Late Complication of a Couvelaire Uterus: Case Report and Literature Review
Received: 27-Jan-2019 / Accepted Date: 28-Mar-2019 / Published Date: 04-Apr-2019
Abstract
Couvelaire uterus is a rare but nonfatal complication of severe forms of abruption placentae. A diagnosis of this condition can only be made by direct visualization or biopsy. Its incidence is difficult to define. The subject of this report is a 32 years old pregnant woman G1, who had a placental abruption, bleeding per vagina and stillbirth and whose uteroplacental apoplexy was diagnosed at the time of the Caesarean Section (CS). Several hours after the CS, during which patient’s condition worsened, an emergency hysterectomy was performed, because of persistent uterine bleeding and hemoperitoneum associated with hypofibrinogenemia.
Keywords: Couvelaire; Abruption placentae; Uteroplacental apoplexy; Retrouterine hematoma; Disseminated intravascular coagulation; Hysterectomy
Introduction
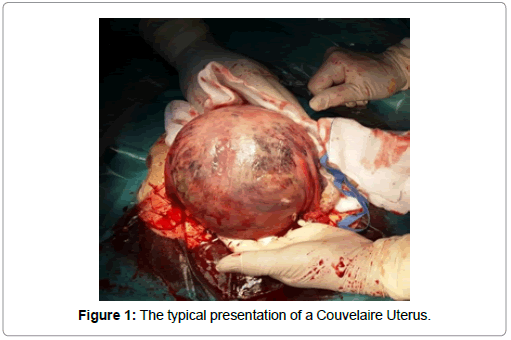
Couvelaire uterus, also known as uteroplacental apoplexy, is a rare but nonfatal condition resulting from extravasation of blood into the uterine musculature and surrounding tissues [1]. It was first described in the medical literature by Alexandre Couvelaire, a 1912 French obstetrician. This condition is typically associated with abruption placentae, the premature separation of the placenta, enabling blood to penetrate the myometrium and parametrium [2]. Diagnosis is made by direct visualization during caesarean section or biopsy [3]. Its characteristic appearance is a bluish or purple colour, mottled by ecchymoses [4]. Its real incidence is difficult to define and some estimate its occurrence as high as 20%, while others estimate it as low as 5% [5].
Case Report
A 32-year-old woman G1 para 0 at 34 weeks and 6 days was admitted to our department. The diagnosis was: Abruption placentae, stillbirth and bleeding per vagina.
At admission, the patient complained of abdominal pain, started earlier during that evening, and no fetal movement since the day before. Heart rate was 70 bpm, blood pressure 110/75 and the uterus was subcontracted. Vaginal examination showed profuse vaginal bleeding and 2 cm dilated, effaced cervix. Abdominal ultrasound examination revealed a nonviable fetus in a cephalic position, fundic placenta with retroplacental clots and a considerably reduced amniotic fluid.
Lab test showed the following values: Haemoglobin 10.9 g/dL, haematocrit 31.2%, a mild thrombocytopenia 133 x 10^3/mcL, a white blood cell count 16.08 × 103/mcL (reference range 4.50-10.00 × 103/ mcL), prothrombin time and partial thromboplastin time were in the normal range, while fibrinogen and D-Dimer respectively showed a value of 138 mg/dL (150-450 mg/dL) and a value of 29427 ng/mL (0- 200 ng/mL).
With a diagnosis of stillbirth and the evidence of a large retroplacental hematoma, in order to reduce the risks of Disseminated Intravascular Coagulation (DIC), the patient was brought to the operating room for a caesarean section.
A primary low transverse caesarean section was performed via a Pfannenstiel skin incision. As the abdomen was opened, the uterus was found to be dark, indurated, wooden-like, ecchymotic and with petechial areas. This was the typical clinical presentation of a Couvelaire uterus. The uterus was transected, with the spillage of blood mixed with clots and the contemporary leakage of the placenta with a wide hematoma from abruption. A nonviable fetus of 2.330 kg was delivered, according to the gestational age (50 growth percentile) (Figure 1).
Caesarean section was uneventful with an estimated blood loss of 700 cc. A careful inspection of the tubal serosa, ovarian surface, utero-ovarian and infundibulopelvic ligaments showed no signs of blood extravasation and no superficial ecchymosis changes. The uterus showed a normal tone and size. Further inspection of the surrounding tissues showed no active bleeding. No significant vaginal blood loss was noted. After the Caesarean section, lab test showed a value of haemoglobin at 7.8 mg/dL, compatible with the plentiful loss of blood.
Patient was carefully monitored for several hours after delivery. She showed no signs of clinical deterioration. Nevertheless, a blood test performed three hours after the CS showed markedly abnormal values: Haemoglobin 7.4 mg/dL, fibrinogen 96 mg/dL (150-400 mg/ dL), platelets 89 x 10^3 mcL and INR 1.42 (0.8-1.2). These values are all compatible with progressive consumption of clotting factors and disseminated intravascular coagulation at an early phase. Blood transfusion and infusion of fresh frozen plasma were therefore administered. An ultrasound scan, performed 4 h after CS, showed a normal sized uterus with an empty uterine cavity and no signs of hemoperitoneum. Nevertheless, 12 h after caesarean section, an abdominal CT revealed the presence of an hemoperitoneum, with periuterine oozing and a dimensional increase next to the anteroinferior wall of the uterus.
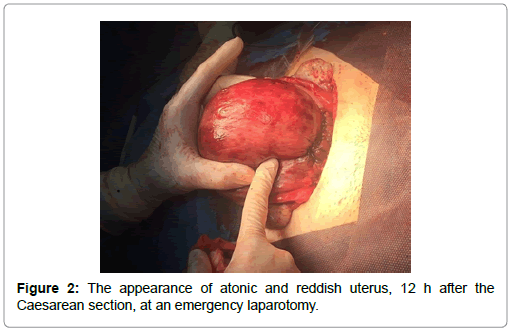
Due to worsening of hemodynamic balance and severe anaemia with a haemoglobin drop to 6.5 mg/dL, an emergency laparotomy was performed. The uterus showed a severe atony and the whole surface was reddish and covered by a soft and spongy haematoma. Its consistence appeared very weak, due to a massive wall infarction. Suture of the uterine incision showed no abnormality. A first dose of intravenous Sulprostone and then directly intrauterine was injected. Despite these measures, due to persistent and diffuse blood seeping and visible haemorrhagic infarction, extending to ovaries and uteroovarian ligaments, a subtotal hysterectomy was required. Shortly after the removal of the uterus significant improvements of patient’s condition occurred. Postoperative course was uneventful and patient was discharged 4 days after operation (Figure 2).
Discussion
Diagnosis of Couvelaire Uterus (CU) is generally made by inspection during surgery. Etiology of this condition remains uncertain though its occurrence is frequently associated with one or more of obstetrical complications such as placental abruption, uterine atony, bleeding from placenta previa, coagulopathy, amniotic fluid embolism and uterine rupture. Onset of a CU developed after an iatrogenic perforation during dilatation and curettage has also been reported [6].
Nevertheless, a recent case describes the occurrence of a CU without any of the abovementioned predisposing conditions [7].
The exact incidence has been difficult to determine and it varies between 5% and 20%. Among the reported cases of Post-Partum Haemorrhage (PPH) related to atony, the incidence of CU has been estimated to reach 2.6 % of the total. Its occurrence increases to 39% in case of bleeding from abruption placentae [8].
Since blood clots are dissecting the myometrium in CU, this results in an impairment of the contracting strength of the uterus and subsequent atony. On the other side, the dissecting process causes persistent oozing through the serosal surface involving especially the tube with an acute drop in hemoglobin levels and hypofibrinogenemia as result. Therefore, prompt use of uterotonics (Carbetocin, Sulproston) is mandatory during several hours after surgery, when diagnosis of CU has been made. Careful observation of the coagulation markers (PT, PTT, fibrinogen) can orientate the diagnosis and prevent the onset of a DIC.
Prospective observational studies involving all the patients with abruption placentae stated that CU followed abruption placentae in 39% of the cases and that the medical treatment was effective in 58% of CU. Failure of the medical approach requested hysterectomy in 8.3% of cases and other surgical treatment in 41% of the cases (b-lynch or dearterialization). Use of haemostatic suture (technique of B-Lynch) may be an alternative to control uterine hemorrhage associated with hypertensive disorders. No hysterectomy was needed in those cases of abruption placentae not complicated by uterine apoplexy [8].
Conclusion
We believe that conservative (surgical or medical) management of the uterine apoplexy can be reliable during the initial phases of the pathological changes related to this condition. At a subsequent stage, the findings of a wide bloody hematoma of the uterine walls and a vivid, reddish appearance of the serosal uterine surface become clearly visible. The adoption of conservative measures at this stage can be very hazardous due to the concrete risk of severe complications e.g., hemorrhagic shock and DIC. In addition, inappropriate use of tightening sutures (B-lynch) at an advanced stage, as last resort to avoid hysterectomy, can lead to fatal lacerations of the uterus and is therefore not indicated [9].
References
- Habek D, Selthofer R, Kulas T (2008) Uteroplacental apoplexy (couvelaire syndrome). Wien Klin Wochenschr 120: 88.
- Couvelaire A (1912) Two new observations of utero-placental apoplexy (retro-placental hemorrhage with infiltration of the uterus. Ann Gynecol Obstet 9: 486.
- Rathi M, Rathi SK, Purohit M, Pathak A (2014) Couvelaire uterus. BMJ Case Rep.
- Uwagbai ON, Wittich AC (2017) A 30 year old female found to have a couvelaire uterus with placenta accreta during planned caesarean delivery. Mil Med 182: e1877-e1879.
- Hubbard JL, Hosmer SB (1997) couvelaire uterus. J Am Osteopath Assoc 97: 536-537.
- Osial P, Atkinson AL, Sherlock D, Moskowitz D (2013) An unreported etiology for couvelaire uterus. SEAJCRR 2: 244-248.
- Shreedevi K, Mudanur SR, Neelamma P, Aruna SN, Aishwarya J, et al. (2014) Couvelaire uterus without placental abruption: A rare case report. J Evolution Med Dent Sci 3: 9787-9789.
- Sunanda N, Sruthi T, Sheela SR (2018) Feto-maternal outcome in patients with couvelaire uterus: A 3 year study in a tertiary care hospital in rural Karnataka, India. Int J Reprod Contracept Obstet Gynecol 7: 503-507.
- Aydın DS, Hasanova M, Göksedef PC, Ekmez M, Çetin A (2016) Failure of B-Lynch compression suture in a patient with couvelaire uterus and uterine atony. Med Bull Haseki 54: 47-49.
Citation: Cipullo LMA, Poto GE, Zullo F, Merciai F, Guida M (2019) Late Complication of a Couvelaire Uterus: Case Report and Literature Review. J Preg Child Health 6: 407.
Copyright: © 2019 Cipullo LMA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 9745
- [From(publication date): 0-2019 - Nov 17, 2025]
- Breakdown by view type
- HTML page views: 8749
- PDF downloads: 996