Laryngeal Manifestations in Recurrent Respiratory Papillomatosis - A Descriptive Study
Received: 03-Oct-2021 / Editor assigned: 01-Jan-1970 / Reviewed: 01-Jan-1970 / Revised: 01-Jan-1970 / Accepted Date: 20-Nov-2021 / Published Date: 27-Nov-2021
Abstract
Aim: Recurrent respiratory papillomatosis in children is common but potentially life- threatening benign tumor of the respiratory tract with laryngeal predilection. The diagnosis of recurrent respiratory papillomatosis may be challenging unless there is a high index of suspicion and awareness of the variable presentations.
Methods: Children with voice change with or without stridor was examined with Laryngoscopy and further investigated for Microlaryngeal Surgery for excision of the warty lesion and screening of the mothers for HPV was carried out.
Results: Five patients, aged 2 to 14 years, were diagnosed with recurrent respiratory papillomatosis. Once the diagnosis of recurrent respiratory papillomatosis was made, recurring surgical excision of papillomata initiated.
Conclusion: Recurrent respiratory papillomatosis in any child presenting with voice change with or without stridor should be considered for prompt management and follow-up.
Key words
Recurrent respiratory Papillomatosis; Human papilloma virus; Juvenile onset RRP; Adult onset RRP; Vocal cords
Introduction
Recurrent respiratory Papillomatosis (RRP) is caused by a viral agent –the Human papilloma virus (HPV) of which serotype 6 and 11 are the most common types.
SITE: Exophytic wart–like growth that could be found anywhere from the nose to the lungs, with the larynx as most common site of occurrence. Although the condition is a common benign neoplasm of the larynx among children and a frequent cause of childhood hoarseness some with spontaneous regression and others suffering aggressive papilloma growth requiring multiple surgical procedure and medication for relief. It is associated with a less than one percent risk of malignant transformation [1].
Categories:
1. Juvenile onset RRP (JORRP) – Before the age of 12 years.
2. Adult onset RRP (AORRP)
Prevalence 2.59/100 000 and 1.6/100 000 was found among paediatric population Despite the low prevalence of RRP, it has been shown to have significant economic and emotional burden on the patients as they go through the cycle of recurrence and surgeries.
Case Series
Case 1
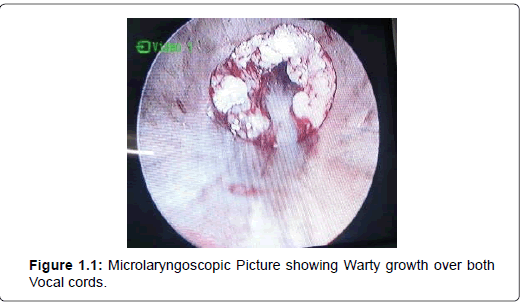
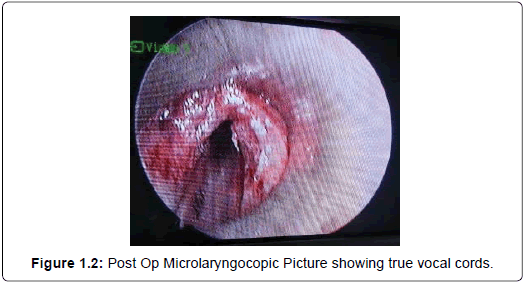
A 14 year old male child was brought by his mother with c\o respiratory distress since 8 days She gives history of previous episodes of hoarseness of voice for which four times surgery has been done with diagnosed case of recurrent respiratory papillomatosis On examination : The e\o warty growth occluding the glottic chink involving both the vocal cords were seen (Figure 1.1). Patient was in stridor and patient was shifted to emergency ot and was operated for ML scopy (Figure 1.2) Patient was referred for Homeopathic mode of management for Thuja Therapy.
Case 2
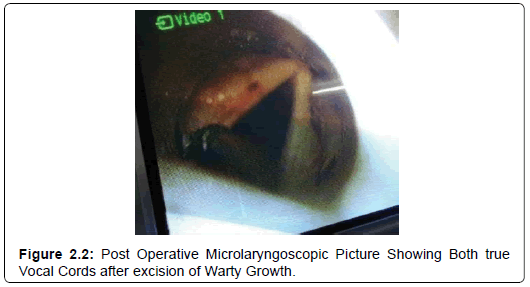
A 4 year old (Figure 2.1) female child brought by parent with c\o: hoarseness in voice since 1 year .Parent gives history of immunisation till date and no h\o respiratory distress. No h\o bronchial asthma\ epilepsy. On examination: Patient not in distress,e\o hoarseness of voice,ENT: NAD,VL scopy: s\o B|L vocal cord growth ? Warty with adequate glottic chink (Figure 2.2) Patient was diagnosed as Respiratory papillomatosis and was worked up for Microlaryngeal surgery (MLS). Patient underwent MLS and the growth was excised and sent for HPE. HPR came to be Respiratory Papillomatosis [2, 3].
Case 3
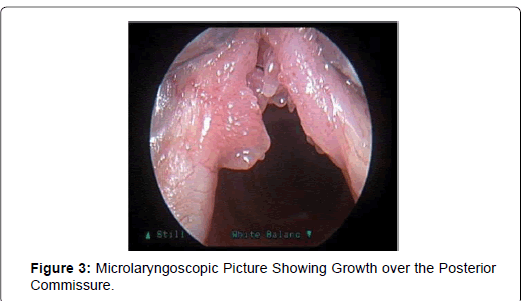
A 8 year old female child brought by parent with c\o : hoarseness in voice since 18 months .Parent gives history of immunisation till date and no h\o respiratory distress . No h\o bronchial asthma\epilepsy.On examination: Patient not in distress, e\o hoarseness of voice, ENT: NAD, VL scopy: s\o B|L vocal cord growth ? warty with adequate glottic chink involving the posterior commissure (Figure 3) .Patient was diagnosed as Respiratory papillomatosis and was worked up for Microlaryngeal surgery(MLS).Patient underwent MLS and the growth was excised and sent for HPE. HPR came to be Respiratory Papillomatosis.
Case 4
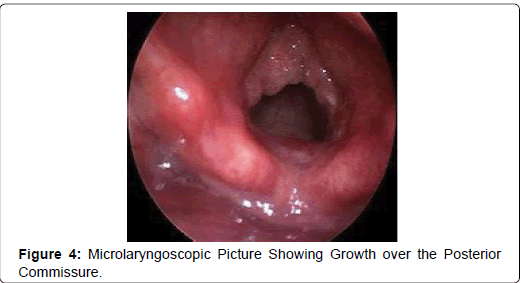
A 11 year old male child brought by parent with c\o: hoarseness in voice since 3 months. Parent gives history of immunisation till date and no h\o respiratory distress . No h\o bronchial asthma\epilepsy. On examination :Patient not in distress ,e\o hoarseness of voice ENT: NAD,VL scopy: s\o B|L vocal cord growth ? warty with adequate glottic chink(Figure 4).Patient was diagnosed as Respiratory papillomatosis and was worked up for Microlaryngeal surgery(MLS). Patient underwent MLS and the growth was excised and sent for HPE. HPR came to be Respiratory Papillomatosis.
Case 5
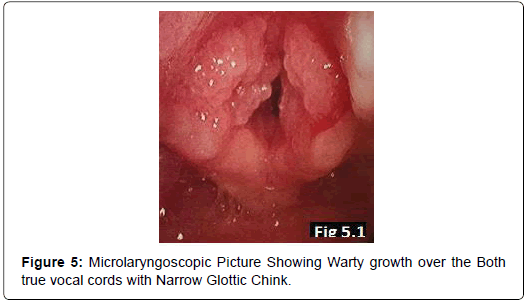
A 9 year old female child brought by parent with c\o: hoarseness in voice since 1 year with respiratory distress since 3 days .Parent gives history of immunisation till date and no h\o respiratory distress. No h\o bronchial asthma\epilepsy. On examination: Patient in respiratory distress, e\o hoarseness of voice +, ENT: NAD,VL scopy: s\o B|L vocal cord growth ? warty with narrow glottic chink almost obstructing the airway (Figure 5).Patient was diagnosed as Respiratory papillomatosis and was worked up for Microlaryngeal surgery(MLS). Patient underwent MLS and the growth was excised and sent for HPE. HPR came to be Respiratory Papillomatosis. All patients mother’s were screened for Vaginal HPV by Vaginal Smear and results came out to be Vaginal smear Negative For HPV [4].
Discussion
RRP was first described by Sir Morrell Mackenzie in 1800s; he recognized it as a distinct lesion of the larynx in children. It was with modern genetic technology in 1990’s that HPV was confirmed as the causative agent. Over a 100 serotype of HPV have been identified, with serotypes sometimes classified by anatomical sites; namely anogenital, nongenital cutaneous and non- genital mucosal. The HPV 6 and 11 can cause both genital warts and laryngeal Papillomatosis. Some are also classified as ‘high risk’ type when it is associated with malignant transformation or ‘low risk’ type manifesting as warts (Condylomatosis), with low risk for malignancy.The low risk serotypes 6 and 11 are the most common types found to be involved as causative agent of RRP. The aetiology of JORRP is generally agreed to be vertical transmission either in pregnancy or at child delivery, especially when a mother has frank condylomatosis or is actively shedding disease from a recent HPV infection. Three major risk factors that have been identified for development of JORRP include; teenage mother, vaginal delivery and first born. Gender: Males = Females (0.75-4.3/1,00,000) The age of occurrence reported ranges from one day to 84 years; however a bimodal distribution is seen with the peak age range of juvenile form at two to four years and that of the adult at 20 to 40 years [5].
Extra- laryngeal spread of RRP occurs in 30% of children and 16% of adult, which is an indication of progressive disease common with the JORRP type. Other symptoms identified includes, c h r o n i c cough, paroxysms of choking, recurrent pneumonia, failure to thrive, dyspnoea, dysphasia and acute life threatening event. At time of presentation it is important to identify respiratory distress for immediate transfer of patient to emergency room or operating room to ensure that a safe airway is established.
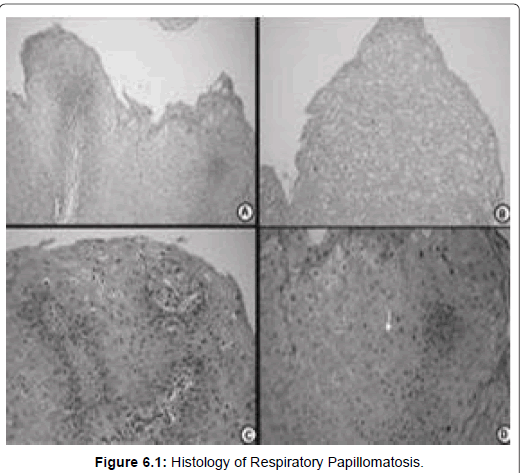
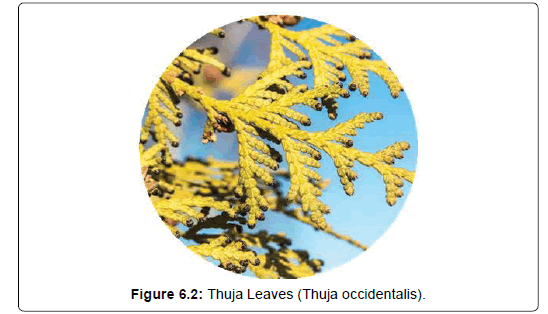
A laryngoscopic examination should be performed on stable patient. This is challenging in children and requires examination under anaesthesia in operating room. Histological findings in biopsied lesion show growth of keratinized squamous epithelium overlying a fibrovascular core. Koliocyte, vacuolated cells with clear cytoplasmic inclusion (Figure 6.1) are seen, with variable degrees of dysplasia and metaplasia. Surgery is the mainstay of treatment,with several surgical methods that include direct resection with operating microscopes, endoscopic debulking with microdebriders, laser ablative surgery using CO2 , Nd: YAG laser, pulse dye laser and most recently the Shaver technology.The list of adjuvant medical therapy include; Thuja therapy (Figure 6.2), antiviral agents (acyclovir, ribavarin, cidofovir); interferon, retinoid (oral metabolite or analogue of vitamin A), photodynamic therapy, zinc, antireflux medication, cyclooxygease -2- inhibitor, methotrexate, preventive vaccine (mumps, MMR, quadrivalent HPV, heat shock protein E7) and gene therapy. The economic and medical burden of RRP makes prevention of paramount importance [6]. There are two HPV vaccines available for usage. These are Gardasil R from Merck, and CervirixR from GlaxoSmithKline (GSK).
Conclusion
RRP is a chronic disease caused by HPV characterized by cauliflower-like warty growth in the aerodigestive tract. The lesion is commonly found in the larynx.Hoarseness of voice is the commonest symptom and patient can present with acute life threatening airway obstruction. Surgery is mainstay of treatment but does not provide cure. Several adjuvant medical treatments are required for frequent relapse, lesions with rapid re-growth causing airway obstruction and those in remote site. RRP cause substantial emotional and economic burden in patient and the family as well as create management challenge to the medical practitioner. The greatest promise for future prevention rest with the development of an HPV vaccine, and hence reduced management challenges for HPV- associated diseases. Promote awareness among clinicians, especially general practitioners (GPs) regarding juvenile recurrent respiratory papillomatosis (JRRP) as a rare disease with varied presentation and tendency to masquerade as asthma. Highlight the implications of high mortality and morbidity with delayed diagnosis and mismanagement of this rare disorder. Emphasise the need for GPs to maintain high index of suspicion in ruling out this devastating disease when encountering any child with airway problem in particular the need to obtain relevant history of symptoms that may suggest JRRP.
Acknowledgments
Nil
Funding
The author(s) received no financial support for the research, authorship, and/ or publication of this article.
Conflicts of Interest
The author(s) declare(s) that there is no conflict of interest.
References
- Ghosh SK, Chattopadhyay S, Bora H, Mukherjee PB (2001) Microlaryngoscopic study of 100 cases of hoarseness of voice. Indian J Otolaryngol Head Neck Surg 53: 270–272
- Hemant Chopra, Minisha Kapoor (1997) Study of benign glottic lesions undergoing microlaryngeal surgery. Indian J Otolaryngol Head Neck Surg 49: 276- 279
- Kimberlin DW (2004) Current status of antiviral therapy for juvenile_onset recurrent respiratory papillomatosis. Antiviral Res 63: 141-151
- Rahbar R, Shapshay SM, Healy GB (2001) Mitomycin: Effects on Laryngeal and tracheal stenosis,benefits and complications. Ann Otol Rhinol Laryngol 110: 1-6.
- Veen EJ, Dikkers FG (2010) Topical use of MMC in the upper aerodigestive tract: a review on the side effects. Oto-Rhino-Laryngol 267: 327-334
- Dedo HH, Jackler RK (1982) Laryngeal papilloma: results of treatment with the CO2 laser and podophyllum.Ann Oto Rhinol Laryngol 91: 425-430
Citation: Jayakumar V (2021) Laryngeal Manifestations in Recurrent Respiratory Papillomatosis – A Descriptive Study. Otolaryngol (Sunnyvale) S7: 005.
Copyright: © 2021 Jayakumar V. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 1731
- [From(publication date): 0-2021 - Apr 07, 2025]
- Breakdown by view type
- HTML page views: 1247
- PDF downloads: 484