Review Article Open Access
Knowledge, Attitude, Practice and Associated Factors of Voluntary Blood Donation among Undergraduate Students in Hargeisa University
Abdirahman Omer Ahmed*Department of Public health, Jimma University College of Public Health and Medical Sciences, Ethiopia
- *Corresponding Author:
- Abdirahman Omer Ahmed
Department of Public health, Jimma University College of Public Health and Medical Sciences
Bole Sub-City, Woreda 02, Addis Ababa, Ethiopia
Tel: +251939998254
E-mail: abdi_4u2@hotmail.com
Received date: August 06, 2017; Accepted date: August 16, 2017; Published date: August 18, 2017
Citation: Ahmad AO (2017) Knowledge, Attitude, Practice and Associated Factors of Voluntary Blood Donation among Undergraduate Students in Hargeisa University. J Community Med Health Educ 7:547. doi:10.4172/2161-0711.1000547
Copyright: © 2017 Ahmed AO. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community Medicine & Health Education
Abstract
Background: Availability of blood for transfusion is limited in Somaliland; as is the evidence relating to knowledge, attitude and practice on blood donation among youth Since youth represent both large share of the population and important group of potential donors, this study attempts to investigate what factors may be important to consider for promoting voluntary blood donation among them.
Objectives: To assess the Knowledge, Attitude, Practice (KAP) of Voluntary Blood Donation and associated factor among undergraduate students in Hargeisa University.
Methods: An institutional based cross-sectional study was conducted on 311 undergraduate regular students in the University of Hargeisa from March 1-12 2016. The study participants were selected using stratified random sampling. A pre-tested structured questionnaire was used to collect data. Variables with P-value<0.25 were selected as candidates for Multivariate regression and variables with P-value<0.05 were considered as statistically significantly associated.
Results: The proportion of students having adequate knowledge was 46.6% and significantly associated with being a medical student [AOR: 2.591, 95% CI: 1.518, 4.422]. The proportion of students having favorable attitude was 46.9% and significantly associated with being a student at the faculty of Applied Science [AOR: 2.8, 95% CI: 1.136, 6.956], Health Science [AOR: 3.8, 95% CI: 1.205, 12.554] and Social Science [AOR: 10.00, 95% CI: 1.786, 55.976]. The proportion of students who have ever donated blood was 11.3% and significantly associated with age [AOR: 1.284, 95% CI: 1.078, 1.530] and being a male [AOR: 7.465, 95% CI: 2.104, 26.487].
Conclusion and Recommendation: More than half of the students had inadequate knowledge and unfavorable attitude towards blood donation; and majority of them had never donated blood. University Administrators in collaboration with Ministry of Health and Hargeisa Group Hospital’s Blood Bank Department must come up with plans to increase KAP of blood donation among university students.
Keywords
Knowledge; Attitude; Voluntary blood donation; Undergraduate students; University of Hargeisa
Abbreviations
AOR: Adjusted Odds Ratio; CI: Confidence Interval; COR: Crude Odds Ratio; HIV: Human Immunodeficiency Virus; KAP: Knowledge Attitude and Practice; OR: Odds Ratio; SPSS: Statistical Package for Social Science; UOH: University of Hargeisa; WHO: World Health Organization
Introduction
Blood is unique body fluid that performs vital functions for humans by carrying oxygen and nutrients to the cells and carrying out carbondioxide and metabolic wastes away from those same cells. Ancients Egyptians used to use blood for different purposes including when practicing healing rituals. In the early 20th century, Dr. Karl Landsteiner made a scientific break-through by discovering the ABO blood group system that was crucial in blood donation. The first blood bank storage unit was made in 1973 in Chicago. As the First World War ended, transfusion of blood was accepted as the treatment of choice for dealing with severe blood loss. Blood safety is important in enhancing health care and in preventing the spread of infectious disease. Each year blood transfusion helps save many lives, yet three issues remain a major constraint in the developing world: quality, quantity and safety of blood [1].
Blood transfusion is a vital component of health care. It helps saves millions of lives yearly through routine and emergency situations, aids in complex medical and surgical conditions and in improving the quality of life of the patients with different acute and chronic illnesses. In all health facilities, the accessibility of safe blood on time is very important; however, in many developing countries this constitutes a problem and the gap between blood demand and supply is widening. The capacity of health care system and its coverage of the population determine the national blood requirement of a country. In advanced health care system, such as those found in developed countries, the demand for blood continues to rise to sustain increasingly sophisticated medical procedures [2].
Voluntary unpaid blood donors whose blood has been checked for infection are the best source of safe blood. A resolution adopted by the World Health Assembly in 2010 highlighted that “secure supply of safe blood components, based on voluntary, non-remunerated blood donation must be an important national goal of every country to prevent blood shortages”. Blood supply in many middle and low income countries are in an alarming stage, especially in Sub-Saharan Africa which has the highest maternal mortality rate of 510 deaths per 100,000 live births [2].
A survey conducted by WHO in 2014 on blood safety and availability showed that out of 54 African countries, 40 countries (including Somalia/Somaliland) collected less than 10 blood donations per 1000 population per year; out of these, 25 countries collect less than half of the blood need to meet transfusion requirements. In contrast, high-income countries collect around 35 blood donations per 1000 populations per year [3]. In Somaliland, were severe blood shortage is evident, family members are often forced to donate blood or find a replacement donor during an emergency situation. This results in a financial and emotional strain and causes significant delay in getting appropriate blood. This condition may also put many lives in danger, especially women, in contracting blood borne infections since there is no time or adequate facilities to properly screen donated blood.
Over 100 million blood units are collected annually throughout the world and yet many more is needed to achieve global demand to guarantee adequate and timely availability of blood [4]. According to WHO estimates, for a country health care system to achieve minimum requirement of blood, 1% of its population has to donate. The requirement increases as the health care system advances. The average donation rate in developing countries is 15 times lower compared to developed countries. In a survey conducted by WHO in 2006 reported that more than 70 countries had blood donation rates less than the WHO established standard of 1% or 10 donations per 1000 population [5]. Of the 108 million blood donations collected globally, half of these are collected in high-income countries, home to 18% of the world’s population. The rate of blood donation in high, middle and low income countries are 36.8, 11.7 and 3.9 donations per 1000 population respectively. Within 8 years (from 2004-2012) an increase of 8.6 million donations has been reported globally. In total, 73 countries collect over 90% of their blood from voluntary un-remunerated blood donors; though the figure from other sources of blood, such as family/ replacement or paid are 50% in 72 countries [6]. Out of 193 countries, 54 countries reached 100% voluntary blood donation; of these 68% are developed countries while transitional and developing countries account for 23% and 9% respectively. The average donation rate is 31 per 1000 population in countries with 100% voluntary blood donation; were as this rate is 9 per 1000 population in countries with 50% or less voluntary blood donation. Donation rates in Africa are very low and it’s estimated at about 4.15 per 1000 population in 2006, compared to over 30 per 1000 population on average in developed countries. WHO estimated that Africa requires 8 million units of blood in 2006, but only 3.2 million units were collected. Blood requirements in many countries in the region are very insufficient and not enough is being collected for the population [2]. In Hargeisa the case is not different. Blood requirements have been estimated at 10,000 units; but only 6,000-6,500 units are collected annually, that is 4-4.33 donations per 1000 population, which is very low.
University represents a great source of blood for collection agencies. There is large population of mostly young and healthy people who can be easily reached. Regrettably, at most tertiary level institutions, most students do not intend to donate [7]. Fear of needles, pain and sight of blood, fear of future weakness, possible ill effects, ignorance and illiteracy are some reasons for many people who are hesitant in donating blood. All of the above false convictions must be removed in order for sufficient amount of blood to be made available for blood banks in saving lives [8]. Blood donation rates must be improved, especially among the youth, in order to help reduce shortages [7].
Methods and Materials
Study setting
The population of Somaliland has been estimated at approximately 3.5 million residents; the population consists of nomads (33.8%), urban (52.9%), IDPs (2.4%) and rural dwellers (11%). The capital and the largest city is Hargeisa, has a population of a little over a million residents. The annual population growth rate is 2.7%. Life expectancy at birth is 51.8. The population density has been estimated at 25 persons per square km in 2014. The approximately 3.5 million populations are served by 25 hospitals, 91 health centers, and 164 health posts. The country has one blood bank managed by Hargeisa Group Hospital, the largest referral hospital in Somaliland. The country has no blood donation policy or blood donation organizations. The health sector receives large amounts of assistance from international organizations. There are 17 institutions that offer tertiary level education [9]. The University of Hargeisa (UOH) is largest public university in the country located in the capital. The institution was founded in 2000. It has over 5000 students, and operates on a four to seven year system. The university consists of 12 faculties namely Faculty of Economics and Political Science, Faculty of Information and Communication Technology (ICT), Faculty of Law and Legal Clinic, Faculty of Engineering, Faculty of Business and Public Administration, Faculty of Arabic Language and Islamic Studies, Faculty of Applied Science, Faculty of Mathematics and Statistics with Management, Faculty of Education, Faculty of Health Science, Faculty of Agriculture and Veterinary, and Faculty of Social Science [10]. The study was conducted at UOH from March 1-12 2016.
Study design
An institution based cross sectional study design was used.
Sampling technique and sample size determination
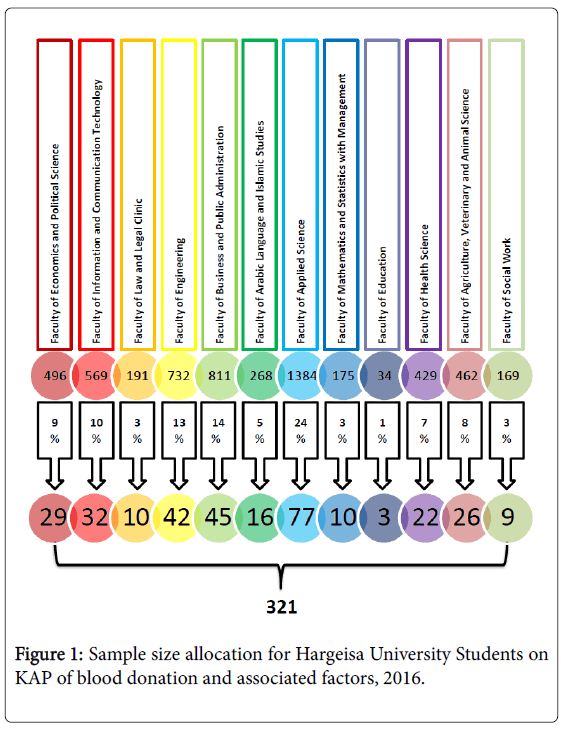
The population was stratified based on their respective college and from each strata sample was drawn (based on their respective proportion) using simple random sampling technique. A two population proportion formula was used to determine the sample size using a similar study conducted in Addis Ababa [11]. The knowledge level is 83.7% and the factor associated with it was age (OR=5). This gave a sample of 172. The Attitude level was 68% and the factor associated with it was sex (OR=2.2). This gave a sample of 292. The Practice level is 23.4% and the factor associated with it was age (OR=6.5) and sex (OR=3.9). This gave a sample of 34 and 70 respectively. To increase the power of the study the maximum sample size (292) will be considered for this study Figure 1.
n= (Zα+Z2β)2 {P1 (1−P1 + P2 (1−P2)}/ (P1−P2)2
Where:
• n= minimum sample size
• Zα= confidence interval usually at 95%
• Z2β= 1 Power (the probability that if the two proportions differ the test will produce a significant difference) usually at 80%
• P1= level of attitude at 68% or 0.68
• P2= level of factor associated with attitude (sex) at 82% or 0.82 calculated in the following manner:
P2 = ωP1 / ωP1 + (1−P1)…..
Where ω = odds ratio (OR = 2.2)
P2 = 2.2 (0.68) / 2.2(0.68) + (1−0.68) = 0.82 or 82%
n = (1.96 + 0.84)2 × {0.68(1 − 0.68) + 0.82 (1− 0.82)} / (0.68 − 0.82)2
n = 146 is the minimum sample size for one proportion.
Therefore the sample size for two proportion is 146 × 2 = 292
Data collection process
Data were collected using self-administered questionnaire which consisted of 37 questions drafted from similar studies conducted in different places. The questionnaire is subdivided into four parts; part 1 focused on socio-demographic factors of the participants, while parts 2-4 measured knowledge, attitude and practice. Data facilitators each from 2nd and 3rd year were recruited for data collection. Third year students supervised while second year student facilitated. One day training was given by principle investigators to the data facilitators and supervisors prior to data collection. The training focused on understanding the meaning of each question, obtaining consent, keeping confidentiality of the information they gathered and quality of data collection. Emphasis was given on the significance and the appropriate meanings of each question as well as how to explain for the participants in understandable manner if required.
Data quality management
To ensure data quality management the following procedures were considered:
• For ensuring data quality the questionnaire was prepared first in English, translated to Somali, and then re-translated back to English by professional translator to check its consistency.
• The questionnaire was pretested on 10% of sample number (34 students) to check the validity of the questionnaire and necessary modification was made on the instrument. Participants who were involved in the pilot study were excluded in the actual study analysis.
• Cronbach’s alpha was used to measure the reliability of the tools used to collect data. Cronbach’s alpha is a measure of internal consistency, that is, how closely related a set of items are as a group. Although the standards for what makes a “good” α coefficient are entirely arbitrary and depend on your theoretical knowledge of the scale in question, many methodologists recommend a minimum α coefficient between 0.65 and 0.8 (or higher in many cases); α coefficients that are less than 0.5 are usually unacceptable [12]. The Cronbach alpha for this study was 0.68.
• Questionnaire was checked thoroughly for its validity before it was distributed to respondents.
• At time of data collection, filled questionnaires were checked for completeness and consistency of information by the supervisor.
• Data were also checked for uniformity and completeness before entry into computer software for analysis.
• Random sample of 30% were re-entered into the double entry feature of Epi-data version 3.1 to check the consistency of the entered data.
• Multivariate logistic regression was used to control the effect of confounding.
Data processing and analysis procedure
The collected data was checked for its completeness, consistency and accuracy before analysis. A scoring mechanism was used to understand knowledge, attitude and practice level on blood donation. Each right response was given a score of 1 while a wrong, unsure or blank response was scored 0. Knowledge on blood donation was assessed using a 9-item questionnaire Total knowledge scores ranged between 0-14. Higher points indicate good knowledge. In order to identify whether students are able to answer at least half of the questions; those who have answered above the median score were considered to be having adequate knowledge and were given a score of 1. The rest were categorized as inadequate knowledge and given a score of 0.
Attitude on blood donation was assessed using a 12-item questionnaire. Total attitude scores ranged between 0-12. Higher points indicate favorable attitude. Those who have answered above the median score were considered to be having favorable attitude and were given a score of 1. The rest were categorized as unfavorable attitude and given a score of 0. Practice was assessed based on whether or not a person has donated blood. The score for a respondent who donated blood was 1 and was categorized as having good practice. If a respondent had never donated blood the score given was 0 and was categorized as bad practice. The collected data was cleaned, coded and entered into Epi Data version 3.1 and then exported to SPSS version 20 for analysis. The data obtained was tabulated and analyzed in terms of the objectives of the study using descriptive and inferential statistics. The plan of data analysis is as follows:
Descriptive statistics
• Frequency and percentage were used to assess the Socio- Demographic data and level of knowledge, attitude and practice.
Inferential statistics
• Bivariate logistic regression was used to determine the relationship of predictor on outcome variables.
• A multivariate logistic regression was used to examine the effect of two or more independent variables on a single dependent variable to test the statistical significance at 95% confidence level. P-value of <0.25 identified in bivariate analysis was considered as candidate for multivariate logistic regression; and again a P-value ≤ 0.05 at multivariate logistic regression will be considered statistically significant. Backward likelihood ratio of multivariate logistic regression was employed.
Ethical consideration
Ethical clearance was obtained from the Research Review Board (RRB) of Jimma University, College of Health Science. Secondly, research permission was obtained from Research and Community Directorate of Hargeisa University. In addition, verbal consent was obtained from all study subjects to ensure that participation was on voluntarily basis. On top of that, to keep the anonymity of study participants, code numbers rather than personal identifiers was used. Finally, all questionnaires were kept locked after data entry completion.
Results
Baseline characteristics
Out of 321 students 311 agreed to participate in the survey making the response rate 97%. The age of the respondents ranged from 17-30 years with mean age of 21.51 and Standard deviation of ± 2.298 years. Of the total participants, 172(55.3%) were males. The Majority of the respondents 297(95.5%) were single. Regarding their field (i.e. Science or Arts) and stream (Medical or Non-Medical), 174(55.9%) of the students were majoring in Science and 81(26%) were Medical students. Faculty with largest number of students was the faculty of Science. Table 1 shows the baseline characteristics of the respondents.
| Characteristics | Frequency (n=311) | Percentage (%) | |
|---|---|---|---|
| Sex | Male | 172 | 55.3 |
| Marital status | Single | 297 | 95.5 |
| Stream | Science | 174 | 55.9 |
| Field | Non-medical | 230 | 74 |
| College | Economics | 29 | 9.3 |
| ICT | 31 | 10 | |
| Law | 9 | 2.9 | |
| Engineering | 40 | 12.9 | |
| Business and Public Administration | 42 | 13.5 | |
| Islamic Studies | 15 | 4.8 | |
| Applied Science | 77 | 24.8 | |
| Mathematics, Statistics with Management | 9 | 2.9 | |
| Education | 2 | 0.6 | |
| Health Science | 22 | 7.1 | |
| Agriculture, Veterinary and Animal Science | 26 | 8.4 | |
| Social Science | 9 | 2.9 | |
| Educational Year | Year I | 91 | 29.3 |
| Year II | 75 | 24.1 | |
| Year III | 77 | 24.8 | |
| Year IV | 60 | 19.3 | |
| Year V & above | 8 | 2.6 | |
Table 1: Baseline characteristics of undergraduate students in Hargeisa University, 2016 Level of knowledge on blood donation.
One hundred and forty five (46.6%) of the respondents had adequate knowledge regarding blood donation. A total of 204(65.6%) respondents knew the common blood groups, and 232(74.6%) mentioned their own blood group. Almost half of the respondents 150(49.2%) knew the normal volume of blood in an average healthy adult.
Regarding donor eligibility requirements, 81(26%), 60(19.3%) and 33(10.6%) of the students answered correctly for the age, hemoglobin and weight level required for blood donation respectively. Similarly, 104(33.4%) and 88(28.3%) of the respondents knew the maximum amount of blood to be donated and minimum interval between two blood donation respectively.
The majority of the respondents had good knowledge of who should and who should not donate blood; however, there are some misconceptions on both groups. For instance 23(7.4%), 15(4.8%), 8(2.6%) and 8(2.6%) of the respondents answered that people younger than 18 years, greater than 60 years, diseased and vulnerable groups should donate blood; while 37(11.9%), 137(44.1%) and 44(14.1%) of the respondents answered that men, woman, and healthy people should not donate blood.
Regarding indications of blood transfusion, 84(27%) could not answer any condition, 129(41.5%) gave one correct reason, 72(23.2%) gave two correct reasons, 23(7.4%) gave three correct reasons and 3(1%) gave four correct reasons. Frequently mention reasons where people with illness such as anemia, patients undergoing surgery or pregnancy and people with serious injuries. Most of the respondents 231(74.3%) were aware of the risk of transmission of infection by transfusion. The risk of transmission of HIV was affirmed by 281(90.4%), Hepatitis B Virus 206(66.2%), Hepatitis C Virus 95(30.5%), Syphilis 96(30.9%) and Malaria 100(32.2%). Table 2 shows the details of knowledge of blood donation expressed by respondents.
| Question | Option | Frequency (311) | Percentage (%) |
|---|---|---|---|
| Do you know your blood group? | Yes | 232 | 74.6 |
| What is the normal volume of blood in an average healthy adult? | 3 liters | 20 | 6.4 |
| 4 liters | 27 | 8.7 | |
| 5 liters | 153 | 49.2 | |
| Don't Know | 111 | 35.7 | |
| Who can donate blood? | Persons b/w 20-40 years | 168 | 54 |
| Persons b/w 30-50 years | 15 | 4.8 | |
| Persons b/w 18-60 years | 81 | 26 | |
| Don't Know | 47 | 15.1 | |
| What should be the hemoglobin level for a person to donate blood? | Not less than 10.5 mg/dl | 30 | 9.6 |
| Not less than 11.5 mg/dl | 16 | 5.1 | |
| Not less than 12.5 mg/dl | 60 | 19.3 | |
| Don't Know | 205 | 65.9 | |
| What should be the body weight for a person to donate blood? | Not less than 55 kg | 106 | 34.1 |
| Not less than 50 kg | 77 | 24.8 | |
| Not less than 45 kg | 33 | 10.6 | |
| Don't Know | 95 | 30.5 | |
| What is the amount of blood withdrawn during a single blood donation? | Less than 500 m/l | 104 | 33.4 |
| Between 500-1000 m/l | 110 | 35.4 | |
| Greater than 1000 m/l | 14 | 4.5 | |
| Don’t know | 83 | 26.7 | |
| How often can donation be done? | Once in every 2-3 months | 88 | 28.3 |
| Twice in every 2-3 months | 31 | 10 | |
| Once in every 6 months | 99 | 31.8 | |
| Don’t know | 93 | 29.9 | |
| Question | Option | Frequency (311) | Percentage (%) |
| Who should donate? | Men | 259 | 39.8 |
| (multiple response question) | Women | 71 | 10.9 |
| Younger than 18 years | 23 | 3.5 | |
| Greater than 60 years | 15 | 2.3 | |
| Healthy | 267 | 41 | |
| Diseased | 8 | 1.2 | |
| Vulnerable groups | 8 | 1.2 | |
| Who should not donate? | Men | 37 | 4.4 |
| (multiple response question) | Women | 137 | 16.2 |
| Younger than 18 years | 121 | 14.3 | |
| Greater than 60 years | 122 | 14.4 | |
| Healthy | 44 | 5.2 | |
| Diseased | 220 | 26 | |
| Vulnerable groups | 165 | 19.5 | |
| Can a person be infected by receiving blood transfusion? | Yes | 231 | 74.3 |
| No | 52 | 16.7 | |
| Don't know | 28 | 9 | |
| What diseases are transmissible by blood transfusion? | HIV | 281 | 36.1 |
| (multiple response question) | HBV | 206 | 26.5 |
| HCV | 95 | 12.2 | |
| Syphilis | 96 | 12.3 | |
| Malaria | 100 | 12.9 |
Table 2: Level of knowledge on blood donation among undergraduate students in Hargeisa University, 2016.
Factors associated with knowledge on blood donation
Bivariate analysis identified field of study (medical), faculty and educational year as potential candidates for multivariate logistic regression. After controlling for the effects of potentially confounding variables using multivariate logistic regression, only field of study was found to be a statistically significant predictor level of knowledge. Students majoring in the medical field were 3 times [AOR: 2.591, 95% CI: 1.518, 4.422] more likely to be more knowledgeable relative to students majoring in non-medical field. The Table 3 shows the details of factors associated with knowledge level of blood donation.
| Variable | Knowledge | COR | 95% CI | AOR | 95% CI | ||||
|---|---|---|---|---|---|---|---|---|---|
| Adequate knowledge | Inadequate knowledge | Upper limit | Lower limit | Upper limit | Lower limit | ||||
| Age | 145 | 166 | 1.045 | 0.948 | 1.152 | - | - | - | |
| Sex | Male | 82 | 90 | 1.099 | 0.702 | 1.721 | - | - | - |
| Female | 63 | 76 | 1 | - | - | - | |||
| Field | Medical | 52 | 29 | 2.641 | 1.562 | 4.466 | 2.591 | 1.518 | 4.422 |
| Non-medical | 93 | 137 | 1 | - | - | 1 | - | - | |
| Faculty | Economics | 10 | 19 | 1 | - | - | - | - | - |
| ICT | 13 | 18 | 1.372 | 0.482 | 3.908 | - | - | - | |
| Law | 2 | 7 | 0.543 | 0.095 | 3.118 | - | - | - | |
| Engineering | 23 | 17 | 2.571 | 0.956 | 6.915 | - | - | - | |
| Buss & Public Admin | 18 | 24 | 1.425 | 0.535 | 3.796 | - | - | - | |
| Islamic | 6 | 9 | 1.267 | 0.35 | 4.582 | - | - | - | |
| App Sci | 47 | 30 | 2.977 | 1.22 | 7.265 | - | - | - | |
| MSM | 4 | 5 | 1.52 | 0.332 | 6.96 | - | - | - | |
| Health Science | 11 | 11 | 1.9 | 0.612 | 5.902 | - | - | - | |
| Agri, Vet & Animal Science | 7 | 19 | 0.7 | 0.22 | 2.225 | - | - | - | |
| Social Science and Edu | 4 | 7 | 1.086 | 0.255 | 4.617 | - | - | - | |
| Year of study | Year I | 44 | 47 | 1 | - | - | 1 | - | - |
| Year II | 39 | 36 | 1.157 | 0.628 | 2.133 | 1.144 | 0.612 | 2.139 | |
| Year III | 26 | 51 | 0.545 | 0.291 | 1.019 | 0.552 | 0.291 | 1.047 | |
| Year IV | 30 | 30 | 1.068 | 0.557 | 2.05 | 1.151 | 0.591 | 2.24 | |
| Year V & above | 6 | 2 | 3.205 | 0.614 | 16.72 | 2.728 | 0.505 | 14.748 | |
*Indicates statistical significant association
Table 3: Factors associated with knowledge level on blood donation among undergraduate students in Hargeisa University, 2016.
Attitude towards blood donation
One hundred and forty six (46.9%) of the respondents had favorable attitude towards blood donation. Three hundred (96.5%) respondents said that blood donation is a good thing to do. Voluntary donation was accepted as the best source of blood by 271(87.1%), replacement donor by 17(5.5%), remunerated by 2(0.6%) and the remaining 21(6.8%) had no knowledge of It. fifty eight (18.6%) of the respondents said that blood donation had adverse effect on the donor, 150(48.2%) disagreed with the above notion while 103(33.1%) were uncertain. In relation with the above question; 145(46.6%), 63(20.3%) and 101(32.5%) of the respondents stated that a donor might become weak, contract infection and fall sick respectively. From the total respondents, 242(77.8%) of the respondents said that patients relative should be asked to donate blood; and that 277(89.1%) agreed that relatives should be encouraged to donate blood. Regarding to their willingness to donate blood, 254(81.7%) respondents were ready to donate if called upon or reminded to do so. Table 4 shows the detail attitude level of respondents regarding to blood donation.
| Question | Option | Frequency (311) | Percentage (%) |
|---|---|---|---|
| Blood donation is good thing to do? | Yes | 300 | 96.5 |
| No | 2 | 0.6 | |
| Don’t know | 9 | 2.9 | |
| What do you think is the best source of blood donation? | Voluntary | 271 | 87.1 |
| Replacement | 17 | 5.5 | |
| Remunerated | 2 | 0.6 | |
| Don’t know | 21 | 6.8 | |
| Only males are allowed to donate? | Yes | 155 | 49.8 |
| No | 92 | 29.6 | |
| Don’t know | 64 | 20.6 | |
| Only physically strong people should donate? | Yes | 28 | 9 |
| No | 195 | 62.7 | |
| Don’t know | 88 | 28.3 | |
| Blood donation can lead to anemia? | Yes | 130 | 41.8 |
| No | 74 | 23.8 | |
| Don’t know | 107 | 34.4 | |
| Blood donation can lead to reduced immunity? | Yes | 127 | 40.8 |
| No | 82 | 26.4 | |
| Don’t know | 102 | 32.8 | |
| Blood donation has adverse effect on the donor? | Yes | 58 | 18.6 |
| No | 150 | 48.2 | |
| Don’t know | 103 | 33.1 | |
| Blood donation cause weakness? | Yes | 145 | 46.6 |
| No | 94 | 30.2 | |
| Don’t know | 72 | 23.2 | |
| Blood donation can cause infection? | Yes | 63 | 20.3 |
| No | 136 | 43.7 | |
| Don’t know | 112 | 36 | |
| Blood donation can cause a person to fall sick? | Yes | 101 | 32.5 |
| No | 122 | 39.2 | |
| Don’t know | 88 | 28.3 | |
| I am scared of donating blood? | Yes | 117 | 37.6 |
| No | 165 | 53.1 | |
| Don’t know | 29 | 9.3 | |
| A patient’s relative should be asked to donate? | Yes | 242 | 77.8 |
| No | 42 | 13.5 | |
| Don’t know | 27 | 8.7 | |
| Will you donate if called upon or reminded to do so? | Yes | 254 | 81.7 |
Table 4: Attitude level on blood donation among undergraduate students in Hargeisa University, 2016.
Factors associated with attitude towards blood donation
Bivariate analysis identified field of study (Medical) and being a student at the faculty of Applied Science, Health Science and Social Science as potential candidates for multivariate logistic regression. Being a student at the faculty of Applied Science, Health Science and Social Science showed statistical significant association in the multivariate analysis. Students in the faculty of Applied Science, Health Science and Social Science were 3, 4, 10 times [AOR: 2.8, 95% CI: 1.136, 6.956, AOR: 3.8, 95% CI: 1.205, 12.554 and AOR: 10.00, 95% CI: 1.786, 55.976] more likely to have positive attitude towards blood donation relative to students in the faculty of Economics. Table 5 shows details of factors associated with attitude level of blood donation.
| Variable | Attitude | COR | 95% CI | AOR | 95% CI | ||||
|---|---|---|---|---|---|---|---|---|---|
| Favorable attitude | Unfavorable attitude | Upper limit | Lower limit | (Upper limit | Lower) limit | ||||
| Age | 146 | 165 | 1.018 | 0.924 | 1.122 | - | - | - | |
| Sex | Male | 81 | 91 | 1.013 | 0.647 | 1.586 | - | - | - |
| Female | 65 | 74 | 1 | - | - | - | - | - | |
| Field | Medical | 47 | 34 | 1.829 | 1.095 | 3.054 | - | - | - |
| Non-medical | 99 | 131 | 1 | - | - | - | - | - | |
| Faculty | Economics | 9 | 20 | 1 | - | - | 1 | - | - |
| ICT | 9 | 22 | 0.909 | 0.301 | 2.744 | 0.909 | 0.301 | 2.744 | |
| Law | 4 | 5 | 1.778 | 0.384 | 8.228 | 1.778 | 0.384 | 8.228 | |
| Engineering | 21 | 19 | 2.456 | 0.902 | 6.69 | 2.456 | 0.902 | 6.69 | |
| Business & Public Admin | 19 | 23 | 1.836 | 0.679 | 4.96 | 1.836 | 0.679 | 4.96 | |
| Islamic | 4 | 11 | 0.808 | 0.202 | 3.24 | 0.808 | 0.202 | 3.24 | |
| Applied Sci | 43 | 34 | 2.81 | 1.136 | 6.956 | 2.81 | 1.136 | 6.956 * | |
| MSM | 5 | 4 | 2.778 | 0.6 | 12.856 | 2.778 | 0.6 | 12.856 | |
| Health Sci | 14 | 8 | 3.889 | 1.205 | 12.554 | 3.889 | 1.205 | 12.554* | |
| Agri, Vet & Animal Sci | 9 | 17 | 1.176 | 0.381 | 3.634 | 1.176 | 0.381 | 3.634 | |
| Social Sci and Edu | 9 | 2 | 10 | 1.786 | 55.976 | 10 | 1.786 | 55.976* | |
| Year of study | Year I | 46 | 45 | 1 | - | - | - | - | - |
| Year II | 33 | 42 | 0.769 | 0.416 | 1.42 | - | - | - | |
| Year III | 30 | 47 | 0.624 | 0.337 | 1.155 | - | - | - | |
| Year IV | 31 | 29 | 1.046 | 0.545 | 2.007 | - | - | - | |
| Year V & above | 6 | 2 | 2.935 | 0.562 | 15.315 | - | - | - | |
Table 5: Factors associated with attitude level of blood donation among undergraduate students in Hargeisa University, 2016.
Practice of blood donation
Pertaining blood donation practice of participants, only thirty five students (11.3%) have ever donated blood. When it comes to the frequency of donation by donors, 23(65.7%) donated once while 12(34.3%) donated more than once. Out of total donors, only six (17.1%) donated blood on regular basis. Most 27(77.1%) donated blood because a family or a friend needed blood and 8(23.5) donated on voluntary basis. Majority of the students 276(88.7%) had never donated blood. The three frequently mentioned reason for nondonation were not approached 120(38.6%), fear of repercussion that may be caused by blood donation 72(23.1%) and lack of information 65(20.9%). Table 6 shows details of blood donation practice among students.
| Question | Option | Frequency (n=311) | Percentage (%) |
|---|---|---|---|
| Have you ever donated blood? | Yes | 35 | 11.3 |
| How many times have you donated blood? | 1 time | 23 | 65.7 |
| 2-3 times | 9 | 25.7 | |
| 4-5 times | 1 | 2.9 | |
| 6 times or more | 2 | 5.7 | |
| Main reason for donation? | A family or friend needed blood | 27 | 77.1 |
| Voluntary | 8 | 22.9 | |
| Main reason for non-donation? | Not approached | 120 | 38.6 |
| Lack of information | 65 | 20.9 | |
| Need to donate for family or friend in the future | 16 | 5.1 | |
| Parents don’t allow | 16 | 5.1 | |
| Unfit to donate | 13 | 4.2 | |
| fear of repercussion caused by blood donation | 72 | 23.1 | |
| Donated blood may be sold | 4 | 1.3 | |
| No remuneration | 5 | 1.6 |
Table 6: Practice of blood donation among undergraduate students in Hargeisa University, 2016 Factors associated with practice of blood donation.
Bivariate analysis showed age, sex (male) and year of study (year 5 and above) as potential candidates for multivariate logistic regression. In multivariate analysis, age and sex (male) showed statistical significance association. The difference of 1 year between respondents age increases the likelihood to donate blood by 1.3 times [AOR: 1.284, 95% CI: 1.078, 1.530] keeping sex (male) constant. On the hand, males were 7 times [AOR: 7.465, 95% CI: 2.104, 26.487] more likely to donate blood as compared to females keeping age constant. Table 7 shows the details of factors associated with practice of blood donation.
| Variable | Practice | COR | 95% CI | AOR | 95% CI | ||||
|---|---|---|---|---|---|---|---|---|---|
| Good Practice | Bad Practice | Upper limit | Lower limit | Upper limit | Lower limit | ||||
| Age | 35 | 276 | 1.334 | 1.156 | 1.539 | 1.284 | 1.07 | 1.530* | |
| Sex | Male | 32 | 140 | 10.36 | 3.1 | 34.64 | 7.465 | 2.104 | 26.487* |
| Female | 3 | 136 | 1 | - | - | 1 | - | - | |
| Field | Medical | 9 | 72 | 0.981 | 0.439 | 2.192 | - | - | - |
| Non-medical | 26 | 204 | 1 | - | - | - | - | - | |
| Faculty | Economics | 3 | 26 | 1 | - | - | 1 | - | - |
| ICT | 0 | 31 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Law | 2 | 7 | 2.476 | 0.344 | 17.832 | 1.646 | 0.182 | 14.863 | |
| Engineering | 5 | 35 | 1.238 | 0.271 | 5.653 | 1.411 | 0.29 | 6.861 | |
| Buss & Public Admin | 5 | 37 | 1.171 | 0.257 | 5.337 | 2.237 | 0.445 | 11.238 | |
| Islamic | 0 | 15 | 0 | 0 | 0 | 0 | 0 | 0 | |
| App Science | 5 | 72 | 0.602 | 0.134 | 2.697 | 1.219 | 0.251 | 5.912 | |
| MSM | 2 | 7 | 2.476 | 0.344 | 17.832 | 3.683 | 0.445 | 30.502 | |
| Health Sci | 5 | 17 | 2.549 | 0.538 | 12.087 | 2.756 | 0.532 | 14.275 | |
| Agri, Vet & Animal Sci | 8 | 18 | 3.852 | 0.898 | 16.53 | 3.887 | 0.837 | 18.061 | |
| Social Sci and Education | 0 | 11 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Year of study | Year I | 6 | 85 | 1 | - | - | - | - | - |
| Year II | 5 | 70 | 1.012 | 0.296 | 3.456 | - | - | - | |
| Year III | 12 | 65 | 2.615 | 0.932 | 7.339 | - | - | - | |
| Year IV | 8 | 52 | 2.179 | 0.716 | 6.635 | - | - | - | |
| Year V & above | 4 | 4 | 14.167 | 2.819 | 71.183 | - | - | - | |
Table 7: Factors associated with practice of blood donation among undergraduate student in Hargeisa University, 2016.
Discussion
Maintaining an adequate and safe supply of blood is an issue of concern to health planners, especially with the increase in demand. In this study an attempt has been made to assess the level and factors associated with knowledge attitude and practice of students on voluntary blood donation.
In this study only 46.6% of the students had adequate knowledge about blood donation. The current finding is almost similar with previous studies conducted on university students in Thailand and Ethiopia; were the knowledge level was 42.7% and 40.04% respectively [13,14]. A little over a quarter (28.4%) said that the minimum frequency of donation was every three months. This is lower than in studies conducted on health or medical students in Ethiopia and India were the rate was 40.09% and 59.63% respectively [11,15]. The reason may be perhaps in the above studies the participants were exclusively medical or health students; while in this study, participants come from both medical and non-medical colleges. Being a student in the medical field was found to be a significant predictor of level of knowledge.
In this study, less than half of the respondents (46.9%) had favorable attitude towards blood donation. This is comparable to a study conducted on regular students in Ambo University, Ethiopia, were the rate was 47.7% [14]. Almost all of the respondents (96.5%) said that blood donation is a good thing to do which is slightly higher than studies conducted on students in Kathmandu (82.5%) and two studies conducted in Nigeria on physicians (89%) and health care workers (81.6%) in the University of Benin Teaching Hospital [16-18]. Eighty two percent of the respondents were ready to donate blood if called upon or reminded to do so. This is smaller than a study conducted on health students in Addis Ababa University; were the figure was 100% [11]. This may be due to the fact that large number of females believes that they are not eligible or not allowed to donated blood. Being a student in the faculty of Social Science was found to be significant predictor of attitude towards blood donation.
Less than one quarter, (11.3%) of the respondents has ever donated blood. This is comparable to WHO report on percentage of blood donors among WHO African countries, which categorized Somalia in the lowest group. This supports that blood donation rates are considerably less in developing countries when compared to developed countries [6]. The major reason for those who have donated blood was a family or friend needed blood (76.5%). This is greater than in a study conducted among university students in Saudi Arabia 30% [18]. The main reason may be because the only source of blood donation in Somaliland is replacement and people occasionally donate blood voluntarily. The major reason for non-donation were not approached to donate (39.5%) and no information as to when, where or how to donate (21.1%). Age and sex (male) was found to be significant predictor of practice towards blood donation. This is similar to a study conducted on health science students in Addis Ababa University were age and sex were also significant predictors of blood donation practice [11].
Even though these students represent a large healthy source of blood donation, this clearly shows that there is a serious need for sensitization and education to all; and to encourage them to go to the blood bank for blood donation.
Conclusion
This study revealed the student’s level of knowledge about blood donation in Hargeisa University is very low; above half of the respondents have adequate knowledge on blood donation with significant predictor of level of knowledge was field of study (belonging to a medical field). Similarly, more than half of the respondents had unfavorable attitude towards voluntary blood donation and factors associated with attitude was faculty (being a student at the faculty of Applied Science, Health Science and Social Science).
Finally, this study identified that blood donation practice was very low. Small number of the respondents had ever donated blood. Significant predictors of blood donation were age and sex (male). This reflects that KAP of students towards blood donation were affected by different socio-demographic characteristics of the respondents. These factors should be emphatically considered during blood donation program development.
Recommendation
Since youth represent the largest share of Somaliland’s population and since many of them could be found in the universities; and in order to solve and overcome blood shortages in this country and based on the findings of this study the following recommendations are suggested:
• Regional Red Crescent should use school mini media, Radio, TV programs to create awareness among University students, to increase knowledge, positively influence individual’s unsupportive attitude toward blood donation. Informing audience during health education to consider higher institutions periodic sensitization, and addressing the place where voluntary blood donation was taken place.
• Employing educated individuals and political leaders in the University by participating in voluntary blood donation to break the poor attitude of students toward blood donation could be some solutions.
• Ministry of health in collaboration with Hargeisa Group Hospital would be better to strengthen working on voluntary blood donation by using mass media, school health education and provide counseling for those who donated blood on the center for replacement or voluntary and also extended emphasis to University students to encourage educated people and particularly students to donated blood regularly to solve shortage blood in the country.
• As baseline data to Understanding what Somalilanders know and what they do in terms of voluntary blood donation will serve the local authorities in planning and implementing measures to improve the national blood program, including the education, recruitment and service of donors.
Author’s Contributions
Abdirahman Omer Ahmed: Conceptualized the study, designed the study instrument, conducted the data collection and analysis and wrote the first draft and final draft of the manuscript.
Competing Interests
The author declares that there is no competing interest.
Acknowledgements
First and foremost my heartily felt gratitude goes to almighty Allah. I would also like to jointly acknowledge Jimma University’s College of Health Science and ABH Services PLC for giving me the opportunity in developing this thesis. My earnest appreciation goes to my advisors: Prof. Abraham Haileamlak and Mr. Alamayehu Atomsa for their inspiring guidance, constant encouragement and constructive criticism. Their guidance at different stages of this paper has not only enabled me in drafting this research, but would have not been possible to complete. Finally, I would like to acknowledge the support of Hargeisa University administration for their unwavering cooperation and assistance in providing timely and relevant information.
References
- Nwabueze S, Nnebue C, Azuike E, Ezenyeaku C, Aniagboso C et al. (2014) Perception of blood donation among medical and pharmaceutical students of Nnamdi Azikiwe University, Awka. Open J PrevMed 4: 515-522.
- (2010) World Health Organization and International Federation of Red Cross and Red Crescent Societies.
- World Health Organization (2014) World blood donor day 2014: Safe blood needed to save mothers.
- Wiwanitkit V (2002) Knowledge about blood donation among a sample of Thai University students. Vox Sang 83: 97-99.
- WHO (2007) Blood safety indicators, 2007: Global database on blood safety. Geneva.
- World Health Organization (2015) Blood safety and availability. Geneva.
- Allerson J (2012) Assessment of selected university students' knowledge of blood donation and the relationship with intent to donate blood. Mankato: Minnesota State University, Public Health.
- WHO (2006) Blood donation safety report. Geneva 92:14-7.
- Ministry of National Planning and Development (2015) Somaliland in figures. Annual report, Hargeisa: Republic of Somaliland.
- University of Hargiesa
- Misganaw C, Meaza T, Deresea A, Tesfaye M, Tessema TT, et al. (2014) The level and associated factors of knowledge, attitude and practice of blood donation among health science students of addis ababa University. Int J Med Res Health Sci 1: 105-118.
- Goforth C (2015) Using and Interpreting Cronbach's Alpha. Research Data Services + Sciences.
- Nigatu A, Demissie DB (2014) Knowledge, attitude and practice on voluntary blood donation and associated factors among Ambo University regular students, Ambo Town, Ethiopia. J Community Med Health Educ 4: 315.
- Smriti V, Stuti S, Tejvansh SI, Vaibhav M (2014) Awareness and knowledge of blood donation among medical faculty and students in Vadodar District. Int J Sci Res 3: 304-308.
- Mrigendra A (2013) Study on knowledge, attitude and practice of blood donation among students of different college of kathmandu, Nepal. Int J Pharm Biol Arch 4: 424-428.
- Benedict N, Usimenahon A, Alexander NI, Isi A (2012) Knowledge, attitude and practice of voluntary blood donation among physicians in a tertiary health facility of a developing country. J Blood Disord Transfus 3: 1-4.
- Nwogoh B, Aigberadion U, Nwannadi AI (2013) Knowledge, attitude, and practice of voluntary blood donation among healthcare workers at the University of Benin teaching hospital, Benin City, Nigeria. J Blood Transfus 1-6.
- Baig M, Hamed H, Abdullah HH, Faisal TA, Abdulelah MN, et al. (2013) Knowledge, misconceptions and motivations towards blood donation among University students in KSA. Pak J Med Sci 29: 1295-1299.
Relevant Topics
- Addiction
- Adolescence
- Children Care
- Communicable Diseases
- Community Occupational Medicine
- Disorders and Treatments
- Education
- Infections
- Mental Health Education
- Mortality Rate
- Nutrition Education
- Occupational Therapy Education
- Population Health
- Prevalence
- Sexual Violence
- Social & Preventive Medicine
- Women's Healthcare
Recommended Journals
Article Tools
Article Usage
- Total views: 5198
- [From(publication date):
August-2017 - Nov 21, 2024] - Breakdown by view type
- HTML page views : 4341
- PDF downloads : 857