Case Report Open Access
Invasive Micro Papillary Carcinoma of the Sigmoid Colon: Distinct Entity
Junainah EM1* and Alghamdi AR21Department of Pathology, Taief University, Kingdom of Saudi Arabia
2Department of Community Medicine, Taief University, Kingdom of Saudi Arabia
- *Corresponding Author:
- Enaam Mohammed Junainah
Department of Pathology
Taief University, Kingdom of Saudi Arabia
Tel: 00966544442556
E-mail: mennastar3@hotmail.com
Received Date: June 16, 2016; Accepted Date: July 11, 2016; Published Date: July 13, 2016
Citation: Junainah EM, Alghamdi AR (2016) Invasive Micro Papillary Carcinoma of the Sigmoid Colon: Distinct Entity. J Clin Exp Pathol 6:285. doi: 10.4172/2161-0681.1000285
Copyright: © 2016 Junainah EM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Clinical & Experimental Pathology
Abstract
Micro papillary carcinoma (MC) has been recently recognized as a rare distinctive variant of adenocarcinoma. It is considered as an aggressive variant with a high incidence of lymph node metastasis, only few cases of colorectal MC have been reported. Recently it has been officially recognized in WHO classification We present a case of MC of the sigmoid colon with extensive lymph node metastasis. A 61-year-old female patient was admitted with a complaint of acute abdomen diagnosed as MC of the sigmoid colon. The patient underwent Left hemi colectomy with lymph node dissection.
Keywords
Invasive micro papillary carcinoma of the colon; Aggressive
Introduction
Invasive micro papillary carcinoma (IMPC) has been recently recognized by WHO as a rare distinctive and aggressive variant of adenocarcinoma. With high incidence of lymph node and distant metastasis, it was first described in breast, but recently been reported in other organs such as lungs, urinary bladder, ovaries or salivary glands. It carries worse Prognosis than conventional colorectal carcinoma [1]. Pathologically it is characterized by mall clusters of malignant cells with abundant eosinophilic cytoplasm and pleomorphic nuclei, micropapillae inhabit lacunar-like spaces and demonstrate a "reverse polarity" configuration, with apical surfaces facing the periphery rather than the center. However, vigorous immunohistochemical staining for endothelial or lymphatic markers has been negative [1-3]. In most cases, it usually accompanied by variable component of conventional and mucinous carcinoma. Patients with IMPC usually present with higher-stage disease while here we report a case of IMPC of the sigmoid colon with immunohistochemical studies.
Case Report
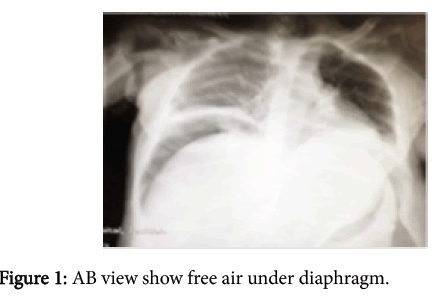
61-year-old Saudi female patient known to have diabetes, hypertension on treatment. Presented to ER with a history of abdominal pain and distension constipation for ten days duration. Three days prior to the admission she developed obstipation. On the day of admission her symptoms get worst and started to be anuric for 24 hours and she got chest pain. She gave a history of significant weight loss and appetite during last 2 years. Five months ago she sought medical advice at private hospital, stool analysis showed occult blood, colonoscopy done and it revealed sigmoid mass, and she was advised for surgery. On examination patient looks very ill, dehydrated, the abdomen distended, tense, guard, bowelsound absent. Her investigation show CBC: WBC 6, HB: 11.3, Chemistry: urea 64 Creatinine 2 ABG: showed metabolic acidosis. X-ray abd: free air under diaphragm (Figure 1). The patient started to reinstated with IVF, correct acidosis, foly’s catheter inserted, no urine output, nephro consultation done and cardiology assessment pre-operative done. The patient started on antibiotics Tazocine and Flagyl. The patient pushed for urgent laparotomy. Intra operative found gush of pussy fluid come out contaminated with large bowel contents and fibrinous and haemorrhagic adhesion between small bowel loop and urinary bladder, uterus and adnexal structure. Fibrinous tissue completely covering the liver and the spleen, intra looplar abscess. Primary resection was done with heartman pouch procedure done. Post-operative the patient was admitted to ICU, keep her on ventilator and supportive measure. On the third day she got leak at site of colostomy where push again to OR for revision of colostomy. After that she was kept in ICU her general condition mildly improved with drop in white blood cells, but still she was on sepsis. Drain was brought serous fluid. Ultrasound was done twice post-operative, proved no intra-abdominal collection so drain removed. We found perforation at recto sigmoid junction proximal to constructing lesion at this area. She passed away due to sever sepsis and advanced tumour.
Pathological and Immunohistochemical Finding
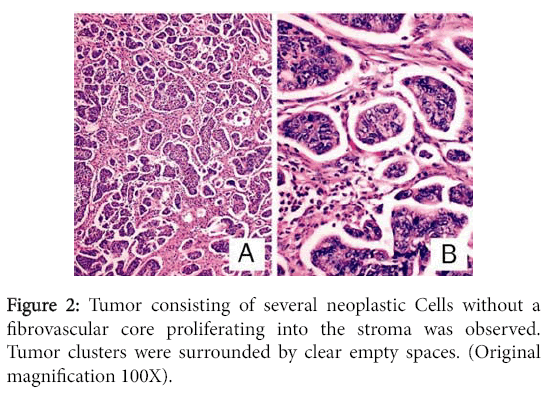
Macroscopic examination show hemicolectomy composed of part of sigmoid and rectum. Sigmoid colon measures 19 × 5 × 3 cm. On opening showing fungating necrotic mass that measure about 9 × 3 cm. The tumor is shown grossly infiltrated into muscle and fat. Microscopically characterized by Small clusters of malignant cells with abundant eosinophilic cytoplasm and pleomorphic nuclei Micro papillae inhabit lacunar-like spaces and demonstrate a "reversepolarity" configuration, with apical surfaces facing the periphery rather than the center (Figure 2).
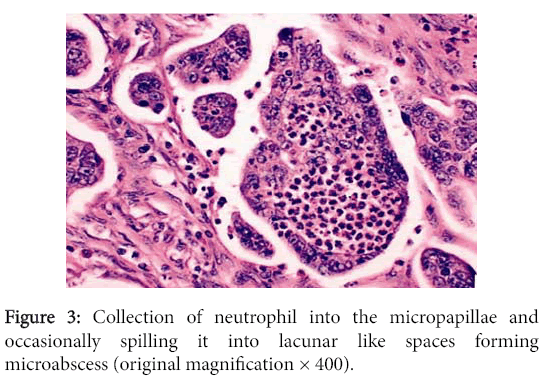
No fibrovascular core in the micropapillae (Figure 3). Furthermore, abundant neutrophils were frequently found mainly within and occasionally surrounding the micropapillae, forming microabscess but not “dirty necrosis” which is typically associated with conventional colorectal carcinoma, giving comedonecrosis like area that is seen mainly in breast. DCIS Mucinous area about 10% was noted.
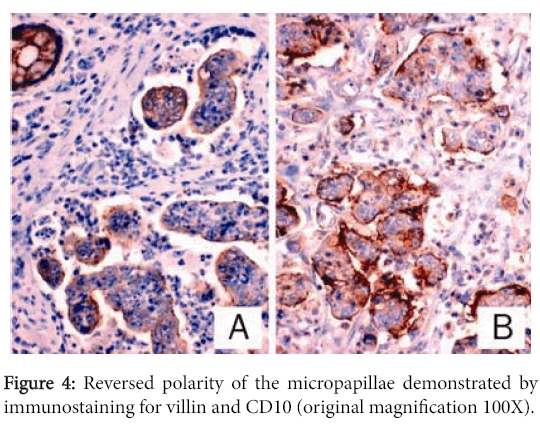
46 positive lymph nodes are identified. Some of which show extracapsular extension. The apical lymph node are 7 positive lymph node, Interestingly, Immunohisto-chemically, as in conventional colorectal carcinoma, the tumor cells were positive for, CK20, monoclonal CDX2, CD10, and villin; (Figure 4) and negative for CK7. Although, reversed polarity was demonstrated by positive CD10 and villin immunostaining on the stroma-facing surfaces of the micro papillae. Furthermore, endothelial marker (CD31) was negative in the tumor cluster at the lacunar space, but positive in true lympho vascular invasion.
Discussion
MPC has been first described in breast later on it has been recognized in urinary bladder, lung, and salivary gland tissues [4,5-7]. Recently approximately 265 cases of colon cancer with IMPC have been reported. It accounts for about 9%-19% of all colon cancers, most common in males aged 53-72 with 3/1 male to female predominance. Clinical symptoms in those are not specific and mainly include abdominal pain, anemia, vomiting, diarrhoea, constipation and bleeding from the rectum [8-13]. These tumours usually have exophytic growth with a centrally ulcerating crater [14]. Microscopically it shows neoplastic cells form small tight clusters surrounded by clear spaces which devoid of fibrovascular cores. IMPC of the colon is aggressive tumour usually high lymph node metastasis and high local recurrence, [13]. All IMPCs have a typical growth pattern with reversed polarity where the stromal-facing (basal) surface of the tumour demonstrated by MUC1, CD10 and villin, although other immunostains are still maintained, which is helpful to determine the primary of metastatic IMPC [14]. (Positive CK20, CDX2, and villin; negative CK7) the lacunar-like spaces were negative for endothelial marker CD31. Electron microscopic examination revealing microvilli at the surface of the cells facing stroma [2]. Our case uniquely showed abundant neutrophils within and around micropapillae. We believe that this is analogous to “dirty necrosis” characteristically associated with colorectal carcinoma. However, in the micropapillae the neutrophilic infiltrate manifested more like microabscesses rather than “dirty necrosis”.
Conclusion
Our case is among the first reported cases of invasive micropapillary carcinoma of the colorectal adenocarcinoma in the literature. It is a rare but distinct variant of adenocarcinoma that shares histologic and immunohistochemical features of IMPC in other sites.
Acknowledgement
Almamlka Lab, ksa for their support.
References
- Sirianunkgul S, Tavassoli FA (1993) Invasive micropapillary carcinoma of the breast. Mod Pathol 6: 660-662.
- Luna-More S, Gonzalez B, Acedo C, Rodrigo I, Luna C(1994) Invasive micropapillary carcinoma of the breast. A new special type of invasive mammary carcinoma. Pathol Res Pract 190: 668-674.
- Ro JY, el-Sharkawy T, Lee KM, Troncoso P, Silva EG, et al. (1994) Micropapillary variant of transitional cell carcinoma of the urinary bladder. Histologic pattern resembling ovarian papillary serous carcinoma. Am J SurgPathol 18: 1224-1232.
- Tamboli P, Merchant SH, Ordonez NG, Ro J, Ayala AG, et al. (2002) Micropapillary component in lung adenocarcinoma: a distinctive histologic feature with possible prognostic significance. Am J SurgPathol 26: 358-364.
- Gaffey TA, Visscher D, Kay P A, Minato H, Serizawa H, et al. (2004) Invasive papillary salivary duct carcinoma: a distinct variant with biologic significance. Am J SurgPathol 28: 319-326.
- Pansare V, Zhang H, Che M, Sakr W, Ali- Fehmi R, et al. (2004) Pathogenesis of invasive micropapillary carcinoma: role of MUC1 glycoprotein. Mod Pathol 17: 1045-1050.
- Nassar H (2004) Carcinomas with micropapillary morphology: clinical significance and current concepts. AdvAnatPathol 11: 297-303.
- Sakamoto K, Watanabe M, De La Cruz C, Honda H, Ise H, et al. (2005) Primary invasive micropapillary carcinoma of the colon. Histopathology 47: 479-484.
- Walsh MM, Bleiweiss IJ (2001) Invasive micropapillary carcinoma of the breast: eighty cases of an under-recognized entity. Hum Pathol 32: 583-589.
- Middleton LP, Tressera F, Sobel ME, Bryant BR, Alburquerque A, et al. (1999) Infiltrating micropapillary carcinoma of the breast. Mod Pathol 12: 499-504.
- Zekioglu O, Erhan Y, Ciris M, Bayramoglu H, Ozdemir N (2004) Invasive micropapillary carcinoma of the breast: high incidence of lymph node metastasis with extension and its immunohistochemical profile compared with invasive ductal carcinoma. Histopathology 44:18-23.
- Nagi C, Guttman M, Jaffer S, Qiao R, Keren R, et al. (2005) N-cadherin expression in breast cancer: correlation with an aggressive histologic variant—invasive micropapillary carcinoma. Breast Cancer Res Treat 94: 225-235.
- Paterakos M, Watkin WG, Edgerton SM, Moore DH, Thore AD (1999) Invasive micropapillary carcinoma of the breast: a prognostic study. Hum Pathol 30: 1559-1463.
- Tresserra F, Grases PJ, Fabregas R, Fernandez-Cid A, Dexeus S (1999) Invasive micropapillarycarcinoma.Distinct features of a poorly recognized variant of breast carcinoma. Eur J GynaecolOncol 20: 205-208.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 11706
- [From(publication date):
specialissue-2016 - Dec 21, 2024] - Breakdown by view type
- HTML page views : 11002
- PDF downloads : 704