Kidney Transplant
Received: 30-May-2022 / Manuscript No. troa-22-68222 / Editor assigned: 01-Jun-2022 / PreQC No. troa-22-68222 / Reviewed: 15-Jun-2022 / QC No. troa-22-68222 / Revised: 20-Jun-2022 / Manuscript No. troa-22-68222 / Accepted Date: 25-Jun-2022 / Published Date: 27-Jun-2022 DOI: 10.4172/troa.1000143
Abstract
Patients who get strong organ transfers are at higher gamble for creating disease, which is owing to ongoing safe concealment. Under 8 instances of metastatic RCC (mRCC) have been accounted for as of recently. The point of this article is to introduce the situation of a 77-year-old male with mRCC of the local kidney and examine treatment choices including designated treatment, which gives off an impression of being the treatment of decision, even in the time of immunotherapy.
Keywords
Metastasis; Clear cell renal cell carcinoma; Transplant; Kidney
Introduction
Thrombotic microangiopathy is a range of problems described by occlusive microvascular apoplexy, microangiopathic hemolytic pallor, thrombocytopenia, and possibly lethal end-organ harm. TMA in patients with disease is an uncommon however frequently destroying difficulty that might be straightforwardly connected with a fundamental threat, chemotherapeutic treatment or a different coincidental determination. Malignant growth related TMA is clinically vague from other TMA disorders. An unexpected diminishing in hemoglobin levels, intense kidney injury, uncontrolled hypertension, and thrombocytopenia might make clinicians aware of the chance of TMA. In patients with danger, kidney-restricted TMA is generally normal, especially with openness to hostile to vascular endothelial development factor agents. In drug-prompted TMA, the most widely recognized clinical introductions are gradually moderate kidney disappointment, new or deteriorating hypertension, and a tasteless urinary dregs [1], frequently without even a trace of a clinically evident cancer.
Case presentation
A 64-year-elderly person with a background marked by Kaposi sarcoma and perished benefactor kidney transplantation 4 years earlier was seen for a gradually moderate expansion in his serum creatinine (sCr) level. He had a background marked by constant kidney disappointment of obscure etiology and had gone through hemodialysis for quite a long time prior to getting the kidney relocate [2]. His previous clinical history included hypertension, dyslipidemia, and moderate aortic stenosis. His prescriptions included expanded discharge tacrolimus 5 mg day to day, mycophenolic corrosive 360 mg two times every day, prednisone at 5 mg day to day, acetylsalicylic corrosive at 81 mg day to day, bisoprolol 5 mg day to day, ramipril 10 mg day to day, and pravastatin 40 mg day to day. He was a long lasting nonsmoker, had negligible liquor consumption, and didn't utilize sporting medications.
A kidney allograft biopsy performed 10 months after transplantation due to allograft brokenness uncovered intense rounded putrefaction, mediocre glomeruli, and moderate ongoing vascular illness. One and a half years after transplantation, the patient created nonpainful, nonpruritic, blended, violaceous papules respectively on the average surfaces of his feet as well as macules on the dorsum of the left metatarsophalangeal joints. A skin biopsy uncovered Kaposi sarcoma. He was treated with PLD at 20 mg/m2 at regular intervals for a considerable length of time; clinical reduction was accomplished, with great medication resilience. At the hour of Kaposi sarcoma conclusion, tacrolimus was supplanted with sirolimus determined to further develop malignant growth control and the mycophenolic corrosive portion was diminished. The patient gave Kaposi sarcoma repeat 8 months after the fact, and hence, the PLD treatment was continued at the past portion and recurrence, with great clinical reaction.
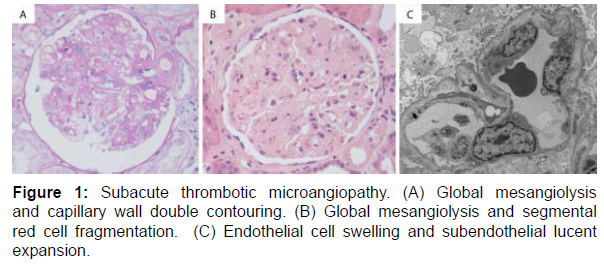
Two months after the determination of PLD-initiated, kidneyrestricted TMA, the patient was booked for a transcatheter aortic valve substitution for the treatment of his aortic stenosis [3]. Around then, sirolimus was changed to stretched out discharge tacrolimus to guarantee ideal careful injury mending after the technique. The patient's posttranscatheter aortic valve substitution course was muddled by pneumonia, cardiovascular breakdown, and intense or ongoing kidney injury (Figure 1). From there on, the sCr level got back to standard, and sirolimus was continued 3 months after the fact, without really any proof of TMA. Seven months after the suspension of PLD, the patient gave limited Kaposi sarcoma repeat. He got gemcitabine for a long time, with unfortunate resilience notwithstanding portion decreases, while his kidney capability stayed stable.
Description of constant kidney sickness
Is a significant wellbeing worry in this nation besetting in excess of 8,000,000 Americans. At the point when kidney capability declines to a specific level, patients have end-stage renal infection and require either dialysis or transplantation to support their life [4]. As of now in excess of 340,000 individuals are on dialysis, with 106,000 new patients added in 2006. More than 140,000 individuals are living with a working kidney relocate. The predominance of these two populaces of end-stage renal sickness has significantly increased over the most recent 20 years. Federal medical care use for end-stage renal sickness is supposed to surpass $28 billion out of 2010.
In 2006, 10,659 patients got a departed contributor kidney relocate and 6,432 patients got a live giver kidney relocate. Nonetheless, in excess of 74,000 individuals are at present on the public sitting tight rundown for a departed contributor kidney relocate. Notwithstanding the rising quantities of kidney transfers played out every year, the holding up list keeps on developing. Twelve individuals pass on every day anticipating a kidney relocate.
Medicines for end-stage renal disease
The medicines for end-stage renal illness are hemodialysis, a mechanical course of cleaning the blood of side-effects; peritoneal dialysis, in which byproducts are eliminated by going substance arrangements through the stomach depression; and kidney transplantation.
Notwithstanding, while none of these medicines fix end-stage renal sickness, a transfer offers the nearest thing to a typical life on the grounds that the relocated kidney can supplant the bombed kidneys. In any case, it likewise includes a long lasting reliance on medications to keep the new kidney sound. A portion of these medications can make serious side impacts.
Some kidney patients think about a transfer subsequent to starting dialysis; others think of it as prior to beginning dialysis. In certain conditions, dialysis patients who likewise have serious clinical issues, for example, disease or dynamic contaminations may not be reasonable contender for a kidney relocate.
Discussion
This case depicts a 64-year-elderly person with a distant history of kidney transplantation; Kaposi sarcoma in clinical reduction after 2 courses of PLD; and biopsy-demonstrated, kidney-restricted TMA credited to PLD.
Relocate related TMA might result from different gamble factors, including the utilization of calcineurin inhibitors or mammalian objective of rapamycin inhibitors, unite versus have sickness, past transplantations, human leukocyte antigen crisscross, and shrewd diseases. The normal pathogenetic pathway incorporates endothelial cell injury, potential supplement actuation, and end-organ harm [5].
Calcineurin inhibitors probably significantly affect the kidney allograft, prompting endothelial brokenness and expanded platelet total, perhaps through prostacyclin restraint. Patients with sirolimusinstigated TMA have essentially lower kidney VEGF articulation contrasted and those with typical relocated kidneys. The restraint of VEGF capability in glomerular endothelial cells seems, by all accounts, to be the reason for TMA. For this situation, an optional workup for TMA yielded adverse outcomes, with no dynamic contaminations, intense dismissal, connective tissue or immune system illnesses, openness to radiation, or openness to different poisons.
Results
TMA is a very much depicted entanglement of both disease and its treatment. Disease related TMA for the most part happens with regards to cutting edge or metastatic malignant growth, looking like thrombotic thrombocytopenic purpura, and is all the more usually found in mucin-delivering adenocarcinomas [6]. There are no revealed instances of TMA related with Kaposi sarcoma, and the patient's clinical reduction at the hour of TMA conclusion makes Kaposi sarcoma an improbable etiology.
The fleeting relationship between the utilization of PLD and demolishing kidney capability, improvement after PLD stopping in spite of proceeded with openness to sirolimus or tacrolimus, a high combined PLD portion, repetitive kidney brokenness when PLD was continued, and clinically unmistakable or advancing metastatic danger support the idea that PLD-prompted TMA was the likely etiologic variable. This is additionally upheld by utilization of the World Health Organization-Uppsala Monitoring Center System and the Naranjo causality evaluation scale in this case. A possible contributing job for the patient's immunosuppressive treatment and gemcitabine can't be precluded.
Conclusion
We depicted the principal instance of kidney-restricted TMA because of PLD in a kidney relocate patient. Kidney relocate patients are at expanded chance of threat, and it is vital to perceive PLD-related TMA as a substance that is habitually treacherous and restricted to the kidney. Patients getting PLD ought to be checked for new or demolishing hypertension, hematuria, proteinuria, and diminished kidney capability.
Acknowledgement
The authors are grateful to the Perth Children’s Hospital for providing the resources to do the research on transplantation.
Conflicts of Interest
The authors declared no potential conflicts of interest for the research, authorship, and/or publication of this article.
References
- Augustine J (2018) Kidney transplant: New opportunities and challenges. Cleve Clin J Med 85: 138-144.
- Voora S, Adey DB (2019) Management of kidney transplant recipients by general nephrologists: core curriculum 2019 Am J Kidney Dis 73: 866-879.
- Suarez MLG, Parker AS, Cheungpasitporn W (2020) Pregnancy in kidney transplant recipients. Adv Chronic Kidney Dis 27: 486-498.
- Capelli I, Aiello V, Gasperoni L, Comai G, Corradetti V, et al. (2020) Kidney transplant in fabry disease: a revision of the literature. Medicina 56: 284.
- Pinter J, Hanson CS, Chapman JR, Wong G, Craig JC, et al. (2017) Perspectives of older kidney transplant recipients on kidney transplantation. Clin J Am Soc Nephrol 12: 443-453.
- George JN, Nester CM (2014) Syndromes of Thrombotic Microangiopathy. N Engl J Med 371: 654-666.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Piana A, Urrego M, Cameron A (2022) Kidney Transplant. Transplant Rep 7: 143. DOI: 10.4172/troa.1000143
Copyright: © 2022 Piana A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 1602
- [From(publication date): 0-2022 - Nov 23, 2024]
- Breakdown by view type
- HTML page views: 1419
- PDF downloads: 183