Ischemic Cerebrovascular Accident as a Novel Presentation of CTLA-4 Haploinsufficiency, a Case Report
Received: 24-Aug-2022 / Manuscript No. JCB-22-72856 / Editor assigned: 26-Aug-2022 / PreQC No. JCB-22-72856 (PQ) / Reviewed: 09-Sep-2022 / QC No. JCB-22-72856 / Revised: 13-Jan-2023 / Manuscript No. JCB-22-72856 (R) / Published Date: 28-Jan-2023
Abstract
Background: Patients with CTLA-4 haploinsufficiency suffer from immune system dysregulation with symptoms of autoimmunity and immunodeficiency. Clinical presentation of CTLA-4 haploinsufficiency is described as recurrent infections due to immunodeficiency, as well as autoimmune related type 1 diabetes mellitus and neurologic complications. Neurologic manifestations of CTLA-4 haploinsufficiency included autoimmune encephalitis and demyelinating syndromes.
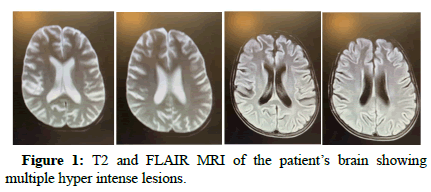
Case presentation: The patient was a 10 year old girl known case of CTLA-4 haploinsufficiency who presented with vertigo and impaired Romberg test. In her brain MRI, multiple hyper intense lesions in T2 and FLAIR were found. Her electroencephalogram also showed focal epileptic waves. She was treated with tacrolimus, prednisolone and levetiracetam which ended in the resolution of her symptoms.
Conclusion: Ischemic Cerebrovascular Accidents (CVA) and epilepsy might be the novel neurologic manifestations of CTLA-4 haploinsufficiency
Keywords: CTLA-4 haploinsufficiency; Pediatric CVA; Seizure; Autoimmune disease
Introduction
Inborn errors of immunity are referred to defects in immune system which are also associated with immune dysregulation which might cause autoimmunity and white blood cell proliferation, as in Cytotoxic T Lymphocyte associated Antigen-4 (CTLA-4) deficiency [1]. CTLA-4 is a surface protein of regulatory T cells, mostly involved in the process of immune response deactivation; therefore CTLA-4 deficiency would lead to autoimmunity and leukocyte over proliferation [2]. Lipopolysaccharide Responsive Beige like Anchor protein (LRBA) mutations are also associated with lower CTLA-4 expression on regulatory T-cells, thus ending in overstimulation of the immune system [3].
Patients with CTLA-4 haploinsufficiency suffer from immune system dysregulation, with symptoms of autoimmunity and immunodeficiency due to hypogammaglobulinemia [4]. Laboratory findings in CTLA-4 haploinsufficiency include: Decreased number of lymphoid lineage cells, such as B cells, T cells and NK cells, increased number of double negative T cells, decreased FOXP3 expression on regulatory T cells, increased CD21+B cells accompanied by splenomegaly, as well as hypogammaglobulinemia in IgA, IgM and IgG classes. T cell hyper activation can then lead to underproduction of other lineages, such as B cells and NK cells [5-7].
Clinical presentation of CTLA-4 haploinsufficiency is described as recurrent infections due to immunodeficiency, as well as autoimmune related type 1 diabetes mellitus, gastrointestinal involvement and neurologic complications. Neurologic manifestations of CTLA-4 haploinsufficiency included autoimmune encephalitis and demyelinating syndromes [8]. In this case report, we aimed to describe a new neurologic manifestation of CTLA-4 haploinsufficiency in a 10 year old girl.
Case Presentation
The patient was a 10 year old girl who presented with splenomegaly since two years prior to admission. She had a history of recurrent otitis media and chronic diarrhea. After primary workup, she had received 14 doses of IVIg due to hypogammaglobulinemia with suspected diagnosis of ALPS. However, since she had less than one percent CD4-/CD8-/α/β+ T cells in her flow cytometry study, the diagnosis of ALPS was questioned. Moreover, she had not responded to the treatment and the splenomegaly had not resolved; therefore, whole exome sequencing was done for her which showed CTLA-4 haploinsufficiency. In her last admission, she presented with sudden vertigo and exacerbation of her diarrhea. On her physical examination, she had impaired heel to shin test and impaired Romberg test; she also had cerebellar ataxia. Endoscopy, colonoscopy and brain MRI were done for the patient. The endoscopy and colonoscopy showed multiple ulcers in the colon and active colitis, as well as CMV ulcers in the esophagus with CMV IV. As can be seen in figure, brain MRI of the patient showed multiple T2 and FLAIR hyper intense lesions with diffuse restriction especially in the body of left lateral ventricle, most probably due to leukostasis in her brain (Figure 1). The patient also showed epileptic movements for which an electroencephalogram was taken from the patient. The EEG showed fast background activity and focal epileptic waves. In her course of hospitalization, the patient received prednisolone, tacrolimus and levetiracetam by which the symptoms resolved. The patient was discharged from the hospital but after two weeks returned back with fever and dyspnea. She was admitted and a diagnosis of COVID-19 was made for her. In her second course of hospitalization, she developed gastrointestinal bleeding and unfortunately expired due to her poor condition. Subsequently, long term follow up of the patient is not available (Table 1).
| Test | Result |
|---|---|
| WBC | |
| Neutrophil | 49.2% |
| Lymphocyte | 48.8% |
| Mixed cell | 2.0% |
| Hemoglobin | |
| RBC | |
| MCV | 86.3 |
| MCH | 27.5 |
| MCHC | 31.9 |
| Platelets | 1,29,000 |
| Reticulocytes | 1.60% |
| BUN | 10 |
| Creatinine | 0.55 |
| Sodium | 138 |
| Potassium | 3.7 |
| Calcium | 7.3 |
| Phosphorus | 2.4 |
| AST | 13 |
| ALT | 7 |
| Alkaline phosphatase | 117 |
| Serum protein | 4.3 |
| Albumin | 3.1 |
| Total bilirubin | 0.5 |
| Direct bilirubin | 0.2 |
| TSH | 2.7 |
| T4 | 155 |
| Hemoglobin electrophoresis | Normal |
| ANA | 0.3 (negative<1) |
| Anticardiolipin IgG | <0.01 (negative<12) |
| Anticardiolipin IgM | <0.01 (negative<12) |
| Lupus anticoagulant | 41.3 (NL: 28-45) |
| Anti ds-DNA | 3.7 (Negative<25) |
| Anti-TTG IgA | 0.11 (negative<12) |
| LDH | 164 (NL: 120-300) |
| Vitamin B12 | 852 (NL: 328-1130) |
| G6PD | Normal |
| C3 | 1.53 (NL: 0.9-1.8) |
| C4 | 0.35 (NL: 0.1-0.4) |
| EBV VCA | 6.5 (negative<20) |
| Pyruvate kinase M2 | 17 (NL: 7.4-23) |
| IGF-1 | 134 (NL: 30-900) |
| Morning cortisol | 18 |
| GH stimulation with clonidin | Base: 2.6 |
| 30 min: 5.3 | |
| 60 min: 3.6 | |
| 90 min: 3.0 | |
| ESR | |
| CRP | |
| DHR | |
| Direct coombs test | Negative |
| Indirect coombs test | Negative |
| Osmotic fragility test | |
| IgG level | 244 (NL: 700-1600) |
| IgM level | 27.0 (NL: 40-230) |
| IgA level | 7.8 (NL: 70-400) |
| IgE level | 93.5 (NL: 0-200) |
| CD3 (Total T cells) | 87% (NL: 56-84) |
| CD4 (helper T cells) | 21% (NL: 31-52) |
| CD8 (cytotoxic T cells) | 63% (NL: 18-35) |
| CD16 (NK cells) | 12% (NL: 3-22) |
| CD19 (B cells) | 1% (NL: 6-23) |
| CD45 (gated leukocytes) | 93% |
| CD56 (NK cells) | 12% (NL: 3-22) |
| CD4/CD8 | 0.3 (NL: 1.1-1.4) |
| CD11b (adhesion molecule) | Normal |
| IFN-gamma receptor | Normal |
| CD14 (monocyte) | 7% (NL: 4.4-8) |
| HTLV 1 and 2 | 0.34 (Negative<1.0) |
Table 1: Lab data of the patient.
Discussion
In this case report, we aimed to describe a new neurologic manifestation of CTLA-4 haploinsufficiency. In our case, CTLA-4 haploinsufficiency presented with ischemic infarction of the cerebellum and focal epileptic activities. The infarction resolved after a few days with treatment of CTLA-4 with corticosteroid (prednisolone) and a calcineurin inhibitor (tacrolimus), without any antiplatelet or thrombolytic agent. The seizures were also resolved with levetiracetam.
Previously, the neurologic complications of CTLA-4 haploinsufficiency included autoimmune encephalitis and demyelinating syndromes [8].
In a case series by Ayrignac they described three patients with neurologic manifestations of CTLA-4 haploinsufficiency. One of the patients had recurrent severe headaches, with lower limb weakness and partial seizures. The patient’s brain MRI revealed multiple cortical and subcortical lesions which were hyper intense in FLAIR views and was enhanced with gadolinium contrast. The other patient had transient hemianopsia and headache that had infiltrative lesions in her occipital lobe which were enhanced with gadolinium contrast. The other patient had urinary urgency and axonal optic neuropathy with abnormal gait. She had bilateral diffuse leukoencephalopathy in her brain MRI [9].
The underlying causes of the neurologic manifestations of CTLA-4 might be autoimmune in nature, such as autoimmune encephalitis, or be due to lymph proliferation and leukostasis in CNS vessels. The patients in the study performed by Ayrignac showed both of the pathophysiologic pathways. In our case, the patient most probably showed this problem due to leukostasis since the lumbar puncture profile of the patient was normal. Moreover, she responded to treatment of CTLA-4 haploinsufficiency. Although the main treatment of CTLA-4 haploinsufficiency in Abatacept, since this pharmaceutical agent was unavailable in Iran, we decided to treat the patient with corticosteroids and calcineurin inhibitors.
The documents concerning the neurologic manifestations of CTLA-4 haploinsufficiency are very limited in number; however, multiple documents have described the neurologic complications of target therapy agents against CTLA-4 pathway in antineoplastic treatments. The treatment with Ipilimumab, a CTLA-4 blocking agent, has shown multiple immune mediated neurologic adverse effects, such as sensory and motor polyneuropathy, aseptic meningitis, enteric neuropathy, Guillain-Barre syndrome, posterior reversible encephalopathy syndrome and myasthenia gravis like symptoms and hypophysitis [10,11]. Such complications might be seen in patients with CTLA-4 deficiency, especially in homozygote forms. Brain edema, temporal arteritis, chronic inflammatory demyelinating polyneuropathy, and transverse myelitis have also been associated with anti-CTLA-4 treatments [12-14].
Conclusion
Patients with CTLA-4 haploinsufficiency might have various neurologic symptoms, such as autoimmune encephalitis, and demyelinating syndrome due to immune system dysregulation. However, since this disease can cause lymph proliferation, leukostasis can occur in various parts of the blood circulation of the central nervous system. In our patient, cerebellar infarction due to leukostasis occurred which was resolved by the proper treatment of CTLA-4 haploinsufficiency.
Acknowledgement
The authors would like to thank the patient’s parents for their cooperation with our team.
Conflict of Interest
The authors declare no conflicts of interest.
Consent Disclosure
The patient’s parents consented to have their daughter’s medical record publish if she remains anonymous.
References
- Sun D, Heimall J (2019) Disorders of CTLA-4 expression, how they lead to COVID and dysregulated immune responses. Curr Opin Allergy Clin Immunol 19: 578-585.
[Crossref] [Google Scholar] [PubMed]
- Takahashi T, Tagami T, Yamazaki S, Uede T, Shimizu J, et al. (2000) Immunologic self-tolerance maintained by CD25(+) CD4(+) regulatory T cells constitutively expressing cytotoxic T lymphocyte associated antigen 4. J Exp Med 192: 303-310.
- Lo B, Zhang K, Lu W, Zheng L, Zhang Q (2015) Patients with LRBA deficiency show CTLA4 loss and immune dysregulation responsive to abatacept therapy. Science 349: 436-440.
[Crossref] [Google Scholar] [PubMed]
- Schwab C, Gabrysch A, Olbrich P, Patiño V, Warnatz K (2018) Phenotype, penetrance, and treatment of 133 cytotoxic T-lymphocyte antigen 4-insufficient subjects. J Allergy Clin Immunol 142: 1932-1946.
[Crossref] [Google Scholar] [PubMed]
- Waterhouse P, Penninger JM, Timms E, Wakeham A, Shahinian A (1995) Lymphoproliferative disorders with early lethality in mice deficient in Ctla-4. Science 270: 985-988.
[Crossref] [Google Scholar] [PubMed]
- Schubert D, Bode C, Kenefeck R, Hou TZ, Wing JB (2014) Autosomal dominant immune dysregulation syndrome in humans with CTLA4 mutations. Nat Med 20: 1410-1416.
[Crossref] [Google Scholar] [PubMed]
- Kuehn HS, Ouyang W, Lo B, Deenick EK, Niemela JE (2014) Immune dysregulation in human subjects with heterozygous germline mutations in CTLA4. Science 345: 1623-1627.
[Crossref] [Google Scholar] [PubMed]
- Lougaris V, Tabellini G, Baronio M, Patrizi O, Gazzurelli L (2018) CTLA-4 regulates human natural killer cell effector functions. Clin Immunol 194: 43-45.
[Crossref] [Google Scholar] [PubMed]
- Ayrignac X, Goulabchand R, Jeziorski E, Rullier P, Carra-Dallière C (2020) Two neurologic facets of CTLA4 related haploinsufficiency. Neurol Neuroimmunol Neuroinflamm 7: e751.
[Crossref] [Google Scholar] [PubMed]
- Tarhini A (2013) Immune mediated adverse events associated with ipilimumab ctla-4 blockade therapy: The underlying mechanisms and clinical management. Scientifica (Cairo) 2013: 857519.
[Crossref] [Google Scholar] [PubMed]
- Astaras C, de Micheli R, Moura B, Hundsberger T, Hottinger AF (2018) Neurological adverse events associated with immune checkpoint inhibitors: Diagnosis and management. Curr Neurol Neurosci Rep 18: 3.
[Crossref] [Google Scholar] [PubMed]
- O'Day SJ, Maio M, Chiarion-Sileni V, Gajewski TF, Pehamberger H (2010) Efficacy and safety of ipilimumab monotherapy in patients with pretreated advanced melanoma: A multicenter single arm phase II study. Ann Oncol 21: 1712-1717.
[Crossref] [Google Scholar] [PubMed]
- Weber JS, Amin A, Minor D, Siegel J, Berman D, et al. (2011) Safety and clinical activity of ipilimumab in melanoma patients with brain metastases: Retrospective analysis of data from a phase 2 trial. Melanoma Res 21: 530-534.
[Crossref] [Google Scholar] [PubMed]
- Liao B, Shroff S, Kamiya-Matsuoka C, Tummala S (2014) Atypical neurological complications of ipilimumab therapy in patients with metastatic melanoma. Neuro Oncol 16: 589-593.
[Crossref] [Google Scholar] [PubMed]
Citation: Nabavizadeh SH, Esmaeilzadeh H, Alyasin S, Askarisarvestani A (2023) Ischemic Cerebrovascular Accident as a Novel Presentation of CTLA-4 Haploinsufficiency, a Case Report. J Cytokine Biol 8: 434.
Copyright: © 2023 Nabavizadeh SH, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 3130
- [From(publication date): 0-2023 - Dec 19, 2025]
- Breakdown by view type
- HTML page views: 2685
- PDF downloads: 445