Invasive Rhino-Orbital-Cerebral Mucormycosis in Sinonasal Neuroendocrine Carcinoma: A Case Report
Received: 18-Oct-2021 / Accepted Date: 01-Nov-2021 / Published Date: 08-Nov-2021
Abstract
Mucormycosis is an invasive infection due to Mucorale species with an acute onset and have potential to be life-threatening. Though a relatively uncommon fungal infection in comparison with candidiasis and aspergillosis, mucormycosis cases have been on the rise over the past decade possibly due to the increased use of chemotherapy, steroids and other immunosuppressants which is associated with prolonged immunocompromised state. Neuroendocrine carcinoma is a rare malignancy of specialised cells called neuroendocrine cells having both hormones producing as well as nerve cells which can occur anywhere in the body. Surgical intervention and debridement is the gold standard of treatment for eradicating the infection along with antifungal treatment with Liposomal Amphotericin B formulations and Posaconazole. We report a case of a diabetic woman with sinonasal neuroendocrine cancer who developed mucormycosis recovered with appropriate intravenous antifungal therapy.
Keywords: Mucormycosis; Neuroendocrine carcinoma; Amphotericin B; Chemotherapy
Introduction
Mucormycosis (previously called as Zygomycosis or phycomycosis) is an invasive infection caused by the widespread saprophytic organisms called Mucorale which has a potential to become life threatening. It was first described as Mycosis mucorina by Arnold Paltauf in 1885 [1]. It causes acute angioinvasive infection seen primarily in the immunocompromised individuals with seven genera within Mucorales namely Rhizopus, Mucor, Absidia, Saksenaea, Rhizomucor, Apophysomyces, and Cunninghamella documented as pathogenic, with the most common causative organism being Rhizopus species [2]. The primary route of infection is by inhalation of asexual spores of Mucorales called sporangiospores, leading to invasive sinopulmonary infection in susceptible individuals with other occasional causes being ingestion of contaminated food or traumatic inoculation. From there, Central Nervous System (CNS) penetration occurs either by hematogenous spread or by direct cranial penetration from the paranasal sinuses [3,4]. The definitive diagnosis depends on microbiological analyses of tissue obtained by biopsy or surgical debridement along with imaging with Computed Tomography (CT) or Magnetic Resonance Imaging (MRI) scans to assess for sinus involvement or spread to contiguous structures. Successful treatment of mucormycosis requires surgical debridement of infected tissue, prompt institution of antifungal treatment, and correction of the underlying metabolic and immune derangement [4].
Case Presentation
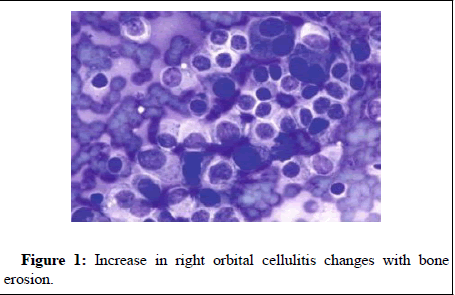
A 45 year old female was admitted with complaints of pain in the throat, backside and abdomen along with fever on day 10 post chemotherapy. She was a known diabetic whose persisting nasal block, bleed was diagnosed with immunohistochemistry of excised mass from septoplasty with Functional Endoscopic Sinus Surgery (FESS) to be positive for malignancy with histology favouring sinonasal neuroendocrine tumour (ki67 92%). She started chemotherapy with Etoposide (100 mg/m2) and Cisplatin (25 mg/m2) with Granulocyte Colony Stimulating Factor (GCSF) injection. On Day 10 post chemotherapy she was found to be neutropenic along with body ache and fever. Hence she was started on G CSF along with prophylactic antibiotics as well as antifungal prophylaxis. The blood and urine cultures were found to be sterile but G CSF had to be continued due to persistent neutropenia. Serum Galactomannan was found to be 2.35 while HRCT lungs taken did not suggest any abnormality besides possible atelectatic changes but antifungal prophylaxis was escalated to Voriconazole. On day 18 post chemotherapy she developed pain in the right eye with periorbital swelling, difficulty opening eyelid along with headache. Suspecting Multiple cranial nerve palsy [3,5,6] or Tolosa hunt syndrome probably infiltration, neurologist initiated her with IV Methylprednisolone 125 mg twice daily but the MRI of brain showed mucosal edema in right paranasal sinus and inflammatory changes in right orbit most likely to be infection hence Methyl Prednisolone was stopped and she was started on ophthalmic steroids, ophthalmic antibiotic and eye lubricants. Nasopharyngoscopy was taken on day 20 post chemotherapy which suggested colonising fungal activity in the right nasal cavity thus requiring escalation to IV Posaconazole. On Day 28 post chemotherapy, the MRI of brain and Peripheral Nervous System (PNS) taken to assess treatment progress demonstrated significant increase in right orbital cellulitis changes with bone erosion, poor enhancement and intracranial extension likely to be fungal sinusitis, right basifrontal leptomeningitis with small infarct requiring an emergency FESS with orbital exenteration of right eye (Figure 1). The histopathology confirmed invasive mucormycosis thus initiating IV liposomal Amphotericin B 250 mg (4 mg/kg) once daily. On day 3 of Amphotericin B she developed generalized maculopapular rash with pruritus and hypokalemia (2.8 mEq/L) for which she was given antihistamine and topical moisturizers along with supplementation with intravenous as well as oral potassium till the end of treatment with Amphotericin B for a total course of 14 days after which she was restarted with IV Posaconazole.
Discussion
Mucormycosis commonly presents in five forms based on the area affected namely pulmonary, rhinocerebral, gastrointestinal, cutaneous, or the central nervous systems. The fungi penetrates the organs through orbital, oral, nasal, or skin pathways and produce granulomatous, thrombotic and necrotic lesions, while the hyphae penetrate all normal structures [4]. Our case involves infection in the sinonasal area which extended towards the right eye classifying it broadly into rhinocerebral mucormycosis. Invasive mucormycosis in oncologic patients is usually seen in hematological malignancies, and is not that common in patients with solid tumors. Roden et al. in a study of 929 mucormycosis cases, state that only 7 out of 154 patients with malignancy related mucormycosis had Non-Hematological Malignancy (NHM) [5]. The common causes for mucormycosis include diabetes mellitus with or without diabetic ketoacidosis, malignancies (haematological and solid organ tumor), transplant recipients, corticosteroid therapy and neutropenia. In the Asian continent diabetes mellitus is the most common risk factor whereas haematological malignancies and transplantation are the major risk factors in European countries and the United States. Our case is of a diabetic patient with good glycemic control who had an unusually prolonged neutropenia period post chemotherapy for a non hematological malignancy. Immunosuppressive therapy and high steroid dose in patients also make the patient susceptible to mucormycosis as corticosteroid impairs the macrophage and neutrophil function. The patient was also given steroids due to suspicion of neurological disorder which was then stopped [6]. The patients with diabetes mellitus usually develop Rhino-Orbital-Cerebral Mucormycosis (ROCM) while patients with hematological neoplasms generally develop sino-pulmonary disease and trauma patients develop necrotizing skin and soft tissue infections. High residual morbidity and mortality is associated with Rhinocerebral Mucormycosis due to the angioinvasive nature of the fungus due to vascular occlusion and extensive tissue necrosis. Initial symptoms are usually those of a sinusitis preseptal or orbital cellulitis. Surgical intervention and debridement is the gold standard of treatment for eradicating the infection, and was associated with improved survival in several case series. In patients with rhino-orbital-cerebral mucormycosis (ROCM), sinus surgery is regarded as essential but extensive surgical debridement is difficult to achieve because important structures are often adjacent to necrotic tissues, particularly in sinonasal, rhinoorbital, and, especially, cerebral involvement. Our patient had undergone an emergency FESS with orbital exenteration of the right eye [4].
Amphotericin B is considered the treatment of choice for mucormycosis with preference for its liposomal formulation since significant toxicity was associated with the high doses of Amphotericin B deoxycholate (AmBd) needed to attain fungicidal effect against Mucorales species [4]. Patients who respond to initial therapy with l-AmB may be switched to maintenance treatment with less toxic azoles like Posaconazole or Isavuconazole which may increase the likelihood of achieving effective drug concentrations in the brain. The optimal duration of treatment for CNS mucormycosis is unknown and must be weighed based on the extent of surgical debridement performed and the immune state of the patient as well as the affordability of the patient given the expense of antifungal treatment. European guidelines suggests to “continue treatment until complete response (on imaging) and permanent reversal of immunosuppression are achieved” but no prospective studies have been performed [2,7]. Amphotericin B crosses the blood-brain barrier poorly while concentrations of Posaconazole are highly variable in treated patients [4]. Our patient was started on Liposomal Amphotericin B upon report of mucormycosis for a course of 14 days which was then de-escalated to Posaconazole.
A recent meta-analysis had 92 cases of mucormycosis in patients with prior antifungal prophylaxis with Voriconazole (52%), Fluconazole (25%), Itraconazole (7.6%), Posaconazole (5%) and Caspofungin (9.8%). An increase in frequency of mucormycosis cases after treatment with Voriconazole prophylaxis in HSCT patients was reported by Marty et al in 2016. Our case also had prophylactic therapy with Voriconazole prior to confirmation of mucormycosis from biopsy of the excised area [6].
Conclusion
Mucormycosis is not only a disease of the immunocompromised host since a considerable number of cases are also seen in an immunocompetent host without any known underlying illness The overall rarity of this disease, and its often-rapid progression and severity impede treatment of the condition while the heterogeneity of clinical presentation, underlying comorbidities and treatments complicate data interpretation. Due to the increase in cases of breakthrough mucormycosis after general antifungal prophylaxis and the overall increase in cases in the population, anti-Mucorales prophylaxis studies should be given due importance, alongside the search for methods of faster diagnosis and treatment.
References
- Athanasiadou KI, Athanasiadis DI, Constantinidis J, Anastasiou A, Roilides E, et al. (2019) Successful treatment of rhinoorbital mucormycosis due to Rhizopus arrhizus with liposomal amphotericin B, posaconazole and surgical debridement in a child with neuroblastoma. Med Mycol Case Rep 25: 10-14.
- Soni A, Gupta AK (2020) Sinonasal mucormycosis in a tertiary care center: A review of 30 cases. International Journal of Head and Neck Surgery 11: 55-57.
- Pak J, Tucci VT, Vincent AL, Sandin RL, Greene JN (2008) Mucormycosis in immunochallenged patients. J Emerg Trauma Shock 1: 106-113.
- Chikley A, Ben-Ami R, Kontoyiannis DP (2019) Mucormycosis of the central nervous system. J Fungi 5: 59.
- Roden MM, Zaoutis TE, Buchanan WL, Knudsen TA, Sarkisova TA, et al. (2005) Epidemiology and outcome of zygomycosis: A review of 929 reported cases. Clin Infect Dis 41: 634-653.
- Prakash H, Chakrabarti A (2019) Review global epidemiology of mucormycosis. J Fungi 5: 26.
- Cornely O, Arikanâ€Akdagli SE, Dannaoui E, Groll AH, Lagrou K, et al. (2014) ESCMID and ECMM joint clinical guidelines for the diagnosis and management of mucormycosis 2013. Clin Microbiol Infect 20: 5-26.
Citation: Philip SM (2021) Invasive Rhino-Orbital-Cerebral Mucormycosis in Sinonasal Neuroendocrine Carcinoma: A Case Report. J Alzheimers Dis Parkinsonism S7:027.
Copyright: © 2021 Philip SM. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 2140
- [From(publication date): 0-2021 - Nov 26, 2025]
- Breakdown by view type
- HTML page views: 1547
- PDF downloads: 593