlike detection rates for other systems, despite training programs wide world, even in routine ST scans [1,13-15]. Moreover, the safety on applying Doppler in the FT did not reach definitive scientifically proved conclusions [26]. On the other hand, ultrasound has an extraordinary “safety record”, being used (and sometimes abusive used) for more than five decades, without a single case of side-effects on the fetus due exclusively to early ultrasound energy exposure reported. For these reason, we are in danger to consider that safety is implied, and this attitude could prove to be wrong in the unforeseeable future.
On the other hand, most reports do not meet criteria for an accuracy study, and this is also reasonable, because the acceptability of the medical terminations (MTOPs) is lower than for surgical TOPs, and even in cases of MTOPs, FT pathology remains challenging, because usually it is either not performed, or not-reliable [11,12,24,27]. This is a reality due to practical limitations in postmortem examination of the FT human fetal heart, because of its small size and fragility. These are the reasons that made some experts conclude that “certainly, only good, reliable images of the beating fetal heart represent, up to now, the gold standard for an early diagnosis of cardiac malformations” [28].
In our view, the main reason why the detection rates of CHD remain so low, despite the ever-improving ultrasound machines resolution is infrequent exposure of observers to cardiac anomalies. Yet, it is already demonstrated the fact that observers that do know what specific normal views must look like, are more likely to diagnose an abnormal view. In other words, an observer used to look at a normal structure will notice faster the abnormality of that structure. This idea is the ground which permits the “expertize” concept.
Our assumption was that, like in many other issues, if a standard protocol is used, FT images of the heart are more interpretable. Moreover, the direction and the spatial arrangement of the great arteries are easy to visualize at the end of the first-trimester if applying color Doppler, both in 2D ultrasound and in color rendered STIC datasets [19].
Further research of this sample of doctors, and of others that contain detailed information on the characteristics of participants will help test the hypothesis that training is important in gaining skills in FT scanning and other hypotheses, like the one that the individual motivation has an important impact on the results.
Future research on these topics is crucial for researchers interested in using the workplace as a screening for CHD center.
There are two significant limitations of this study. To begin with, is the small number of the participants. On the other hand, we did not stratify for other confounders, usually present in real life scanning, such as anterior/posterior placenta, acoustic characteristics of each patient (friendly/unfriendly tissue), subjective amount of amniotic fluid, bowel filling, uterus position (incomplete anteversion or anteflexion), scarred uterus or scarred abdominal wall; we consider that the results of our study would not be influenced by these parameters, being processed a large number of patients.
Our study carries with it strengths that offset these limitations. First, the cohort of trainees belongs from a well-defined population of residents who entered the challenging field of prenatal diagnostic in a specific geographic region, in a developing country, that struggles with a chronic underfunding in healthcare, thereby reducing biases inherent in convenience or other sampling procedures. The strengths of the longitudinal structure were exploited to control for other construct, such as training in other centers. All cases examinations were directly supervised and had normal hearts, thus less subject to recall bias. The longitudinal design also allowed us to look at evolving behaviours, such as the time spent to optimize the setting of the machines, translated in the time required to obtain the sweep, which to our knowledge, has never been performed before. Finally, the sample was an urban-based community cohort of a Universitary Emergency Hospital. Research on work in this population is limited, and our study lends evidence to the notion that the link between practicing and skills is generalizable to settings of varying economic conditions.
Conclusions
Although FT fetal heart scanning is nowadays still seen as a superior technique, and recommendations are that it should be offered in selected cases, we have proved that skills are achievable in a relative short period of time, if the observer is young and motivated, following a standard simple protocol. Bearing in mind the fact that the majority of CHD cases belongs to low-risk patients, a screening method should be attempted in all settings where nuchal scan is performed. The only limitation that is morally acceptable is the access to high-resolution equipment.
Previous research has indicated that early diagnostic of CHD is feasible and that it is associated with reductions in prevalence of neonatal mortality and morbidity [29-31]. Thus, efforts should be made to establish workplace-based training programs. These programs would ideally incorporate educational strategies pertinent to young obstetricians. Finally, this research should highlight the need for future studies to carefully and systematically evaluate the safety of using Doppler in the FT, since this technique is the most informative way to obtain early important information about the heart and great vessels [19,22].
We concluded that the FT fetal heart scanning, using this simplified protocol, is achievable in a relatively short period of training. These results may matter when designing FT screening programs for MCHDs. Our findings may highlight the need that looking at fetal heart should be routinely incorporated into NT scan in order to reassure normality.
Acknowledgement
We are grateful to all the members of the Prenatal Diagnostic Unit who provided and cared for study patients. We would like to acknowledge with appreciation to Prof. Nicolae Cernea for his valuable contributions to this paper.
References
- Salomon LJ, Alfirevic Z, Berghella V, Bilardo C, Andrade H, et al. (2011) Practice guidelines for performance of the routine mid-trimester fetal ultrasound scan. Ultrasound Obstet Gynecol 37: 116-126.
- Salomon LJ, Alfirevic Z, Bilardo CM, Chalouhi GE, Ghi T, et al. (2013) ISUOG practice guidelines: performance of first-trimester fetal ultrasound scan. Ultrasound Obstet Gynecol 41: 102-113.
- Souka AP, Kaisenberg CS, Hyett JA, Sonek JD, Nicolaides KH(2005) Increased nuchal translucency with normal karyotype. Am J Obstet Gynecol192: 1005-1021.
- Cicero S, Dezerega V, Andrade E, Scheier M, Nicolaides KH (2003) Learning curve for sonographic examination of the fetal nasal bone at 11-14 weeks. Ultrasound Obstet Gynecol 22: 135-137.
- Maiz N, Kagan KO, Milovanovic Z, Celik E, Nicolaides KH (2008) Learning curve for Doppler assessment of ductus venosus flow at 11+0 to 13+6 weeks' gestation.Ultrasound Obstet Gynecol 31: 503-506.
- Yang X, Chen M, Wang HF, Leung TY, Borenstein M, et al. (2010) Learning curve in measurement of fetal frontomaxillary facial angle at 11-13 weeks of gestation. Ultrasound Obstet Gynecol 35: 530-534.
- Chen M, Yang X, Leung TY, Sahota DS, Fung TY, et al. (2009) Study on the applicability of frontomaxillary facial angle in the first-trimester trisomy 21 fetuses in Chinese population. Prenat Diagn 29:1141-1144.
- D'Alton ME, Fuchs KM, Abuhammad A, Benacerraf B, Berkowitz R, et al. (2014)Nuchal Translucency Quality Review Program. Implementation of a national nuchal translucency education and quality monitoring program. Obstet Gynecol 123: 149-154.
- Evans MI, Krantz DA, Hallahan TW, Sherwin J (2012) Impact of nuchal translucency credentialing by the FMF, the NTQR or both on screening distributions and performance. Ultrasound Obstet Gynecol 39: 181-184.
- Iliescu D, Tudorache S, Comanescu A, Antsaklis P, Cotarcea S, et al. (2013) Improved detection rate of structural abnormalities in the first trimester using an extended examination protocol.Ultrasound Obstet Gynecol 42: 300-309.
- Becker R, Wegner RD (2006) Detailed screening for fetal anomalies and cardiac defects at the 11-13-week scan. Ultrasound Obstet Gynecol 27: 613-618.
- Bromley B, Shipp TD, Lyons J, Navathe RS, Groszmann Y, et al. (2014) Detection of fetal structural anomalies in a basic first-trimester screening program for aneuploidy. J Ultrasound Med 33: 1737-1745.
- Lee W, Carvalho JS, Chaoui R, Copel J, Hecher K, et al. (2006) Cardiac screening examination of the fetus: guidelines for performing the 'basic' and 'extended basic' cardiac scanUltrasound Obstet Gynecol 27: 107-113.
- Allan L (2010) Fetal cardiac scanning today. Prenat Diagn 30: 639-643.
- Jørgensen DES, Vejlstrup N, Jørgensen C, Maroun LL, Steensberg J, et al. (2015) Prenatal detection of congenital heart disease in a low risk population undergoing first and second trimester screening. Prenat Diagn 35: 325-330.
- Abuhamad A, Chaoui R (2010)A practical guide to fetal echocardiography : normal and abnormal hearts. 2nd ed. Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkinspp: 379.
- Becker R, Schmitz L, Kilavuz S, Stumm M, Wegner RD, et al. (2012) Normal nuchal translucency: a justification to refrain from detailed scan? Analysis of 6858 cases with special reference to ethical aspects. Prenat Diagn 32: 550–556.
- Allan L, Benacerraf B, Copel JA, Carvalho JS, Chaoui R, et al. (2001) Isolated major congenital heart disease. Ultrasound Obstet Gynecol 17:370-379.
- Tudorache S, Cara M, Iliescu DG, Novac L, Cernea N (2013) First trimester two-and four-dimensional cardiac scan: intra-and interobserver agreement, comparison between methods and benefits of color Doppler technique, Ultrasound Obstet Gynecol 42: 659-68.
- Carvalho JS, Allan LD, Chaoui R, Copel JA, DeVore, et al. (2013) ISUOG Practice Guidelines (updated): sonographic screening examination of the fetal heart, Ultrasound Obstet Gynecol 41: 348-359.
- Orlandi E, Rossi C, Perino A, Musicò G, Orlandi F (2014) Simplified first-trimester fetal cardiac screening (four chamber view and ventricular outflow tracts) in a low-risk population. Prenat Diagn 34:558-563.
- Tudorache S, Iliescu DG, Florea M, Dragusin R, Patru C, et al. (2016) OC14.02: Two planes for the first trimester major congenital heart diseases screening. Ultrasound Obstet Gynecol, 48: 25-26.
- Rustico MA, Benettoni A, D'Ottavio G, Fischer-Tamaro L, Conoscenti GC, et al. (2000) Early screening for fetal cardiac anomalies by transvaginal echocardiography in an unselected population: the role of operator experience.Ultrasound Obstet Gynecol16: 614-619.
- Lombardi CM, Bellotti M, Fesslova V, Cappellini A (2007) Fetal echocardiography at the time of the nuchal translucency scan. Ultrasound Obstet Gynecol 29: 249-257.
- Rasiah SV, Publicover M, Ewer AK, Khan KS, Kilby MD,et al(2006) A systematic review of the accuracy of first-trimester ultrasound examination for detecting major congenital heart disease.Ultrasound Obstet Gynecol 28: 110-116.
- Torloni MR, Vedmedovska N, Merialdi M (2009) Safety of ultrasonography in pregnancy: WHO systematic review of the literature and meta-analysis. Ultrasound Obstet Gynecol 33: 599–608.
- Boyd PA, Tondi F, Hicks NR, Chamberlain PF (2004) Autopsy after termination of pregnancy for fetal anomaly: retrospective cohort study. BMJ 328:137.
- Bellotti M, Fesslova V, Gasperi CD, Rognoni G, Bee V, et al. (2010) Reliability of the first-trimester cardiac scan by ultrasound-trained obstetricians with high-frequency transabdominal probes in fetuses with increased nuchal translucency. Ultrasound Obstet Gynecol 36:272-278.
- Donofrio MT, GradyAJM, Hornberger LK, Copel JA, Sklansky MS, et al. (2014) Diagnosis and treatment of fetal cardiac disease: a scientific statement from the American Heart Association.Circulation 129: 2183-2242.
- Hoffman JI, Kaplan S, Liberthson RR (2004) Prevalence of congenital heart disease. Am Heart J 147: 425-439.
- Rosano A, Botto LD, Botting B, Mastroiacovo P (2000) Infant mortality and congenital anomalies from 1950 to 1994: an international perspective. J Epidemiol Community Health 54: 660-666.
Relevant Topics
- Back Pain Diagnosis
- Cardiovascular Diagnosis
- Clinical Diagnosis
- Clinical Echocardiography
- COPD Diagnosis
- Diabetes Diagnosis
- Diagnosis Methods
- Diagnosis of cancer
- Diagnosis of CNS
- Diagnosis of Diabetes
- Diagnostic Products
- Diagnostics Market Analysis
- Heart diagnosis
- Immuno Diagnosis
- Infertility Diagnosis
- Medical Diagnostic Tools
- Preimplementation Genetic Diagnosis
- Prenatal Diagnostics
- Ultrasonography
Recommended Journals
Article Tools
Article Usage
- Total views: 7773
- [From(publication date):
June-2017 - Apr 02, 2025] - Breakdown by view type
- HTML page views : 6781
- PDF downloads : 992