Research Article Open Access
Laparoscopic Adjustable Gastric Banding is more Effective in Body Mass Index<40 Kg/m2 for Short Term Weight Loss
Ooi Tong Li1, Hnin Hnin Oo1, Lucy Kong RN2, Anton Cheng2 and Kee Yuan Ngiam3*1Yong Loo Lin School of Medicine, National University of Singapore, Singapore
2Department of Surgery, Khoo Teck Puat Hospital, 90 Yishun Central, Singapore
3Division of Surgery, University Surgical Cluster, National University Hospital, Singapore
- *Corresponding Author:
- Ngiam Kee Yuan
Department of Surgery, National University Hospital Singapore
1E Kent Ridge Road, NUHS Tower Block, Level 8-119228, Singapore
Tel: +65 6779 5555
Fax: +65 6777 8427
E-mail: kee_yuan_ngiam@nuhs.edu.sg
Received date: July 20, 2015; Accepted date: August 22, 2016; Published date: August 25, 2016
Citation: OOi TL, Oo HH, Kong RNL, Cheng A, Ngiam YK (2016) Laparoscopic Adjustable Gastric Banding is more Effective in Body Mass Index<40 Kg/m2 for Short Term Weight Loss. J Obes Weight Loss Ther 6:317. doi:10.4172/2165-7904.1000317
Copyright: © 2016 Ooi TL, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Obesity & Weight Loss Therapy
Abstract
Background: Obesity is a global health problem. Laparoscopic Adjustable Gastric Banding (LAGB) is a type of bariatric surgery that is effective for weight loss and control of co-morbidities. Long-term results of LAGB in different obesity groups have been widely studied in Western populations but not in a multi-racial Asian population such as in Singapore. This paper aims to compare the outcomes of LAGB and describe its complications in obese Singaporean patients with Body Mass Index (BMI) <40 kg/m2 vs BMI ≥ 40 kg/m2. Methods: 360 patients underwent LAGB surgery at two institutions in Singapore from June 2001 to July 2011. The patients were followed up for ten years post-surgery, out of which data from five years post-LAGB were analysed. Percentage weight loss (%WL), percentage excess weight loss (%EWL), morbidity and mortality were explored in both groups retrospectively. Results: Patients in Group A (BMI <40 kg/m2) were compared with patients in Group B (BMI ≥ 40 kg/m2). A significant difference in %EWL between the groups was noted at one year post-surgery where Group A achieved 30% EWL while Group B achieved 20.8% EWL (p-value=0.01). No other significant differences in %WL and %EWL between the two groups were noted in subsequent years (p-value >0.05). At the end of five years follow-up, Group A achieved 18.8%WL and 52.6% EWL while Group B achieved 18.7% WL and 34.9% EWL. In both groups, peak %WL was attained at 3 to 4 year follow-up before it tapered. A total of 90 patients (25%) developed complications during the study, with seven mortalities on follow-up, out of which two were band-related. Conclusion: LAGB is an effective bariatric surgical option for weight loss in obese Singaporean patients over a short-term but it is more beneficial for patients with BMI <40 kg/m2.
Keywords
Laparoscopic adjustable gastric banding (LAGB); Body mass index (BMI); Bariatric surgery; Obesity; Asian
Introduction
Obesity is rapidly becoming one of the world’s most prevalent public healthcare problems. Obesity rate in Singapore has risen to 10.8% in the 2010 National Health Survey Statistics [1] from 6.9% in its 2004 Survey [2]. In addition, research has shown that Asian patients have a higher proportion of truncal obesity compared to Caucasians, which predisposes obese Singaporeans to various metabolic diseases [3]. Obesity is a major risk factor for diseases such as type 2 diabetes mellitus (T2DM), hypertension (HPT) and coronary heart disease (CAD), thereby increasing the mortality rate [4]. As such, obesity is a major healthcare burden to the country and is set to increase in the years to come. Various modes of bariatric surgeries have been performed in obese patients seeking weight loss. Public hospitals in Singapore performed 154 bariatric surgeries in 2011, up from 66 cases in 2009 [5]. In particular, laparoscopic adjustable gastric banding (LAGB) was amongst the earliest bariatric operations performed in Singapore due to its reversibility and early evidence of efficacy. This method of surgery provides rapid short-term weight loss and significant moderate weight loss up to 10 years, which is more effective than non-surgical alternatives in patients with lower BMIs, as described by Dixon and O 'Brien in their systematic review [6,7]. Recent studies concluded that weight loss is able to decrease the risk of certain co-morbidities in obese patients. Remission of T2DM in patients following various types of bariatric surgery is well documented. LAGB has also shown similar long-term benefits in numerous Western populations [7-12]. However, little is known about the effects of LAGB in Asian populations. The aim of this study is to compare the outcomes of LAGB in two groups of obese Singaporean patients with preoperative BMI <40 kg/m2 and BMI ≥ 40 kg/m2 over five years and describe the operative complications.
Methods
A retrospective analysis was carried out on 360 patients consisting of 139 males and 221 females who underwent LAGB surgery at two institutions in Singapore from June 2001 and July 2011. Patients were followed up for ten years post-LAGB but only data from five-year follow-up were used for statistical analysis.
Patient Selection
Inclusion criteria for LAGB surgery for this study comprise (1) a previous failed attempt at losing weight using diets or medications, (2) BMI >32.5 kg/m2 with co-morbidities (with medical co-morbidities/ complications of obesity such as T2DM, HPT and Obstructive Sleep Apnoea (OSA)) or (3) >37.5 kg/m2 without co-morbidities. Patients are aged between 18 and 65 years old. Surgical risks were explained and informed consent was obtained from all patients. Participants must demonstrate commitment to lifestyle modifications after the surgery. Patients with severe organ dysfunction, psychiatric disorders and substance abuse or eating disorders were excluded from the study. The criteria for surgery during the study period were based on the Society of American Gastroenterological surgeons (SAGES) and the Ministry of Health of Singapore Clinical Practice guidelines for Obesity 2004.
Pre-operative preparation
Pre-operative workup including blood tests and radiological investigations were conducted for all patients. In addition, when there were indications, sleep study, ultrasonography of the hepatobiliary system, barium swallow and oesophagogastrodudenoscopy were conducted as well. Patients were counselled for possible laparoscopic cholecystectomy during the operation should there be gallstones discovered on ultrasonography and if the patient was symptomatic. Nutritional assessment and counselling were carried out by dieticians. For patients with fatty liver on ultrasonography, a trial of very low caloric diet (VLCD) was started for 2 weeks. This diet aimed to reduce the size of the liver to facilitate visualisation of the diaphragmatic crura intra-operatively. The care of bariatric patients was coordinated in a multidisciplinary team including a care manager who would follow up and monitor progress of these patients’ conditions perioperatively. The involvement of the care manager yielded a positive impact on patients’ health [13]. Patients with co-morbidities were referred to the endocrinologist, cardiologist, anaesthesiologist and psychiatrist as required.
Operation technique
Pneumoperitoneum was first created using a 15 mm optical port and a zero degree laparoscope. The laparoscopic procedure is performed with a total of 5 ports. At the epigastric port, a Nathanson retractor is used for liver retraction. Subsequently, the pars flaccid technique is used to create a tunnel behind the upper stomach. Initially, a 46 Fr calibration tube was used to measure a small pouch of stomach above the band. After the initial learning curve, our surgeons were able to estimate the pouch size without calibration. The band was secured with at least 3 non-absorbable anterior gastro-gastric sutures.
Patients had a Gastrografin (Bracco,NJ) contrast study to confirm the adequacy of band placement with no contrast extravasation the following day and was then started on a liquid diet for 2 weeks.
Statistical methods
Statistical analysis was performed using SPSS (version 20.0; SPSS Inc, Chicago, IL). Continuous variables were analysed using independent-samples-t-tests. For multivariate analysis, logistic regression was used to determine confounding factors on weight loss. The criteria for statistical significance was p <0.05.
Results
Between June 2001 and July 2011, 360 patients underwent LAGB at two institutions in Singapore. Based on the preoperative BMI, patients were divided into two groups: (1) Group A consisting of patients in WHO Obesity Obesity Class I (BMI 30-34.9 kg/m2) and II (BMI 35-39.9 kg/m2) and (2) Group B consisting of patients in WHO Obesity Class III (BMI ≥ 40 kg/m2) [14]. BMI of 40 kg/m2 was chosen as the cut-off as it is the lower limit of morbid obesity. Percentage weight loss (%WL) and percentage excess weight loss (%EWL) were calculated using standard methods for both groups. The baseline demographics of both groups are mentioned in (Table 1). Mean operating duration was 98 min (range: 35-420 mins). Mean postoperation stay in hospital was 1.3 days (range: 1-10 days).
| Group A (BMI <40 kg/2) | Group B (BMI ≥40 kg/2) | p-value | |
|---|---|---|---|
| Number of patients (n) | 157 | 203 | NA |
| Mean Age (years) | 36.8 | 34.3 | 0.109 |
| Gender (n, %) | |||
| Male | 44 (28.0%) | 95 (46.8%) | 0.19 |
| Female | 113 (72.0%) | 108 (53.2%) | |
| Race (n, %) | |||
| Chinese | 75 (47.8%) | 87 (42.9%) | |
| Malay | 33 (21.0%) | 63 (31.0%) | 0.2 |
| Indian | 37 (23.6%) | 41 (20.2%) | |
| Others | 12 (7.6%) | 12 (1.9%) | |
| Mean Preoperative weight (kg) | 98.4 | 128.6 | NA |
| Mean Preoperative BMI (kg/2) | 36.1 | 46.2 | NA |
| Mean Excess Weight (kg) | 36.5 | 64.6 | NA |
| Mean Operative Time (min) | 99.6 | 96.7 | 0.607 |
| Mean Hospital Stay (days) | 1.3 | 1.3 | 0.759 |
| Band-related complications | 24 | 27 | NA |
| Non-band related complications | 21 | 45 | NA |
Table 1: Baseline demographics and post-operative complications of Group A (BMI <40 kg/m2) and Group B (BMI ≥ 40 kg/2).
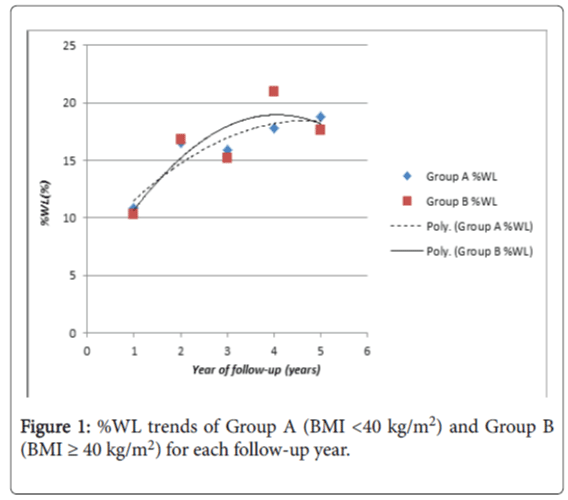
Post-operative outcomes of Groups A and B are shown in (Table 2). There was a significant difference in %EWL between the two groups at one year follow-up (p value=0.01), demonstrating that patients in Group A experienced significantly greater %EWL compared to patients in Group B. Otherwise, there was no other statistical significance between the two groups in %EWL for subsequent followup years and in %WL across all 5 years. Additionally, %WL of both groups was trended in (Figure 1), which demonstrated a common trend of %WL peaking at 3 to 4 year follow-up and tapering off afterwards.
| Follow-up | Number of patients on follow up (%) | %WL (%) | %EWL (%) | |||||
|---|---|---|---|---|---|---|---|---|
| Group A | Group B | Group A | Group B | p-value | Group A | Group B | p-value | |
| 1 year follow-up | 103 (65.5%) | 130 (64.0%) | 10.8 | 10.3 | 0.49 | 30 | 20.8 | 0.01 |
| 2 year follow-up | 57 (36.3%) | 81 (39.9%) | 16.5 | 16.8 | 0.58 | 47.6 | 33.9 | 0.37 |
| 3 year follow-up | 54 (34.4%) | 57 (28.1%) | 16.2 | 15.2 | 0.73 | 43.1 | 32.4 | 0.07 |
| 4 year follow-up | 33 (21.0%) | 44 (21.7%) | 17.8 | 21 | 0.54 | 56.3 | 43.7 | 0.17 |
| 5 year follow-up | 32 (20.4%) | 46 (22.7%) | 18.8 | 18.7 | 0.5 | 52.6 | 34.9 | 0.07 |
Table 2: %WL and %EWL of Group A (BMI <40 kg/m2) and Group B (BMI ≥ 40 kg/m2) for each follow-up year.
Multivariate analysis was performed on relevant baseline demographics and there were no significant independent factors found to affect the %EWL between the 2 groups (p value>0.1)
Complications
A total of 90 patients (25%) developed complications during the study, for which the details are shown in (Table 3). Most of the complications were minor band and port-related issues. It also included seven mortalities on follow-up, out of which two were bandrelated. The remaining mortalities were unrelated to the insertion of the band. During the laparoscopic surgery, seven of the surgeries had to be converted into open surgery due to bleeding that obscured the surgeon’s vision.
| Complications | Number of cases | Percentage (%) |
|---|---|---|
| Band-related | ||
| Slippage | 22 | 6.1 |
| Erosion | 19 | 5.3 |
| Leakage | 8 | 2.2 |
| Tubing malfunction | 19 | 5.3 |
| Port malfunction | 9 | 2.5 |
| Esophageal dilation | 30 | 8.3 |
| Infection | 11 | 3.1 |
Table 3: Complications of LAGB in Group A (BMI <40 kg/m2) and Group B (BMI ≥ 40 kg/m2) for each follow-up year.
As a result of complications, 23 patients (6.39%) underwent either band or port replacement, while 56 patients (15.6%) had to have removal of the gastric band. Six other patients requested for band removal without facing any complications. During the follow-up period, three patients converted to gastric bypass surgery while eight converted to sleeve gastrectomy. It must be noted that each patient may encounter more than one complication during the study.
There were two band-related deaths in this cohort. One patient had severe aspiration after surgery and despite maximal care in the intensive care unit, the patient passed away after two days. The other mortality was after the patient developed early band erosion within a few days of the insertion of the band. The patient developed septic shock due to a leak and multiple upper abdominal abscesses. The patient was resuscitated and the abscesses drained but the patient passed away despite maximal medical management.
Discussion
In this descriptive study of 360 patients who underwent LAGB surgery in Singapore, the median %EWL was 52.6% in Group A and 34.9% in Group B at five years follow up. These findings mirror the results of Alhamdani, et al. [15] where the median %EWL was 40% at ≥ five years post operation in cohort of 575 patients. In addition, regardless of preoperative BMI, we noted a common trend in both groups that %WL was the highest at 3 to 4 year post-LAGB. However, O'Brien, et al. explored the benefits of LAGB over a longer period [16] and demonstrated 47.1% EWL at 15 years, suggesting that weight loss from LAGB surgery may be maintained in the long term.
We reported a statistically significant difference between %EWL of Group A (30.0%) and Group B (20.8%) at one year follow-up (p=0.01) as well. It is also worth noting that during the three and five year follow-up, the results approached clinical significance (p=0.07). Consistent with these observations was a study by Xing, et al. [17] which reported that patients with lower BMI (<35 kg/m2) experienced a greater mean %EWL (50%) compared to patients with higher BMI (≥ 35 kg/m2) (%EWL 25%) within a 5 year follow-up period. As such, our study highlighted that LAGB benefits patients of lower BMI more than patients of higher BMI.
In our study, a total of 90 patients (25%) developed complications post-operatively. This supports existing data that LAGB is associated with a high complication rate. Various studies revealed that 20-50% of study population post-LAGB eventually experienced complications [18-20]. The most common complications encountered within our study were band-related (14.2%), which was similar to the study by Wang, et al. where 24.6% of patients developed band-associated complications [21]. These are often late complications that warrant surgical intervention. The rate of major complication, defined in this study by Suter, et al. as requiring band-removal, increases 3-4% each year, resulting in higher total failure rates and increased need for revision surgery. This may contribute to poor long-term outcomes of LAGB even though it is a minimally invasive procedure [22].
Comparisons have been made to other modes of bariatric surgery such as Roux-en-Y gastric bypass (RYGB) and sleeve gastrectomy (SG). One study suggests that these three bariatric surgeries provide similar weight-loss and safety profiles over 18 months but better remission of diabetes, hypertension and dyslipidemia was obtained with RYGB [23]. However, other studies at 2 years follow-up show that LAGB demonstrated poorer weight loss compared to RYGB and SG [24,25]. Moreover, LAGB has significantly higher complication rate than RYGB [26] and thereby, potentially making it a less popular choice amongst surgeons and patients nowadays. Our study echoed similar findings that LAGB is effective in achieving weight loss in the short term, but has a high rate of complications resulting in band removal subsequently.
To assess for the complications of the band, upper gastrointestinal tract imaging such as dilute barium swallow is performed to diagnose a pouch dilatation or band slippage [27]. A gastroscopy is necessary to pick up band erosion, another commonly seen complication.
In our study, 66 patients (18.3%) underwent band removal either due to band-related complications or personal preference without any complications. Where possible, in lieu of band removal, band revision with insertion of a new band can be considered. One study on outcomes of revision LAGB shows that revision LAGB is reasonably well-tolerated by most patients [28]. Out of 183 consecutive revision LAGB procedures performed in 163 patients, patients experienced 51.52% EWL and overall complication rate of 13.7%. Hence, instead of band removal, band revision can be a viable option for patients with band-related complications.
Where band removal is inevitable, patients in our study underwent the excision of band, followed by band replacement or conversion to sleeve gastrectomy. The outcomes of revision LAGB have been explored in a study showing that patients were able to maintain weight loss achieved from the primary banding, even after the revision surgery [28]. In another study, revision LAGB was well-tolerated as evident in low mortality rate of 0.8% and morbidity rate of 4.6% [29]. The same study applied a structured reoperation algorithm to maximise the efficacy of LAGB in the long term, which is one possible solution to tackle band-related complications.
We acknowledge that our study has several limitations. Firstly, it is a retrospective study and not a prospective trial designed to compare the differences in outcomes of LAGB between BMI<40 kg/m2 and ≥ 40kg/m2. This may introduce unknown biases to this study which may result in spurious conclusions. Hence the results should be applied in the appropriate clinical context Secondly, although our data was collected over 10 years, the follow-up rate beyond 5 years post-LAGB was marginal. Hence, there is insufficient data at 10-years follow up to be included in this study to make any conclusions with regard to the outcomes in LAGB in a longer term. Future studies can explore other metabolic parameters between Group A and B and compare the performances of different bariatric surgeries in a Singaporean population.
Conclusion
In conclusion, LAGB is an effective bariatric surgical option for weight loss in obese Singaporean patients over a short-term but it is more beneficial in patients with lower BMI (Group A with BMI<40 kg/m2) with in the first year.
References
- Singapore (2010) Ministry of Health. Epidemiology and Disease Control Division., National health survey 2010, Singapore. National health survey Singapore.
- Singapore (2004) Ministry of Health. Epidemiology and Disease Control Division., National health survey 2004, Singapore. National health survey Singapore 7: 128.
- Wang J, Thornton CT, Russell M, Burastero S, Heymsfield S, et al. (1994) Asians have lower body mass index (BMI) but higher percent body fat than do whites: comparisons of anthropometric measurements. The American Journal of Clinical Nutrition 7: 23-28.
- Pi-Sunyer X (2002) The Medical Risks of Obesity. Obesity Surgery12 : S6-S11.
- The Straits Times (2012) More opt for drastic weight-loss surgery.
- O'Brien PE, McPhail T, Chaston TB, Dixon JB, (2006) Systematic review of medium-term weight loss after bariatric operations. Obes Surg 16: p1032-1040.
- Dixon JB, O'Brien PE, Playfair J, Chapman L, Schachter LM, et al. (2006) Adjustable gastric banding and conventional therapy for type 2 diabetes: a randomized controlled trial. JAMA 299: 316-23
- Courcoulas AP, Christian NJ, Belle SH, Berk PD, Flum DR, et al. (2013) Weight change and health outcomes at 3 years after bariatric surgery among individuals with severe obesity. JAMA 310: 2416-2425.
- Dolan K, Bryant R, Fielding G (2003) Treating diabetes in the morbidly obese by laparoscopic gastric banding. Obes Surg 13: 439-443.
- Ngiam KY, Lee WJ, Lee YC, Cheng A (2014) Efficacy of metabolic surgery on HbA1c decrease in type 2 diabetes mellitus patients with BMI <35 kg/m2--a review. Obes Surg 24: p148-158.
- Schauer PR, Kashyap RS, Wolski K, Brethauer AS, Kirwan PJ, et al. (2012) Bariatric surgery versus intensive medical therapy in obese patients with diabetes. N Engl J Med 366: p1567-1576.
- Ganesh R, Leese T, Rao AD, Baladas HG (2006) Laparoscopic adjustable gastric banding for severe obesity. Singapore Med J 47: p661-669.
- Ciccone MM, Aquilino A, Cortese F, Scicchitano P, Sassara M, et al. (2010) Feasibility and effectiveness of a disease and care management model in the primary health care system for patients with heart failure and diabetes (Project Leonardo). Vasc Health Risk Manag 6: p297-305.
- Obesity (2000) preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser 894: 1-253.
- Alhamdani A, Wilson M, Jones T, Taqvi L, Gonsalves P, et al. (2012) Laparoscopic adjustable gastric banding: a 10-year single-centre experience of 575 cases with weight loss following surgery. Obes Surg 22: 1029-1038.
- O'Brien PE, MacDonald L, Anderson M, Brennan L, Brown WA, (2013) Long-term outcomes after bariatric surgery: fifteen-year follow-up of adjustable gastric banding and a systematic review of the bariatric surgical literature. Ann Surg 257: 87-94.
- Liu, X.Z, Yin K, Fan J, Shen XJ, Xu MJ, et al. (2015) Long-Term outcomes and experience of laparoscopic adjustable gastric banding: one center's results in China. Surg ObesRelat Dis 11: 855-859.
- Owers, C, Ackroyd R (2013) A study examining the complications associated with gastric banding. Obes Surg 23: 56-59.
- Michalik M, Lech P, Bobowicz M, Orlowski M, Lehmann A, et al. (2011) A 5-year experience with laparoscopic adjustable gastric banding--focus on outcomes, complications, and their management. Obes Surg 21: 1682-1686.
- Lanthaler M, Aigner F, Kinzl J, Sieb M, Cakar-Beck F, et al. (2010) Long-term results and complications following adjustable gastric banding. Obes Surg 20: 1078-1085.
- Wang X, Zheng ZC, Chang SX, Zhao X, Yin K, et al. (2013) Laparoscopic adjustable gastric banding: a report of 228 cases. Gastroenterol Rep (Oxf) 1: 144-148.
- Suter, M, Calmes JM, Paroz A, Giusti V, (2006) A 10-year experience with laparoscopic gastric banding for morbid obesity: high long-term complication and failure rates. Obes Surg 16: 829-835.
- Lee SK, Heo Y, Park JM, Kim YJ, Kim SM, et al. (2016) Roux-en-Y Gastric Bypass vs. Sleeve Gastrectomy vs. Gastric Banding: The First Multicenter Retrospective Comparative Cohort Study in Obese Korean Patients. Yonsei Med J 57: 956-962.
- Weber M, Müller KM, Bucher T, Wildi S, Dindo D, et al. (2004) Laparoscopic gastric bypass is superior to laparoscopic gastric banding for treatment of morbid obesity. Ann Surg 240: 975-982
- Gill, R.S, Majumdar SR, Clausen CFR, Apte S, Birch DW, et al. (2016) Comparative effectiveness and safety of gastric bypass, sleeve gastrectomy and adjustable gastric banding in a population-based bariatric program: prospective cohort study. Can J Surg 59: 13315.
- Zuegel NP, Lang AR, Hüttl PT, Marc Gleis, Jungen KM, et al. (2012) Complications and outcome after laparoscopic bariatric surgery: LAGB versus LRYGB. Langenbecks Arch Surg 397: 1235-1241.
- Moey, T, Peh WC, Clarke MJ, Dubey N, Cheng A (2009) Radiological features of complications of laparoscopic adjustable gastric banding. Radiol Med 114: 802-810.
- Ee E, Nottle PD (2013) Outcomes of revision laparoscopic gastric banding: a retrospective study. ANZ J Surg 83: 571-574.
- Biertho L, Steffen R, Branson R, Potoczna N, Ricklin T, et al. (2005) Management of failed adjustable gastric banding. Surgery 137: 33-41.
Relevant Topics
- Android Obesity
- Anti Obesity Medication
- Bariatric Surgery
- Best Ways to Lose Weight
- Body Mass Index (BMI)
- Child Obesity Statistics
- Comorbidities of Obesity
- Diabetes and Obesity
- Diabetic Diet
- Diet
- Etiology of Obesity
- Exogenous Obesity
- Fat Burning Foods
- Gastric By-pass Surgery
- Genetics of Obesity
- Global Obesity Statistics
- Gynoid Obesity
- Junk Food and Childhood Obesity
- Obesity
- Obesity and Cancer
- Obesity and Nutrition
- Obesity and Sleep Apnea
- Obesity Complications
- Obesity in Pregnancy
- Obesity in United States
- Visceral Obesity
- Weight Loss
- Weight Loss Clinics
- Weight Loss Supplements
- Weight Management Programs
Recommended Journals
Article Tools
Article Usage
- Total views: 12054
- [From(publication date):
August-2016 - Jul 15, 2025] - Breakdown by view type
- HTML page views : 11111
- PDF downloads : 943