Kinesio® Tex Tape: Valuable Conservative Treatment for Plantar Fasciitis?
Received: 24-Aug-2015 / Accepted Date: 08-Sep-2015 / Published Date: 16-Sep-2015 DOI: 10.4172/2165-7025.1000271
Abstract
Purpose: To determine if Kinesio Taping® as a therapeutic intervention will decrease plantar pain and improve functional outcomes in individuals with plantar fasciitis (PF).
Methods: 10 (7 F/3 M; mean age 40.3 years old) subjects reported for three sessions: baseline measurements, after 1 week of taping application, and after 3 weeks of taping application. At each session, the following data were collected: 1) Musculoskeletal Ultrasound (MSK US) imaging of plantar fascia thickness via a long-axis scan at the insertion of the calcaneus; 2) Numerical Pain Rating Scale (NPRS); and 3) Foot and Ankle Ability Measure Scores (FAAM). At the initial session, patients were instructed on Kinesio Taping® protocol and supplied with enough product for daily re-application throughout the study. A 1-way ANOVA was used to compare the outcome measures from the three visits.
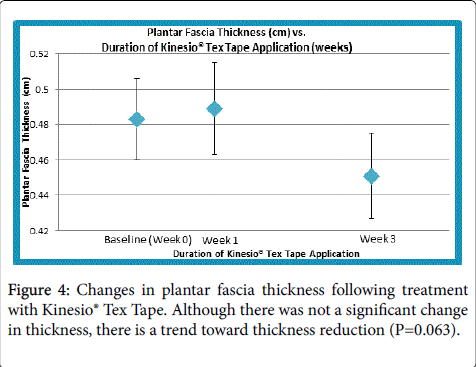
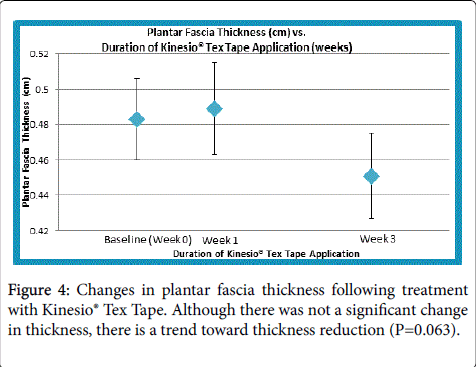
Results: There was a trend towards significant decrease in thickness between the baseline and final measures (P=0.063). This study also revealed a significant and clinically meaningful decrease in NPRS scores (MCID=2) from baseline measurement to week 3 (P=0.031). No significant changes in FAAM scores for the ADL (P=0.639) or Sports (P=0.107) subscales were revealed over the treatment period.
Conclusion: Kinesio Taping® may be considered an effective, conservative, and practical intervention in the treatment of plantar fasciitis for short-term pain relief when used with the exercise protocol. However a larger sample sized study with a control group is needed to warrant these results.
Keywords: Plantar fasciitis; Musculoskeletal ultrasound; Kinesio® Tex Tape
360985Introduction
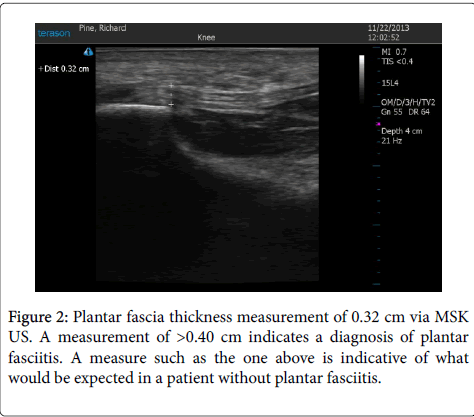
Plantar Fasciitis is the most common cause of heel pain in patients to the outpatient clinic [1]. Up to 10% of the United States population may present with heel pain over the course of their lives [2] which underscores the importance of evidence based interventions. Plantar fasciitis is thought to be caused by biomechanical overuse from prolonged standing or running, thus creat-ing microtears at the calcaneal enthesis [3–5]. Some experts have deemed this condition “plantar fasciosis,” implying that its etiology is a more chronic degenerative process versus acute inflammation [4,5]. An emerging diagnostic trend relies on measuring plantar fascia with musculoskeletal ultrasound (MSK US). Increased plantar fascia thickness is demonstrated by an image of increased thickness and hypoechogenity of the tissue with many studies suggesting that a result greater than 0.4 cm is considered to be indicative of plantar fasciitis [5]. Plantar fascia thickness greater than 0.4 cm allows a more homogenous group when studying people with plantar fasciitis vs subjective complaints and palpation alone. MSK US imaging technique is increasingly being used to assess plantar fascia thickness, monitor the effect of different interventions and guide therapeutic interventions in patients with Plantar Fasciitis [6].
Numerous treatment modalities have been employed with varying results [6–11]. One intervention growing in popularity is Kinesio® Tex Tape. Kinesio® Tex Tape is marketed to be an easy-to-use, easily-accessible, and cost-effective treatment option. Several theories have been proposed to describe its effect. The most widely-accepted theory states that the tape simulates the elasticity of skin and serves to pull the outer layer of skin off the underlying muscle and soft tissue structures, improving muscle function and kinesthetic awareness, decreasing pressure on soft tissues, and creating a larger space and channel for enhanced lymph flow [6]. However, little empirical exists to support its efficacy as a treatment intervention for plantar fasciitis. There is limited evidence from one moderate quality randomized control trial (RCT) using Kinesio® Tex Tape in conjunction with physiotherapy that was clinically beneficial for plantar fasciitis related pain in the short term; however, there are serious questions around the internal validity of this RCT [7]. Evidence suggests that Kinesio® Tex Tape is a positive intervention for other musculoskeletal disorders [8]. The purpose of this study is to determine if Kinesio Taping® as a short-term therapeutic intervention will decrease pain and improve functional outcomes using MSK US to monitor the effect of the intervention.
Materials and Methods
Participants
All subjects were recruited from local specialty running stores, the Elon University school population, and the general public in the Piedmont Triad area of North Carolina. Before beginning the program, subject read and signed the consent form approved by the University IRB.
Inclusion criteria were as follows: at least 18 years of age; plantar fascia thickness greater than or equal to 4 mm measured by musculoskeletal ultrasound, [9] heel pain maximal over the plantar aspect of the foot; symptoms lasting at least 6 weeks, [10] maximal intensity of pain in the previous week equal to or greater than 3 on the Numeric Pain Rating Scale (NPRS); and no history of any systemic disease or recent foot surgery. Demographics are displayed in Table 1.
| Subject | Gender | Age | Height (inches) | Weight (lbs) |
| 1 | F | 43 | 63.25 | 159 |
| 2 | M | 44 | 69 | 174 |
| 3 | F | 27 | 70 | 159 |
| 4 | M | 52 | 70 | 178.5 |
| 5 | F | 55 | 64 | 139 |
| 6 | M | 47 | 74 | 212.25 |
| 7 | F | 39 | 63.5 | 200 |
| 8 | F | 32 | 63.5 | 141 |
| 9 | F | 29 | 63 | 132 |
| 10 | F | 35 | 70 | 238.3 |
Table 1: Demographic data of subjects.
Exclusion criteria includes: experience with previous Kinesio taping application; current therapeutic exercise prescription, or use of other interventions including steroid injections or NSAIDS [11,12].
Intervention
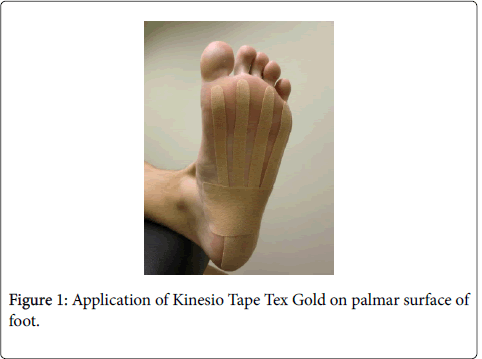
All subjects were assigned to Kinesio Tape treatment. Specifically Kinesio Tex Gold tape was used. On day 1, all subjects completed the NPRS for the most affected foot, the Foot and Ankle Ability Measure survey (FAAM), a physical exam of the ankle, and an initial MSK US to provide a baseline measure of the plantar fascia thickness. Kinesio Tape was placed on the plantar surface of the foot on day 1. Tape was applied by an investigator trained in the application of Kinesio Tape Tex Gold to the foot by a Kinesio certified taping specialist.
The tape was cut to the length, that when stretched, would cover the foot from the posterior calcaneus to the metatarsal heads. . Four fans were cut into the tape lengthwise leaving a solid anchor piece applied to the calcaneus. The fans were stretched with 100% tension to the metatarsal heads. This was followed by placing a second strip, half the length of the first, from the lateral midfoot pulling medially with 50% tension across the arch. All anchors were applied without tension to avoid skin irritation (Figure 1). Each subject was trained on how to reapply the tape in the event of the tape falling off, and enough Kinesio Tape was supplied to each subject for daily if necessary.
Subjects were instructed to continue current activities but not to increase levels of activity beyond what they had been doing prior to the study. All subjects returned 1 week after the pre-tests to complete another NPRS, FAAM, physical exam, and MSK US. At this time, subjects were taped again. At the beginning of the 4th week, all subjects reported a final time for post-testing of MSK US, NPRS, FAAM, and physical exam.
Primary outcome: MSK US
The primary outcome measurement is the plantar fascia thickness measured with MSK US. This was performed in accordance with the protocol outlined by the European Society of Musculoskeletal Radiology [13]. A diagnostic ultrasound machine, T3200/Terason Ultrasound Imaging System Version 5.2/22Hz/Depth 3 cm/MSK Ankle and Foot default setting was used. Subjects were positioned in a prone position with their involved foot hanging off the examination table. The investigators placed the transducer in over the plantar aspect of the hind foot to examine the insertion of the plantar fascia on the calcaneus. Long-axis scans generated slightly medial to the midline of the foot were used. Following the image generation, investigators saved the picture into a secured file. The thickness of the fascia was measured from the point where the fascia emerges from the calcaneal tuberosity using on-screen calipers. Three images and measurements of the involved foot of each subject were generated and plantar fascia thickness was determined by taking the average of the three measurements (Figures 2 and 3).
Secondary outcomes
The 3 secondary outcome measurements include:
Pain measurement of the affected foot via the 11-point NPRS. The NPRS was utilized for heel pain assessment, ranging from 0 (no pain) to 10 (worst imaginable pain). This scale has been demonstrated to be a sensitive, [14] reliable, generalizable, and internally consistent measure of clinical and experimental pain sensation intensity. A change of 2 points in the NPRS has been established as a clinically meaningful change [15].
2) Physical function was measured by the FAAM survey [11,16]. The FAAM is a reliable, responsive, and valid measure of physical function for individuals with a broad range of musculoskeletal disorders of the lower leg, foot, and ankle [17]. It has been validated in a physical therapy practice setting [11]. This outcome measures has a high internal consistency of 0.98. ICC for the ADL and Sport subscale is 0.87 (SEM, 2.1) and 0.89 (SEM 4.5) respectively; the Guyatt's responsiveness index is 2.75 and 1.40 respectively [18] and test retest reliability was 0.89 and 0.87 respectively [18].
3) Physical exam of the affected foot through active and passive range of motion for dorsiflexion (DF) and plantar flexion (PF); gastrocnemius/soleus muscle length measurement; and manual muscle testing (MMT) of inversion, eversion, DF, PF, toe flexion. Intratester reliability (ICC, 0.47-0.96) for ankle ROM testing using a universal goniometer [15].
Data Analysis
Data was checked for normality using the One-Sample Kolmogorov-Smirnov test. Given that the data was normally distributed, a one-way ANOVA with time (baseline – Week 0, Week 1 and Week 3) as a repeated-measures factor was performed. For significant results, pairwise comparisons were done using Bonferroni post hoc analysis. All computations were performed using SPSS 20 software (IBM, Armonk, NY). The α-value was set at 0.05.
Results
There was no statistically significant change with a small to moderate effect size in plantar fascia thickness over the course of this study (F = 3.246; p = 0.063; η2 = 0.265; Power = 0.544). However, after an initial slight average increase in plantar fascia thickness from baseline to week 1, subjects trended toward a reduction in thickness to post-testing after week 3 (Figure 4).
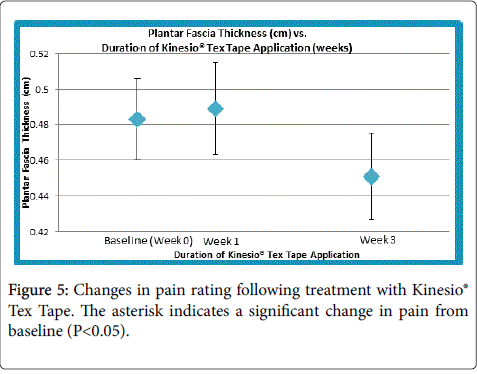
There was a statistically significant change with small to moderate effect size observed among subjects’ self-reported NPRS ratings at post-testing (F = 6.341; p = 0.008; η2 = 0.413 Power = 0.841). Specifically, post hoc analysis showed that subjects’ pain ratings decreased from an average of 5.8 at baseline to 3.6 after week 3 (p = 0.031; Figure 5). This difference of 2.2 points meets the minimally clinical important difference (MCID) of 2 points. Individually, half of the subjects reported at least a 2 point decrease (improvement) in pain scores throughout the study duration.
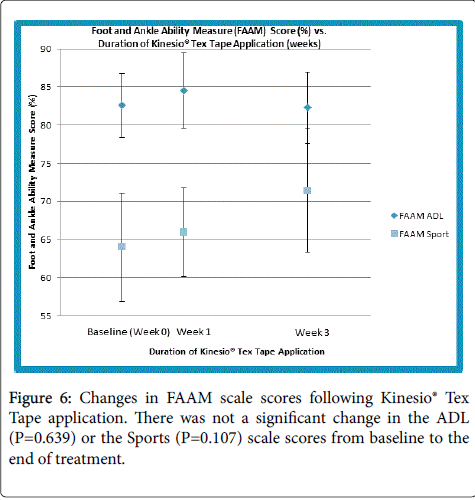
No statistically significant change with small effect size in FAAM ADL ((F = 0.236; p = 0.792; η2 = 0.026; Power = 0.081)) and Sports ((F = 2.537; p = 0.107; η2 = 0.442)) subscale scores was observed (Figure 6). The average ADL subscale scores were virtually unchanged from baseline to post-testing, but average sport subscale scores showed an average improvement of roughly 8 points (MCID=9 points) over the duration of the study.
Discussion
Results from this study suggest that there is a tendency for Kinesio Tape to be effective for decreasing plantar fascia thickness as the data trends toward a significant decrease in thickness between the baseline and measurement at week 3. To the best of our knowledge, this is the first time MSK US has been used as a dependent variable for plantar fasciitis and its relationship with Kinesio taping®. This study also reveals a significant and MCID decrease in NPRS (MCID=2) from baseline measurement to week 3. No significant changes in FAAM scores were found over the treatment period.
Interestingly, the thickness values slightly increased after 1 week of Kinesio taping® but decreased thereafter. This could probably reflect the acute effects of the procedure and highlight the need for a longer taping period. This is further strengthened by a significant decrease in the pain score after a longer intervention period than 1 week with a small to moderate effect size. Though the functional measures for ADL and sport showed no significant change acutely or after 3 weeks, trends for data and effect sizes could suggest that Kinesio taping® may be more sensitive to improve sports-related performance than ADL-related performance. Non-significant changes to both the ADL and sport FAAM scores might have been due to ceiling effect of the scores for both the measures.
During this study, subjects maintained all regular activities and shoe wear and were restricted from receiving additional treatment. The demographics of our subjects (Lifestyle, age, height, and weight of subjects) were variable and seemingly representative of those in the general population that may experience this condition. Other studies observed individuals with a body mass index greater than 30 kg/m2 had an odds ratio of 5.6 for plantar fasciitis compared with those with a body mass index less than 25 kg/m2 [5].
There are several limitations to this study including:
• small sample size (n=10);
• lack of control/sham group;
• variable activity preferences/amounts among subjects;
• study duration--true tissue changes may not be revealed within 3 weeks;
• Variable body mass index
A follow-up study addressing the above limitations and plantar fascia thickness and loss of function on a disability index is recommended. However, our short-term study does indicate that within a small sample of subjects with a wide variety of activity levels and lifestyles, Kinesio taping® does have a positive interaction on reducing plantar fascia thickness and pain.
In conclusion, the application of Kinesio taping® was easily learned and correctly performed by each subject, suggesting it could be applied by the general public. An overall decrease in pain and trend towards decrease in plantar fascia thickness was found, as noted by a comparison of the baseline, pre-intervention measures and those obtained following 3 weeks of Kinesio taping®. These findings seem to suggest that the use of Kinesio Taping® may be considered an effective, conservative, and practical intervention in the treatment of plantar fasciitis for short-term pain relief when used with the exercise protocol. However a larger sample sized study with a control group is needed to warrant these results.
Acknowledgement
Marie Davidson, ATC for her instruction on using the Kinesio taping®, and Richard Pine, SPT and Jonathan Belk, SPT for being part of the research team.
References
- Singh D, Angel J, Bentley G, Trevino SG (1997) Fortnightly review. Plantar fasciitis. BMJ 315: 172-175.
- The epidemiology of plantar fasciitis | Lower Extremity Review Magazine [Internet] 2010 Apr [cited 2015 Aug 19].
- Riddle DL, Schappert SM (2004) Volume of ambulatory care visits and patterns of care for patients diagnosed with plantar fasciitis: a national study of medical doctors. Foot Ankle Int 25: 303-310.
- Thomas JL, Christensen JC, Kravitz SR, Mendicino RW, Schuberth JM, et al. (2010) The diagnosis and treatment of heel pain: a clinical practice guideline-revision 2010. J Foot Ankle Surg 49: S1-19.
- Karabay N, Toros T, Hurel C (2007) Ultrasonographic evaluation in plantar fasciitis. J Foot Ankle Surg 46: 442-446.
- Mohseni-Bandpei MA, Nakhaee M, Mousavi ME, Shakourirad A, Safari MR, et al. (2014) Application of ultrasound in the assessment of plantar fascia in patients with plantar fasciitis: a systematic review. Ultrasound Med Biol 40: 1737-1754.
- Morris D, Jones D, Ryan H, Ryan CG (2013) The clinical effects of Kinesio® Tex taping: A systematic review. Physiother Theory Pract 29: 259-270.
-  Moore R (2012) What is the Current Evidence for the use of Kinesio Tape? a Literature Review. SportEX Dyn 24–30.
- Chen CK, Lew HL, Chu NC (2012) Ultrasound-guided diagnosis and treatment of plantar fasciitis. Am J Phys Med Rehabil 91: 182-184.
- Buchbinder R, Ptasznik R, Gordon J, Buchanan J, Prabaharan V, et al. (2002) Ultrasound-guided extracorporeal shock wave therapy for plantar fasciitis: a randomized controlled trial. JAMA 288: 1364-1372.
- McPoil TG, Martin RL, Cornwall MW, Wukich DK, Irrgang JJ, et al. (2008) Heel pain--plantar fasciitis: clinical practice guildelines linked to the international classification of function, disability, and health from the orthopaedic section of the American Physical Therapy Association. J Orthop Sports Phys Ther 38: A1–A18.
- Donley BG, Moore T, Sferra J, Gozdanovic J, Smith R (2007) The efficacy of oral nonsteroidal anti-inflammatory medication (NSAID) in the treatment of plantar fasciitis: a randomized, prospective, placebo-controlled study. Foot Ankle Int 28: 20-23.
- Martinoli C (2010) Musculoskeletal ultrasound: technical guidelines. Insights Imaging 1: 99-141.
- Williamson A, Hoggart B (2005) Pain: a review of three commonly used pain rating scales. J Clin Nurs 14: 798-804.
- Young B, Walker MJ, Strunce J, Boyles R (2004) A combined treatment approach emphasizing impairment-based manual physical therapy for plantar heel pain: a case series. J Orthop Sports Phys Ther 34: 725–733.
- Carcia CR, Martin RL, Drouin JM (2008) Validity of the Foot and Ankle Ability Measure in athletes with chronic ankle instability. J Athl Train 43: 179-183.
- Eechaute C, Vaes P, Duquet W (2008) The chronic ankle instability scale: clinimetric properties of a multidimensional, patient-assessed instrument. Phys Ther Sport Off J Assoc Chart Physiother Sports Med 9: 57–66.
- Martin RL, Irrgang JJ (2007) A survey of self-reported outcome instruments for the foot and ankle. J Orthop Sports Phys Ther 37: 72-84.
Citation: Lawson D, Hoffmeyer A, Pearsall A and Vallabhajosula S (2015) Kinesio® Tex Tape: Valuable Conservative Treatment for Plantar Fasciitis?. J Nov Physiother 5: 271. DOI: 10.4172/2165-7025.1000271
Copyright: © 2015 Lawson et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 14751
- [From(publication date): 10-2015 - Mar 31, 2025]
- Breakdown by view type
- HTML page views: 10127
- PDF downloads: 4624