Research Article Open Access
Lassa Fever Epidemic in Nigeria - Outbreak Investigation, Risk Factors and Empirical Analysis from 2012 To 2016
Jimoh Mohammed Saka1*, Aishatu Bintu Gubio2, Yennan Sebastian Kerecvel3, Aisha Oluwatoyin Saka4, Akin Oyemakinde51Department of Epidemiology and Community Health, College of Health Sciences, University of Ilorin, Ilorn Kwara State Nigeria
2Nigeria Field Epidemiology and Laboratory Training Program, Federal Ministry of Health, Nigeria
3Epidemiology Division of Federal Ministry of Health, Nigeria
4Department of Pediatrics and Child Health Faculty of Clinical Sciences, University of Ilorin, Nigeria
5Nigeria Centre for Disease Control, Federal Ministry of Health, Abuja, Nigeria
- *Corresponding Author:
- Jimoh Mohammed Saka, Ph.D
M.D, Department of Epidemiology and Community
Health Faculty of Clinical Sciences
College of Health Sciences, University of Ilorin
Ilorn Kwara State Nigeria
Tel: +23480686345
E-mail: sakamj1@yahoo.com
Received date: April 07, 2017; Accepted date: April 27, 2017; Published date: May 04, 2017
Citation: Saka JM, Gubio AB, Kerecvel YS, Saka AO, Oyemakinde A (2017) Lassa Fever Epidemic in Nigeria - Outbreak Investigation, Risk Factors and Empirical Analysis from 2012 To 2016. J Comm Pub Health Nurs 3:170. doi:10.4172/2471-9846.1000170
Copyright: © 2017 Saka JM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited
Visit for more related articles at Journal of Community & Public Health Nursing
Abstract
Lassa haemorrhagic fever caused by the Lassa virus is an acute, highly infectious zoonotic disease. Magnitude of disease is becoming greater with increasing mortality and morbidity and spread to other area in Nigeria. The study accessed outbreak outcome, risk factors and empirical analysis from 2012 to 2016.
Active case search conducted included health facilities that treated confirmed and suspect cases, as well as their residential and business premises using questionnaire and Laboratory analysis. All cases were identified based on the adopted case definition of a person with severe illness of <3 weeks duration and temperature ≥ 38ºC. Individuals with potential direct exposure to Lassa virus through contact with a case were risk assessed. Evidence from data LF cases recorded for five years were analysis using Epi Info 6.
A total of Eight (8) cases were seen during the period of investigation. Three (3) was confirmed, one of the confirmed case who was a doctor died. Case fatality rate is 37.5%. Over 50% of the cases are aged between 25-40 years. Median age is 26 year with range 1-55years. Five of the eight cases (62.5%) are males. 100% of patients live in Markudi but 86.5% are Ibo settlers. Out of the 53 contacts that were assessed for risk, 25 (47.2%) were categorized as no risk, 25 (47.2%) were categorized as low risk, while 3 (5.6%) were high risk contacts. Between the period of five years 5051 cases conformed, with 3891 death from LF with case fatality of 77.03%. Risk factors for transmission not limited ethical believe, ignorance and misinformation.
LF infection is on increase, affecting both health and non-health workers Over half of the contacts had direct contact with this case. Adopting proper standard precautions in hospitals as well as communities is recommended.
Keywords
Lassa fever; Outbreak investigation; Risk factors; Case fatality; Nigeria
Introduction
Lassa fever is an acute viral haemorrhagic illness caused by Lassa virus, a member of the arenavirus family of viruses VHFC, 2013 [1]. It is transmitted to humans from contacts with food or household items contaminated with rodent excreta CDC, 2004 [2]. The disease is endemic in the rodent population in parts of West Africa. Person-toperson infections and laboratory transmission can also occur, particularly in the hospital environment in the absence of adequate infection control measures Ogbu et al. [3]. Diagnosis and prompt treatment are essential.
Lassa fever which has incubation period of 6-21 days is endemic to some parts of Nigeria including Benue state [4]. Lassa Virus is highly contagious, classified by the American centers for Disease control and prevention as class A virus and requiring bio-safety level for management Quick Reference Guide, 2015 [5]. The disease is especially severe in late pregnancy, with maternal death and/or fetal loss occurring in greater than 80% of cases during the third trimester. There has been concerted effort at prevention of Lassa Fever (LF) outbreak following the unprecedented record of 2012, many events like recent flooding and ethnic clashes among the people have caused an increase in vulnerable population as well as the possibility of human contact with rodents, among which is the Mastomys natalensis, the reservoir and host to the Lassa germ Weekly Epidemiology Report, 2015 [6].
As reported by WHO, 2005 [7] Lassa hemorrhagic fever caused by the Lassa virus is endemic in some countries in West Africa including Guinea, Liberia, Sierra Leone and parts of Nigeria. It is an acute, highly infectious zoonotic disease whose public health importance is heightened by its nosocomial spread especially in areas endemicity [8]. The host agent for the Lassa virus is the multimamate rat called mastomys natalensis. Lassa infested rat does not become ill, but sheds the virus in its urine and droppings. Humans are infected when they come in direct contact with this urine, feces deposited on surfaces such as floors or beds, or in food or water WHO, 2005 [7]. Those who eat rodents as delicacies or those who kill them for sport are most likely to be infected by direct contact with its blood. Rat bites on humans is also another avenue for zoonotic transmission.
In the study by Richmond and Baglole [9] Person-to-person and laboratory infections occur, especially in the hospital environment, by direct contact with blood (including inoculation with contaminated needles), pharyngeal (throat) secretions or urine of a patient, or by sexual contact. Person-to-person spread may occur during the acute phase of fever through aerosolized cough/saliva droplets when the virus is present in the throat. Lassa fever symptomatically mimics that of malaria and typhoid fever and is often not diagnosed in the early stages. The case presents with fever, headache, sore throat, retrostenal pain, nausea, vomiting, diarrhoea, cough, abdominal pain, non-injury related haemorrhage Kerne et al. [10]. In about 80% of the infections, clinical presentation may be mild without any observable symptoms CDC, 2004 [2] while the remaining 20% may have severe multisystem disease. In the absence of treatment with antiviral drug Ribavirin 15% of patients who get hospitalized will eventually die.
Following request from State Government for an investigation of LF epidemic a multi-sectoral team was formed by the Federal and State Ministries of Health and the Nigerian Field Epidemiological. Laboratory Training Program (NFELTP) and Public Health Consultant to respond to this outbreak. The study aimed to determine the magnitude of LF in Nigeria over five years and specifically to characterize LF outbreak in terms of time, place and person, assess infection control capacity of health facilities involved in management case and contacts in Benue State, confirm cases based on standard case definition, assess and categorize risk among contacts, institute control measures and ensure public health action. In conducting the study the two null hypothesis are:
1. There was no outbreak of Lassa fever in Benue State.
2. There is poor LF infection control among health facilities in Benue State.
Materials and Methods
Active case search conducted included health facilities which treated confirmed and suspect cases, in carrying out the investigation the steps taking include; Site investigation preparation for field work, verification of the diagnosis, existence of an epidemic was established, cases was identified and counted. Data analysis: time, place and person. Formulate and test hypothesis, assess the local response capacity, set up immediate control measures, address the resource gaps report writing, dissemination of findings and intensify surveillance.
Sites of investigation
All sites investigated were directly linked to confirmed or suspected cases and their contacts. These sites were found in two local government areas namely, Makurdi and Okpokwu Local Government Areas. Markurdi Local Government Area is one of the 23 LGAs that make up State. It is situated on the northern part of the State and is the first Local Government to be accessed if entering Benue State through the Abuja-Nasarawa route. It is also the capital of Benue State with a population of about 500,797 including native Tivs, Idomas, Igedes and settlers. It has an airport and is also the base for the Nigeria Air force’s MiG 21. Being centrally located, it is often a transit town for commuters and others travelling to such States as Enugu (eastern Nigeria), Plateue, Nassarawa, Taraba, etc. Benue Local Government also houses a Federal University of Agriculture and the Benue State University, which teaching hospital played a major role in this investigation. All reported cases during this outbreak are residents and had sort medical care in Benue Local Government. Sites investigated in the local government include:
1. Divine love Hospital
2. Hospital of Immaculate conception
3. Bishop Murray Hospital
4. Benue State University Teaching Hospital
Ukpokwu Local Government Area is in the south-eastern part of Benue State. It is a border community to Enugu State and is home to the State Polytechnic at Ugbokolo. Ugbokolo is a rural town of about 25,123 people Aper [11] whose idyllic existence has been hastily affected by the influx of students. In the absence of proper accommodation within the school premises, students rent accommodation and live among the community people.
Case Definition
Any person during the period of investigation within Benue State having unexplained fever (≥ 38ºC) for one week or more plus 1 of the following:
1. No response to standard treatment for most likely cause of fever (malaria, typhoid fever)
2. Readmitted within 3 weeks of inpatient care for an illness with fever,
3. Edema or bleeding
4. Sore throat and retrosternal pain/vomiting
5. Spontaneous abortion following fever
6. Hearing loss following fever
However, any person with a laboratory detected Lassa virus specific sequence using Polymerase Chain Reaction (PCR) is confirmed cases.
Case Finding/Contact Tracing
Active case search was conducted in Markurdi metropolises. Special targets include health facilities which treated confirmed and suspect cases, as well as their residential and business premises. All cases were identified based on the adopted case definition (above). Identified cases were line-listed and categorized into Suspected and Confirmed. A Suspected case is an individual that meets the clinical and epidemiological linkage criteria. Confirmed case is anyone that meets both clinical and laboratory criterion. Individuals with potential direct exposure to Lassa virus through contact with a case were risk assessed. Based on the assessment, they LF were categorised using Holmes et al. [12] method as; -
• No risk category: No direct contact with case or his potentially infectious material (e.g. shared a room with case)
• Low risk category: Close direct contact with case (e.g. routine medical/nursing care and handling of case laboratory specimen wearing PPE), and beddings and other contaminable formites.
• High risk category: Unprotected exposure of skin or mucosal membranes (e.g. mucosal exposure to splashes, needle-stick injury) to blood or body fluid, including unprotected handling of laboratory specimen.
Data Collection: Type and Source
Both qualitative and quantitative data were collected for the investigation. The Medical records and case notes were reviewed at all health facilities where cases were managed. Then active case search was done at the residence, business premises and health care facilities of identified cases. Details obtained were used to build a line-list. Interviewer-administered questionnaire was used in accessing the infection control capacity of Health care facilities involved in the management of confirmed and suspected cases. The head of Infection control team of the Benue State University Teaching Hospital (BSUTH) Infection control Team. Blood samples for viral studies were taken from the cases/contacts and sent to the Lassa Fever Research and Control Institute in Irrua, Edo State. Sensitization workshop was organized and conducted for the health care workers at the BSUTH college of Health Science auditorium and Lassa fever fact sheets were produced and distributed at households and business premises.
Laboratory Investigation
Blood samples from cases and suspects are collected into EDTA anticoagulant bottles and refrigerated (prior to transportation) or transported immediately in a reverse cold chain transport unit to Specialist Teaching Hospital, Irua, Edo State. At Irua, the samples are subjected to reverse transcription polymerase chain reaction (RTPCR), specifically targeting the glycoprotein precursor (GP) gene. Average turn-around time for samples sent to Irua during this outbreak was 3 days.
Data Processing and Analysis
Data needed for descriptive epidemiology in this investigation was entered a spread sheet and analyzed using Microsoft excel. Other information from questionnaire on hospital infection control capacity was entered Epi-info and analyzed using same.
Results
For clarity, the results will be presented and arrange in two different parts. The specific case findings as part I while the overall epidemic report on the disease as part II.
Part I: Case finding
An unrecorded incident
Mr. CO, a 28th year old male who sells mobile phone accessories opposite Tito gate in old GRA Makurdi Benue State, Nigeria became acutely febrile. He was rushed home and admitted (presumably) at Ebonyi State University Teaching Hospital Abakiliki, Ebonyi State, Nigeria. He passed away a day after arriving Abakiliki and was buried three days after death. No records of CO’s symptoms exist beyond the testimony of his business colleagues who after being sensitized, concluded that he presented symptoms like acute febrile illness, headache, vomiting, seizures and within his last hours, unconsciousness.
Index case
Mr. MN, a 32 year old male also sold mobile phone accessories opposite Tito gate, at railway area, old GRA Makurdi. He also is from Ebonyi State, Nigeria and is active among a communal group of Ebonyi state indigenes who do business opposite Tito gate. He joined others home for the burial of CO in Ebonyi State and returned thereafter. He took ill presented at the hospital and was given intravenous infusion at Divine Love hospital Makurdi and sent home. Two days later he was re-admitted at Divine Love hospital, Makurdi and treated with antimalaria and antibiotics on suspicion of malaria/enteric fever. With worsening symptoms including fever, vomiting and convulsion, he was referred to Benue State University Teaching Hospital (BSUTH). He died a day after continuous manifestation of symptoms; as high grade fever, chest pain, generalized abdominal pain with swelling and yellowness of the eyes, post-pandrial vomiting, and minimal bleeding from mouth. Without suspicion of Lassa and no definitive laboratory diagnosis, Mr. MN was deposited in Bishop Murray Hospital mortuary and later buried at Umuche, Umuigboke, Ugwulagwu in Ohaozara LGA of Ebonyi State. Mr. MN’s linkage with the Lassa outbreak was made after contact tracing revealed that he was treated by the first confirmed case.
First confirmed case
MO is a medical doctor and proprietor of a private clinic in Markudi. He is 55 years old. MO treated a patient with acute febrile illness, recognised as Mr. MN and referred him to BSUTH. Six days after he treated a patient MN he presented himself for admission for symptoms including persistent high grade pyrexia of 3 days duration, Abdominal pain, cough and chest pain. He self-administered antibiotics and antimalarials without relief, Temperature remained above 380ºC and was told to have been hypertensive for 3 years. The laboratory results from the Teaching Hospital shown PCV 52%, WBC Normal, Hyponatraemia Na+ 124 mmol/L, Azotaemia (Urea 16.2 mmol/L, Cr 614) and HbsAg, Anti- HCV and RVST were not reactive. The treatments given were intravenous fluid IVF, Antibiotics and Antimalaria drugs. At second day of admission, the patient was now anuric for 24 h (<30 ml/24 h), rising temperature (T 38.7ºC which later increased to 39.8ºC), dyspnoeic, developed subconjuctival haemorrhage and started bleeding from injection sites, BP 70/40 mmHg (hypotensive) and became unconscious. The hospital now commenced on intranasal Oxygen. Based on the assessment by the Consultant Physician indicated multi organ dysfunction (renal failure, circulatory collapse and bleeding diathesis) and concluded on the Possibility of Viral Haemorrhagic fever (LF). The State Epidemiologist was immediately informed and was asked to bring Ribavirin injection, which he did. Effort was made to resuscitate him by inviting Nephrologists to review and placed him under closed and strict monitoring. The resuscitation was unsuccessful and the patient died at 2 pm three days after manifestation of symptoms and from complications exacerbated by pre-existing medical conditions. No post-mortem examination was undertaken. The blood sample taken was sent to Irua Specialist Teaching Hospital (ISTH) for where LF was confirmed through RT-PCR.
Suspected case 1
The Benue State Chief Epidemiologist had notified the FMOH of two cases of LF. Case one was MO as narrated above while the second is described here as MK. MK is a 24 year old student of Benue State Polytechnic Ugbokolo. She left Ugbokolo for vacation at her home in Makurdi, she fell ill and was admitted at Grace Cottage Hospital, Makurdi. Her case note indicated the following symptoms; fever (Temp=39.3ºC), dizziness and nausea and palpable tenderness in right abdomen. She responded mildly to antibiotic treatment on suspicion of enteric fever and was discharged to continue antibiotics at home. She returned to the hospital because the body temperature spiked again and she was constantly vomiting. Further laboratory investigation was negative for HIV, Hepatitis B and Hepatitis C. She was later referred to BSUTH because she failed to improve. On review, she had persistent high grade pyrexia, nausea. She developed facial puffiness 2 days prior to presentation and reduced urine output. She also had difficulty with breathing, cough and haemoptysis. She developed diarrhoea on the ward and Chest pain but now responding to ribavirin treatment.
Other cases
AE, a 31 year old male was admitted with suggestive symptoms and kept in an isolated treatment room in BSUTH. Sample has been collected and sent to Irua for confirmation. Patient is already getting ribavirin and is stable.
Descriptive epidemiology
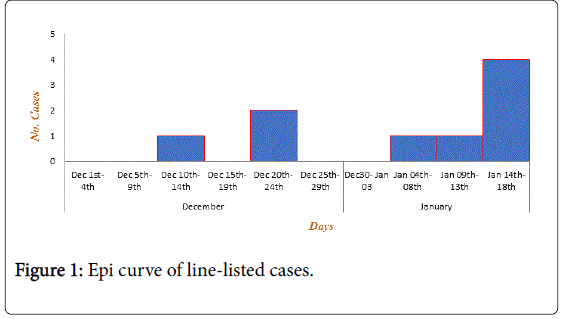
As seen in Figure 1 Eight (8) cases where seen during investigation. One (1) was confirmed, two (2) fatal cases could not be tested before death and five (5) results are being awaited. Case fatality rate is 37.5%. Over 50% of the cases are aged between 25-40 years. Mean age of cases is 26 (SD ± 15.6) years. Median age is 26 year with range 1-55years.
Five of the eight cases (62.5%) are males. 100% of patients live in Markudi but 86.5% are Ibo settlers who are residing in Makurdi for business. Seven (7) cases representing 86.5% live at the railway area of Old GRA in Makurdi metropolis.
Out of the 53 contacts that were assessed for risk, 25 (47.2%) were categorized as no risk, 25 (47.2%) were categorized as low risk, while 3 (5.6%) were high risk contacts. A mixture of low and high risk contacts was started on Ribavirin based on availability and need. All contacts on low risk category were put on surveillance while samples of high risk cases were scheduled for collection and transport to Specialist Teaching Hospital Irua.
Two of the five samples sent to Irua on 17th January were confirmed Lassa fever PCR positive, bringing the total confirmed cases to (3) three (Figure 2).
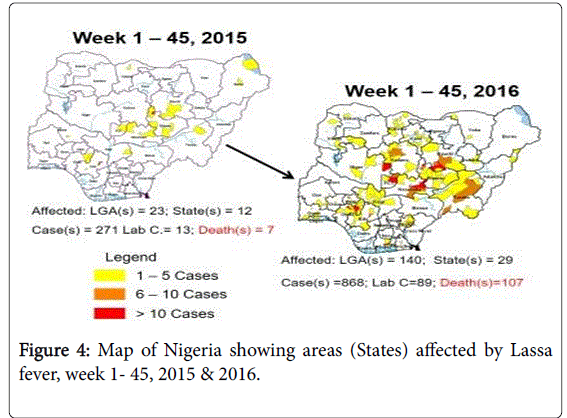
Part II: The overall epidemic report on the disease
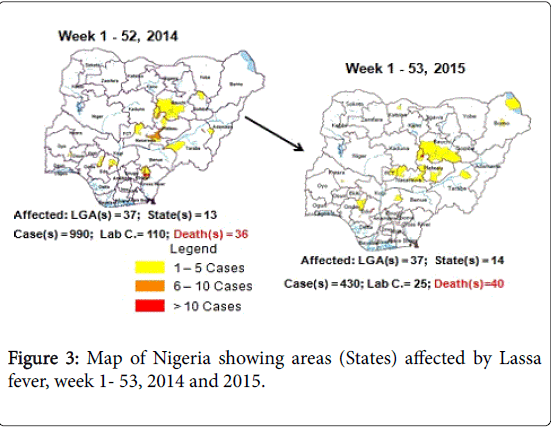
Four suspected cases of Lassa fever and 1 death case fatality rate (CFR, 25%) were reported from 3 LGA (3 States) in week 45, 2016 compared with 1 case from Jos North LGA (Plateau State) at the same period in 2015 (Figure 3). Laboratory results of the 4 suspected were negative for Lassa fever and other viral haemorrhagic fever (VHFs). Between weeks 1 and 45 (2016), 868 suspected Lassa fever cases with 89 lab-confirmed and 107 deaths Case Fatality Rate (CFR, 12.33%) from 140 LGAs (29 States) were reported compared with 271 suspected cases with 13 lab-confirmed and seven (7) deaths (CFR, 2.58%) from 23 LGAs (12 States) at the same period in 2015 (Figure 3).
Between weeks 1 and 53 2015, 430 suspected Lassa fever cases with 25 lab-confirmed and 40 deaths (CFR, 9.30%) from 37 LGAs (14 States and FCT) were reported compared with 990 suspected cases with 110 lab-confirmed and 36 deaths (CFR, 3.64%) from 37 LGAs (13 States) at the same period in 2014 (Figure 4). In 2013, total of 1191 suspected of Lassa fever cases was reported with 35 deaths with a case fatality of (2.94%) which is much lower than 2012 figure of case fatality of 6.93% (Table 1).
| Variables | 2012 | 2013 | 2014 | 2015 | 2016 | Total |
|---|---|---|---|---|---|---|
| Cases | 1572 | 1191 | 990 | 430 | 868 | 5051 |
| Death | 109 | 35 | 36 | 40 | 107 | 3891 |
| CFR | 6.93% | 2.94% | 3.64% | 9.30% | 12.33% | 77.03% |
Table 1: Lassa fever morbidity and mortality from 2012 to 2016.
Discussion
Lassa fever outbreak described was successfully contained by a multidisciplinary collaboration between, the Benue State MoH task force, ISTH, and support from the FMoH. The spread of LF in the hospital and community was limited through the outbreak response efforts, which substantially contributed to this containment. The backbone of the response strategies was a strong collaboration of different sectors, resulting in coordinated efforts and resource mobilization. Also, the Benue State government provided leadership with support from the FMoH. Implementation relied substantially on surveillance for cases and contacts, case management and infection control, and availability of a Lassa virus diagnostic facility in the country, as well as effective public information and communication. Some of these approaches [13] have been adopted previously to contain [14] other outbreaks Ali et al. [15] of viral hemorrhagic Yilmaz et al. [16].
This study confirmed that Nigeria is experiencing an outbreak and resurgence of LF, with a high number of cases and deaths as well as a large geographical distribution Carey et al. [17]. At the beginning of February, statistics by the Nigeria Center for Disease Control (NCDC), the number outbreak has spread widely WHO, 2016 [18], there have been cases in 19 states. Study have showed that LF, endemic in Nigeria and other West-African countries, is an acute viral hemorrhagic illness Asogun et al. [19], which is mainly transmitted by rodents. As found in this study symptoms include fever, vomiting and diarrhoea. In severe cases, the disease also causes bleedings. Morbidity and mortality due to Lassa fever recorded over a period of five years was higher that another West Africa region WHO, 2005 [7].
There are a several factors that have shaped the current and previous outbreaks. Media’s focus on the role of rodents in the transmission of LF in addition to advocacy and community information and mobilization helped to improve awareness, health seeking behaviour and response to FL for referral to tertiary center as previously documented Pulse, 2016 [20]. As found in this study by Badaru et al. [21] many Nigerians are now aware that “rat infected food stuff” is a source for LF infection. Evidence from this study supported the epidemiology of diseases on human to human transmission of disease which play a less important role compared to zoonotic transmission. During the current outbreak of LF in Nigeria, much attention has been paid to human-to-human transmission, which was not well documented in previous outbreak in Nigeria. Inadequate hospital infrastructure and equipment are likely to have caused the infection of these health workers. At the onset of the outbreak, there was no isolation ward in the hospital where the index cases had been treated. Other factors that facilitated the transmission include non-availability of drugs ribavirin, long travelling time to get to accredited center the Institute of Lassa Fever Research and Control in Irrua, Edo State.
This puts the health workers, their families and the wider community at risk of secondary infections, inundation, other study also revealed significant knowledge gaps concerning LF among primary care providers in a LF endemic suburban community Andrew et al. [22].
Despite the above, the observation that almost all the cases were of Io ethnic stock negates the premise that the infection could have arisen through consumption of rat, which is a common delicacy among the Idoma and Tiv people of Benue State. The nature of the Epidemic curve shows that the epidemic is still on the up-swing and more cases are possible. The curve also indicates that the epidemics might be from a common intermittent source, a fact that is supported by the narrative linkage of the index case with the only confirmed case in the epidemics. In most of the previous out breaks in Nigeria, nosocomial transmission has been a major source of morbidity and mortality among health care workers. Despite the loss of one health worker in this outbreak, it is noteworthy that none of the Health care workers at BSUTH to whom most cases were referred to remained asymptomatic. This could be a signal to the improved barrier nursing methods adopted in care and support of patients [23-25].
Conclusion
Lassa fever is an endemic in Nigeria and resurgences of the disease is fast spreading to other part of the country, all health facility and institution should activate surveillance systems, maintain universal precaution, embark on community mobilization to ensure that the resurgence does not escalate to epidemic proportion.
References
- Viral Haemorrhagic Fever (VHFC) (2007) Fevers consortium: Lassa fever.
- Centers for Disease Control and Prevention (CDC) (2004) Imported Lassa fever--New Jersey, 2004. MMWR Morb Mortal Wkly Rep 53: 894-897.
- Ogbu O, Ajuluchukwu E, Uneke CJ (2007) Lassa fever in West African sub-region: An overview. J Vector Borne Dis 44: 1-11.
- Coker AO, Isokpehi RD, Thomas BN, Fagbenro-Beyioku AF, Omilabu SA (2000) Zoonotic infections in Nigeria: Overview from a medical perspective. Acta Trop 76: 59-63.
- Quick reference Guide (2017) Lassa fever: National response team.
- Weekly Epidemiology Report (2015) Nigeria centre for disease control.
- World Health Organization (2005) Update on lassa fever in West Africa.
- Fisher-Hoch SP, Tomori O, Nasidi A, Perez-Oronoz GI, Fakile Y, et al. (2009) Review of cases of nosocomial Lassa fever in Nigeria: The high price of poor medical practice. BMJ 311: 857-859.
- Richmond JK, Baglole DJ (2003) Lassa fever: Epidemiology, clinical features and social consequences. BMJ 327: 1271-1275.
- Kernéis S, Koivogui L, Magassouba N, Koulemou K, Lewis R, et al. (2009) Prevalence and risk factors of lassa seropositivity in inhabitants of the forest region of Guinea: A cross-sectional study. PLoS Negl Trop Dis 3: e548.
- Aper JA, Agbehi SI (2010) Pattern of domestic water supply in ugbokolo community in Benue state, Nigeria. International Journal of Water and Soil Resources Research 1: 72-82.
- Holmes GP, McCormick JB, Trock SC, Chase RA, Lewis SM, et al. (1990) Lassa fever in the United States. Investigation of a case and new guidelines for management. N Engl J Med 323: 1120-1123.
- Borchert M, Mutyaba I, Van Kerkhove MD, Lutwama J, Luwaga H, Bisoborwa G, et al. (2011) Ebola haemorrhagic fever outbreak in Masindi District, Uganda: Outbreak description and lessons learned. BMC Infect Dis 11: 357.
- Lamunu M, Lutwama JJ, Kamugisha J, Opio A, Nambooze J, et al. (2004) Containing a haemorrhagic fever epidemic: The Ebola experience in Uganda (October 2000-January 2001). Int J Infect Dis 8: 27-37.
- Ali F, Saleem T, Khalid U, Mehmood SF, Jamil B (2010) Crimean-Congo hemorrhagic fever in a dengue-endemic region: Lessons for the future. J Infect Dev Ctries 4: 459-463.
- Yilmaz GR, Buzgan T, Irmak H, Safran A, Uzun R, et al. (2009) The epidemiology of Crimean-Congo hemorrhagic fever in Turkey, 2002-2007. Int J Infect Dis 13: 380-386.
- Carey D, Kemp G, White H, Pinneo L, Addy R, et al. (1972) Lassa fever epidemiological aspects of the 1970 epidemic, Jos, Nigeria. Trans R Soc Trop Med Hyg 66: 402âÂ?Â?408
- Minicuci N, Naidoo N, Chatterji S, et al. (2016) Data resource profile: Cross-national and cross-study sociodemographic and health-related harmonized domains from SAGE plus ELSA, HRS and SHARE (SAGE+, Wave 1). Int J Epidemiol 45: 1403-1403j.
- Asogun D, Okokhere P, Tobin E, Okogbenin SA, Akpede G, et al. (2012) Lassa fever practice challenges in Nigeria. Int J Infect Dis 16: e69.
- http://pulse.ng/health/lassa-fever-physician-advocates-war-against-rats-id4636312.html
- Omilabu SA, Badaru SO, Okokhere P, Asogun D, Drosten C, et al. (2005) Lassa fever, Nigeria, 2003 and 2004. Emerg Infect Dis 11: 1642-1644.
- Lo Iacono G, Cunningham AA, Fichet-Calvet E, Garry RF, Grant DS, et al. (2015) Using modelling to disentangle the relative contributions of zoonotic and anthroponotic transmission: The case of lassa fever. PLoS Negl Trop Dis 9: e3398.
- le Clercq CM, Mooi RJ, Winkens B, Salden BN, Bakker CM, et al. (2016) Temporal trends and variability of colonoscopy performance in a gastroenterology practice. Endoscopy 48: 248-255.
- World Health Organization (2010) Time to put Ebola in context.
- http://dailypost.ng/2016/01/25/lassa-fever-4400-rats-killed-in-six-lagos-markets/
Relevant Topics
- Chronic Disease Management
- Community Based Nursing
- Community Health Assessment
- Community Health Nursing Care
- Community Nursing
- Community Nursing Care
- Community Nursing Diagnosis
- Community Nursing Intervention
- Core Functions Of Public Health Nursing
- Epidemiology
- Epidemiology in community nursing
- Health education
- Health Equity
- Health Promotion
- History Of Public Health Nursing
- Nursing Public Health
- Public Health Nursing
- Risk Factors And Burnout And Public Health Nursing
- Risk Factors and Burnout and Public Health Nursing
Recommended Journals
- Epidemiology journal
- Global Journal of Nursing & Forensic Studies
- Global Nursing & Forensic Studies Journal
- global journal of nursing & forensic studies
- journal of community medicine& health education
- journal of community medicine& health education
- Palliative Care & Medicine journal
- journal of pregnancy and child health
Article Tools
Article Usage
- Total views: 10010
- [From(publication date):
May-2017 - Jul 09, 2025] - Breakdown by view type
- HTML page views : 8652
- PDF downloads : 1358