Research Article Open Access
Labor Induction in Primiparous Women and Women with an Unripe Cervix-1
Anna Thorbiornson1, Tomislav Vladic2 and Ylva Vladic Stjernholm2*
1Educational Programme in Gynaecology and Obstetrics, Karolinska Institute and Karolinska University Hospital, Stockholm, Sweden
2Department of Women’s and Children’s Health, Karolinska Institute and Karolinska University Hospital, Stockholm, Sweden
- *Corresponding Author:
- Ylva Vladic Stjernholm
Department of Women’s and Children’s Health
Karolinska University Hospital Solna, Stockholm, Sweden
Tel: 46851770999
E-mail: ylva.vladic-stjernholm@karolinska.se
Received date: May 30, 2016; Accepted date: June 07, 2016; Published date: June 11, 2016
Citation: Thorbiornson A, Vladic T, Stjernholm YV (2016) Labor Induction in Primiparous Women and Women with an Unripe Cervix. J Preg Child Health 3:259. doi:10.4172/2376-127X.1000259
Copyright: © 2016 Thorbiornson A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Pregnancy and Child Health
Abstract
Objective: To compare the efficacy and safety of oral prostaglandin in solution, vaginal prostaglandin gel and trans cervical catheter for labor induction in primiparous women and women with an unripe cervix. Design: A retrospective study. Methods: Data from original obstetric records at a university hospital in Sweden in 2012-2013. Results: In primiparous women, vaginal birth <24 h was achieved in 54% with oral prostaglandin, 71% with vaginal prostaglandin, and 71% with catheter, whereas caesarean section was needed in 25%, 41% and 26% respectively. In women with an unripe cervix, vaginal birth <24 h was achieved in 66% with oral prostaglandin, 79% with vaginal prostaglandin, and 77% with catheter, while caesarean section was carried out in 21%, 33% and 21% respectively. The induction to vaginal delivery interval was the shortest with catheter and the longest with oral prostaglandin. The rates of obstetric bleeding, chorioamnionitis, uterine hyper stimulation and neonatal asphyxia were comparable. Conclusion: Oral prostaglandin in solution was less effective than vaginal prostaglandin gel and transcervical catheter in achieving vaginal birth <24 h. However, oral prostaglandin and catheter were safer, since they resulted in fewer caesarean sections without increasing maternal morbidity or neonatal asphyxia.
Keywords
Catheter; Caesarean section; Prostaglandin; Dinoprostone; Misoprostol; Vaginal birth
Introduction
Labor is induced in 20-30% of all pregnancies. It has increased in Sweden from 7% in the early 1990s to 16% in 2012–2013 [1-3]. Induced labor involves increased risks for prolonged delivery and cesarean section (CS). These risks are high in primiparous women and women with an unripe cervix. Among these women, pre-induction cervical ripening is important for a successful vaginal birth (VB). To our knowledge, there are very few reports on labor induction with oral prostaglandin (OPG) in solution, vaginal prostaglandin (VPG) gel and transcervical catheter in primiparous women and women with an unripe cervix. The meta-analyses reviewers do not report such analyses [4-6].
Approximately two out of three CS are carried out in women with a previous CS. The rising CS rates are followed by increasing reports on maternal mortality and morbidity such as life-threatening obstetric bleeding, placenta complications and peripartal hysterectomy, as well as neonatal and infant complications, e.g. breathing disturbances, altered gut microbiota and DNA-methylation in white blood cells [7-9]. An uncomplicated first delivery is the primary positive prognostic factor for a later uncomplicated delivery. Thus, if a woman achieves an uncomplicated first delivery, she can probably avoid undergoing a CS later in life [7].
Labor induction with transcervical catheter was described in the 1860s [10]. The catheter separates the fetal membranes from the uterine wall, which leads to prostaglandin and oxytocin release from the fetal membranes and uterine decidua [11]. The catheter may also stimulate neuroendocrine pathways interrelated with oxytocin synthesis and release, i.e., the Ferguson reflex [12].
VPG treatment was used for labor induction since the 1980s. OPG treatment was avoided until the 1990s, because of presumed less efficacy due to first pass liver metabolism and gastrointestinal side effects [1,5,6]. PGs are the key mediators for cervical ripening and act via membrane bound G-coupled receptors. They promote cervical ripening via leukocyte chemotaxis and extravasation and a changed progesterone receptor A to B expression resulting in progesterone withdrawal. These events result in an increased collagenase enzyme activity, a changed proteoglycan composition and dispersed collagen fibrils, allowing for cervical effacement and dilatation [3,11,13].
The aim of this study was to compare the efficacy and safety of OPG in solution, VPG gel and transcervical catheter for labor induction in primiparous women and women with an unripe cervix. Our hypothesis was that OPG in solution would be safer than and at least as effective as VPG gel and catheter.
Methods
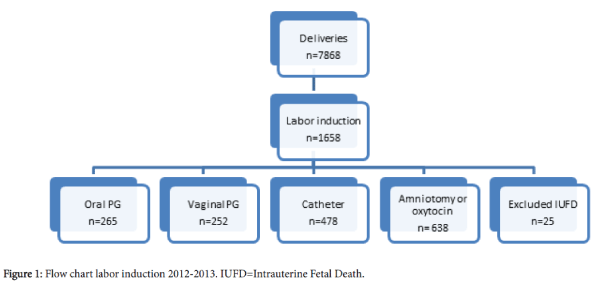
The study was approved by the Ethics Board for Medical Sciences in Stockholm, Sweden, on April 9th 2015, Dnr 2014/255-31. The World Health Organization (WHO) International Classification of Diseases (ICD)-10 and the obstetric records for all women who had labor induced with OPG, VPG or catheter at the Department of Women’s and Children’s Health, Karolinska University Hospital, Solna, Sweden in 2012-2013 were investigated. Inclusion criterion was gestational age ≥ 34+0 weeks. Between January 1st 2012 and December 31st 2013, there were 7868 deliveries in the unit. Labor was induced in 1658 women (21%). Prostaglandins were used for labor induction in 542 women (33%) and catheter in 478 women (29%). Part of this material is described in related studies [14,15]. The remaining 638 women, all with a ripe cervix Bishop score >5, had labor induced with amniotomy or oxytocin infusion. Women suffering from intrauterine fetal death (n=25) were excluded from the calculations (Figure 1).
VPG was the only available PG method in 2012. A total of 252 women had labor induced with this method, 207 in 2012 and 45 in 2013, due to the individual phycisian´s choice. Endogenous PGE gel dinoprostone (Minprostin®, Pfizer, SE-19138 Sollentuna, Sweden) 2 mg was inserted in the posterior vaginal fornix every 6-8 h up to a maximum of 3 doses. According to the manufacturer, the endogenous PGE2 dinoprostone preparation is followed by a peak plasma concentration after 30-45 min after vaginal administration. The fetal heart activity was monitored with cardiotocography (CTG) 20 min before each dose and at labor onset. OPG in sol of 8 doses ution was introduced for labor induction in 2013, and 265 women had labor with this method. The smallest available synthetic, esterified PGE analogue misoprostol tablet (Cytotec®, Pfizer, SE-19138 Sollentuna, Sweden) 200 μg was dissolved in 20 mL of water resulting in a concentration of 10 μg/mL. An adequate concentration was obtained [16]. A solution of 2.5 mL containing 25 μg misoprostol was aspirated in a 3 mL syringe, whereupon the woman sprayed the solution in her mouth. Then, water was aspirated and swallowed. Treatment with a fresh solution 25 μg was continued every 2 h until labor onset up to a maximum of 8 doses. The synthetic, esterified PGE1 analogue misoprostol is followed by a peak plasma concentration after 30 min after oral administration, decreasing significantly within 120 min [17]. The fetal heart activity was monitored with CTG 20 min before each dose and at labor onset. If uterine contractions were monitored, the following dose was postponed for 2 h, given that active labor had not started. Amniotomy was performed when a ripe cervix with a Bishop score (BS) >5 points was achieved. Alternatively, a transcervical catheter was inserted and amniotomy performed after expulsion of the catheter. Oxytocin (Syntocinon®, CD Pharma, SE-751 83 Uppsala, Sweden) infusion 5 U/500 mL NaCl 0.9% was administered for augmentation of labor, if no progress within 1 our following ruptured fetal membranes.
Mechanical induction was carried out with a 22 Charrière Foley catheter (Meteko Instruments AB, Stockholm, Sweden), which was inserted into the extra amniotic space at speculum investigation or digital examination according to the preference of the physician. A total of 478 women had labor induced with catheter, 314 in 2012 and 164 in 2014. After insertion, the catheter balloon was filled with water or NaCl 0.9% 50 mL and fastened to the thigh without traction. The position of the catheter was controlled by traction every 30 min. Amniotomy was performed immediately after expulsion of the catheter. According to the clinical guidelines, the catheter was removed if not expelled after 8 h and amniotomy was performed. Oxytocin infusion 5 U/500 mL saline was started within one hour after amniotomy if no uterine contractions were observed, and immediately after catheter expulsion in women with pre-labor rupture of the membranes. The fetal heart activity was monitored with CTG 20 min before and after application and at labor onset.
Post-term pregnancy was gestation ≥ 42+0 weeks. Pre-labor rupture of the fetal membranes was diagnosed visually and labor was induced after 36-48 h. The hypertensive disease group was women with essential hypertension, gestational hypertension and preeclampsia. The group imminent fetal distress included reduced fetal movements with oligohydramniosis, intrauterine growth restriction, decidual bleeding or Rhesus immunization. Psychosocial indications were fear of childbirth and pregnancy ailments. Maternal illness included thrombophilia, malignancy, heart disease and other systemic diseases. Other fetal indications were, e.g. labour induction after external version of breech presentation, fetal anomalies and cardiac arrhythmia. Women with gestational diabetes or diabetes mellitus had labor induced at 38-40 weeks. Primiparous women ≥ 40 years after in vitro fertilization (IVF) had labor induced at 41 weeks. A prolonged latency phase was cervical dilatation ≤ 3 cm after uterine contractions for 18 hours or more. Dichoriotic twin pregnancies with symmetric fetal growth were induced at 38 weeks and monochoriotic with the same criteria at 37 weeks. Cervical ripeness was categorized according to a simplified BS model, where a BS ≤ 5 was the criterion for an unripe cervix [18]. Hyper stimulation was defined as >5 contractions every 10 min during 20 min as monitored by CTG. An Apgar score <7 at 5 min was the criterion for neonatal asphyxia since Apgar scores, but not umbilical blood gas values, were registered for all new-borns [19].
The primary outcomes were VB<24 h and the CS rate. Secondary outcomes were the induction to vaginal delivery interval, the proportions of obstetric bleeding, chorioamnionitis, uterine hyperstimulation, uterine rupture and neonatal asphyxia.
Continous data were analysed with one-way analysis of variance (ANOVA). Assumptions for parametric statistics were tested by Levene’s test. Categorical data were analysed with non-parametric Mann-Whitney test. Statistical significance was set at p<0.05. We assumed that 40% with OPG and 60% with VPG and catheter would achieve VB<24 h. Aiming at a significance level of 5% and 90% power, 125 observations would be needed in each group. We assumed that the CS rate would be 20% with OPG and 30% with VPG and catheter. Aiming at a significance level of 5% and 90% power, 194 observations would be needed in each group [4-6,19]. All data were entered into the computer program Statistica, version AX, Stat Soft, Inc., Tulsa, Oklahoma, US (2014).
Results
The indications for induced labor are shown in Table 1.
| Variable | OPG n=265 (%) |
VPG n=252 (%) |
Cathetern n=478 (%) |
|---|---|---|---|
| Post-term pregnancy | 64 (24) | 57 (23) | 97 (20) |
| Pre-labor rupture of fetal membranes | 41 (15) | 35 (14) | 110 (23) |
| Hypertensive disease | 36 (14) | 31 (12) | 54 (11) |
| Imminent fetal distress | 36 (14) | 31 (12) | 61 (13) |
| Psychosocial indication | 24 (9) | 20 (8) | 52 (11) |
| Maternal illness | 22 (8) | 26 (10) | 33 (17) |
| Other fetal indications | 17 (6) | 16 (6) | 14 (3) |
| Diabetes | 10 (4) | 12 (5) | 18 (4) |
| Primiparous women ≥ 40 years after IVF | 7 (3) | 14 (6) | 16 (3) |
| Latency phase prolonged | 6 (2) | 5 (2) | 17 (4) |
| Duplex pregnancy | 2 (1) | 5 (2) | 6 (1) |
Table 1: Indications for labour induction. Differences all variables (NS).
The indications and the criteria for prolonged labor were unchanged. Prolonged labor was lack of progress for 3-4 h during the first stage of labor and for 2-3 h during the second stage. Demographic data are shown in Table 2.
| Variable | OPG n=265 |
VPG n=252 |
Catheter n=479 (%) |
|---|---|---|---|
| Age (median and range) | 32 (18-46) | 32 (18-47) | 32 (17-50) |
| Primiparous (%) | 164 (63.6) | 157 (62.8) | 245 (51.2) |
| Previous cesarean section (%) | 8 (3.1) | 25 (10.0) | 64 (13.4) |
| Gestational age (median and range) | 39 (34-42) | 39 (34-42) | 40 (34-42) |
| Gestational age<37+0 weeks (%) | 13 (4.9) | 9 (3.6) | 9 (1.9) |
Table 2: Demographic data. Differences all variables (NS).
The groups with an unripe cervix BS ≤ 5 included similar proportions of primiparous women: in the OPG group 146 (61%) women were primiparous, 85 (36%) parous and 7 (3%) had a previous CS. In the VPG group, 151 (62%) women were primiparous, 68 (28%) parous and 25 (10%) had a previous CS. In the catheter group 201 (50%) women were primiparous, 146 (46%) parous and 55 (14%) had a previous CS. Maternal and neonatal outcomes are shown in Table 3.
| Variable | OPG | VPG | Catheter | OPG vs. VPG | OPG vs. Catheter |
|---|---|---|---|---|---|
| All women | n=265 (%) | n=252 (%) | n=478 (%) | p value | p value |
| Vaginal birth | 214 (80.8) | 171 (67.9) | 382 (79.9) | NS | NS |
| Vaginal birth <24 h | 141 (65.9) | 136 (79.5) | 373 (78.0) | p<0.001 | p<0.001 |
| Instrumental delivery | 48 (18.1) | 30 (11.9) | 69 (14.4) | p=0.02 | NS |
| Cesarean section | 51 (19.2) | 81 (32.1) | 96 (20.1) | p=0.02 | NS |
| Obstetric bleeding >1000 mL | 19(7.1) | 20 (7.9) | 28 (5.9) | NS | NS |
| Chorioamnionitis | 8 (3.0) | 4 (1.6) | 9 (1.9) | NS | NS |
| Primiparous women | n=164 (%) | n=157 (%) | n=245 | ||
| Vaginal birth | 123 (75.0) | 92 (58.6) | 181 (73.9) | NS | NS |
| Vaginal birth <24 h | 66 (53.7) | 65 (70.7) | 175 (71.4) | p=0.01 | p<0.001 |
| Instrumental delivery | 43 (26.2) | 24 (15.2) | 45 (18.4) | p=0.03 | NS |
| Cesarean section | 41 (25.0) | 65 (41.4) | 64 (26.1) | p=0.03 | NS |
| Bishop score ≤ 5 | n=238 (%) | n=244 (%) | n=402 (%) | ||
| Vaginal birth | 189 (79.4) | 164 (67.2) | 319 (79.3) | NS | NS |
| Vaginal birth <24 h | 125 (66.1) | 129 (78.7) | 311 (77.3) | p=0.01 | p<0.001 |
| Instrumental delivery | 44 (18.5) | 30 (12.3) | 56 (13.9) | p=0.04 | NS |
| Cesarean section | 49 (20.6) | 80 (32.8) | 83 (20.6) | p=0.04 | NS |
| Neonatal outcomes | n=265 | n=252 | n=478 | ||
| Birth weight (g) (mean ± SD) | 3472 ± 579 | 3521 ± 602 | 3514 ± 560 | NS | NS |
| Apgar score <7 at 5 min (%) | 4 (1.5) | 1 (0.3) | 9(1.9) | NS | NS |
Table 3: Maternal and neonatal outcomes. OPG=Oral Prostaglandin, VPG=Vaginal Prostaglandin.
Most CS, more than 60% with all treatments, were carried out because of a prolonged first stage of labor. The second indication was imminent fetal distress defined as a pathologic CTG or fetal scalp lactate >4.8 mmol/L. The main indication for an instrumental delivery with all treatments was a prolonged second stage of labor. No uterine ruptures were observed. There was no episode of uterine hyper stimulation with OPG or catheter, whereas one CS in the VPG group was carried out because of uterine hyper stimulation resulting in fetal bradycardia within 1 h after the first VPG dose. The induction to vaginal delivery intervals are shown in Table 4. The induction to vaginal delivery interval was the shortest with catheter, 7-10 hours shorter compared to OPG and 5-7 h shorter compared to VPG.
| Variable | OPG | VPG | Catheter | OPG vs. VPG | OPG vs. Catheter |
|---|---|---|---|---|---|
| All women | 21.6 ± 0.6 | 18.2 ± 0.7 | 12.9 ± 0.3 | p<0.001 | p<0.001 |
| Primiparous | 24.9 ± 0.8 | 21.4 ± 0.9 | 14.4 ± 0.4 | p<0.01 | p<0.001 |
| Bishop score ≤ 5 | 22.7 ± 0.6 | 20.4 ± 0.6 | 13.1 ± 0.3 | p<0.01 | p<0.001 |
Table 4: Induction to vaginal delivery interval in hours (mean ± standard error).
The induction to vaginal delivery interval was 7-10 h shorter with catheter compared to OPG and VPG.
The primary findings were that VPG gel and catheter were more effective than OPG in solution in achieving VB<24 h. However, OPG and catheter were safer, since they resulted in fewer CS compared with VPG in all women, primiparous women and women with an unripe cervix. The overall CS rate in 2012-2013 was 22% and the CS rate after induced labor was 30%. Thus, OPG and catheter resulted in lower CS rates and VPG in higher, than was generally observed at induced labor. The rates of VB <24 h were higher than was assumed with all methods.
The higher instrumental delivery rate with OPG could be explained by the longer induction to vaginal delivery interval, since most instrumental deliveries were carried out because of a prolonged second stage of labor. The proportions of obstetric bleeding >1000 mL at vaginal delivery in the study groups were comparable to the overall incidence, being 6.7% in 2012-2013. The rates of chorioamnionitis in the study groups did not differ from the overall incidence, being 1.3%. The proportions of new-borns with an Apgar score <7 at 5 min were similar to the total incidence at a gestational age ≥ 34+0 weeks, which was 1.0%. In average, 5 doses of OPG and one dose of VPG respectively, were used. The cost for 5 fresh OPG doses was €9.2 which was less than 5% of the cost for one dose of VPG gel. The cost for one Foley catheter was €2.2.
The present findings differed from the PROBAAT-I study on labor induction with VPG gel vs . catheter, which report similar CS rates with the treatments, 20% vs . 23% [4]. The present findings also differed from the PROBAAT-II study onlabor induction with OPG capsules vs . catheter, which report similar CS rates with the treatments 17% vs. 20% [6]. However, our findings were in concordance with amulticenter randomized study comparing OPG in solution with VPG gel, which report a lower CS rate with OPG, 21% vs. 26% [19,20]. Our findings were also in agreement with a recent systematic review and network meta-analysis on labor induction with PGs. The authors conclude that OPG in solution is the safest PG method, and note that OPG in solution is not recommended by the WHO, whereas OPG tablets are, despite the worst overall ranking in their analysis [5].
Limitations in this study were the retrospective character and the lack of information about umbilical cord blood gas values [21]. Strengths were the high number of observations and that all data were collected from original medical records.
In conclusion, labor induction with OPG in solution was less effective than VPG gel and catheter in achieving VB<24 h. However, OPG and catheter were safer, since they resulted in fewer CS in all women, primiparous women and women with an unripe cervix. The induction to vaginal delivery interval was the shortest with catheter and the longest with OPG. Despite this, the incidence of obstetric bleeding, chorioamnionitis and neonatal asphyxia were comparable with the treatments.
References
- World Health Organization (2011) WHO Recommendations for induction of labour. Geneva: World Health Organization.
- The Swedish National Board of Health and Welfare (2014) Medical Birth Register. Pregnancies, deliveries and new-born babies 1973-2013.
- Sahlin L, Stjernholm YV, Roos N, Masironi B, Ordeberg GE (2008) Impaired leukocyte influx in cervix in post term women not responding to prostaglandin priming. ReprodBiolEndocrinol 6:36.
- Jozwiak M, Rengerink KO, Benthem M (2011) PROBAAT study group: Foley catheter versus vaginal prostaglandin E2 gel for induction of labour at term (PROBAAT trial): An open-label randomised controlled trial. Lancet 378: 2095-2103.
- Alfirevic Z, Keeney E, Dowswell T, Welton NJ, Dias S, et al. (2015) Labour induction with prostaglandins: A systematic review and network meta-analysis. BMJ 350: 217.
- Eikelder TM, Rengerink KO, Jozwiak M, Leeuw JD, Graaf ID, et al. (2016) Induction of labour at term with oral misoprostol versus a Foley catheter (PROBAAT-II): A multicentre randomized controlled non-inferiorty trial. The Lancet.
- Spong CY, Berghella V, Wenstrom KD, Mercer BM, Saade GR (2012) Preventing the first cesarean delivery: Summary of a Joint Eunice Kennedy Shriver National Institute of Child Health and Human Development, Society for Maternal-Fetal Medicine and American College of Obstetricians and Gynecologists Workshop. ObstetGynecol 120:1181-1193.
- Schlinzig T, Johansson S, Gunnar A, Ekström TJ, Norman M (2009) Epigenic modulation at birth-altered DNA methylation in white blood cells after caesarean section. ActaPaediatr 98:1096-1099.
- Eggesbo M, Mandal S, Mitvedt T (2015) Factors affecting infant gut microbiota and possible consequences for health. MicrobEcol Health Dis 26: 28062.
- Woodman WB (1863) Induction of labor at eight months and delivery of a living child in less than four hours by Dr Barne’s method. The Lancet 81: 10-11.
- Hertelendy F, Zakar T (2004) Prostaglandins, the myometrium and the cervix. Prostagl, Leukot Essen Fatty Acids 70: 207-222.
- Ferguson JK (1941) A study of the motility of the intact uterus at term. SurgGynecolObstet 73: 359-366.
- Stjernholm YV, Vladic T, Selvanessan B, Ordeberg GE, Sahlin L (2009) Prostaglandin treatment is associated with a withdrawal of progesterone and androgen at the receptor level in the uterine cervix. ReprodBiolEndocrinol 7:116.
- Thorbiornson A, Vladic T, Vladic Stjernholm Y (2015). Labor induction with transcervical catheter versus oral misoprostol in primiparous women and women with an unripe cervix. Open J ObstetGynecol 5: 819-826.
- Thorbiornson A, Vladic T, Vladic Stjernholm Y (2016) Oral versus vaginal prostaglandin for labor induction. J Maternal-Fetal and Neonatal Medicine.
- The Swedish Medical products Agency (2012) Laboratory report study on preparation of misoprostol (Cytotec) for labor induction. Läkemedelsverket, Uppsala, Sweden.
- Tang OS, Schweer H, Seyberth H (2002) Pharmacokinetics of different routes of administration of misoprostol. Hum Reprod 17: 332-336.
- Laughon SK, Zhang J, Troendle J, Sun L, Reddy UM (2011) Using a simplified Bishop score to predict vaginal delivery. ObstetGynecol 117: 805-811.
- Apgar V (1953). A proposal for a new method of evaluation of the new-born infant. AnesthAnalgCurr Res 32:260-267.
- AlשּׁĀrevic Z, Aשּׁ?aifel N, Weeks A (2014) Oral misoprostol for induction of labour. Cochrane Database of Systematic Reviews 6: 1338.
- American Academy of Pediatrics (2006) Committee on the fetus and new-born. ACOG Committee Opinion.ObstetGynecol 107: 1209-1212.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 13711
- [From(publication date):
June-2016 - Apr 04, 2025] - Breakdown by view type
- HTML page views : 12722
- PDF downloads : 989