Case Report Open Access
Intussusception due to Inflammatory Fibroid Polyp Located at Ileum
Paudyal P1*, Agarwal M1, Karki S1, Pradhan A1, Upadhyaya P1 and Agrawal CS2
1Department of Pathology, B P Koirala Institute of Health Sciences, Dharan, Nepal
2Department of Surgery, B P Koirala Institute of Health Sciences, Dharan, Nepal
- *Corresponding Author:
- Dr. Punam Paudyal
Associate Professor, Department of Pathology
B P Koirala Institute of Health Sciences, Dharan, Nepal
Tel: 977-9842040269
Email: drpunamsapkota@hotmail.com
Received date: February 07, 2014; Accepted date: September 23, 2014; Published date: September 25, 2014
Citation: Paudyal P, Agarwal M, Karki S, Pradhan A, Upadhyaya P et al. (2014) Intussusception due to Inflammatory Fibroid Polyp Located at Ileum. J Clin Exp Pathol 4:193. doi:10.4172/2161-0681.1000193
Copyright: 2014 Paudyal P, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Clinical & Experimental Pathology
Abstract
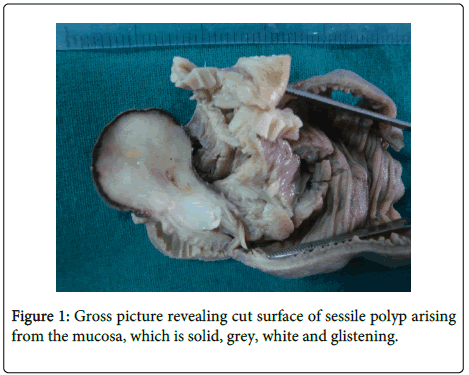
Majority of adult intussusceptions have a well-defined pathological abnormality as the definite cause. We report a case of 27 year old woman presented with vomiting and abdominal pain. We received a polypoidal; dumbbell shaped mass measuring 4×3.5×1 cm arising from the mucosal surface at one end of the small bowel. Outer surface of the polyp was grey to blackish and cut surface was solid, grey, white and glistening with few myxoid areas. Histopathologic examination revealed it to be an inflammatory fibroid polyp. The definite cause for intussusception in this case was a rare non-neoplastic submucosal lesion that is inflammatory fibroid polyp infrequently found in the ileum.
Keywords
Inflammatory fibroid polyp; Ileo-ileal intussusception
Introduction
Inflammatory fibroid polyp (IFP) is a rare, localized non neoplastic condition, originating in the submucosa of the gastrointestinal tract (GIT). It is most commonly found in the stomach, followed by small bowel, where it usually presents as intussusception or obstruction in adults [1].
The term inflammatory fibroid polyp was first proposed by Ranier and Helwig in 1953 [2]. These polyps are composed of fibrous connective tissue, blood vessels and an inflammatory cell infiltrate usually with many eosinophils [3].
Approximately 95% of all intussusception occur in children. Adult intussusception represents 5% of all cases of intussusception and accounts for only 1-5% of intestinal obstructions in adults [4]. In children, it is usually primary and benign, and pneumatic or hydrostatic, reduction of the intussusception is sufficient to treat the condition in 80% of the patients. However, almost 90% of the cases of intussusception in adults are secondary to a pathologic condition that serves as a lead point, which are usually discovered intraoperatively [5-6].
Intussusception represents a rare form of bowel obstruction in the adult, which is defined as the telescoping of a proximal segment of the gastrointestinal (GI) tract, called intussusceptum, into the lumen of the adjacent distal segment of the GI tract, called intussuscipiens. Historically, Sir Jonathan Hutchinson was the first to operate on a child with intussusception in 1871 [7].
Intussusceptions have also been classified according to etiology that is benign, malignant or idiopathic. In the small intestine, an intussusception can be secondary either to the presence of intra or extra luminal lesions like inflammatory lesions, Meckel’s diverticulum, postoperative adhesions, lipoma, adenomatous polyps, lymphoma and metastases or even in patients with a gastrojejunostomy [8,9]. Up to 30% of cases of intussusception are due to malignancy in the small intestine [10].
The aim of this case report is to remind that some very rare aetiology may be involved in adult intestinal obstruction.
Case Report
A 27 year old female with no known medical illness presented to the emergency department of our institute after experiencing abdominal distension, colicky pain and vomiting that had been worsening over the past one week duration. The diagnosis of small bowel obstruction was made and patient was immediately operated. Per operatively ileo-ileal intussusception along with a mass was identified and the specimen was sent for histopathological examination. Clinically no impression was made for the mass.
Post-operative period was uneventful and the patient was discharged after five days.
Grossly we received a part of small intestine measuring 12.2×5 cm with a polypoidal, dumbbell shaped mass measuring 4×3.5×1 cm arising from the mucosal surface at one end of the small bowel. Outer surface of the polyp was greyish to blackish and cut surface was solid, grey, white and glistening with few myxoid areas (Figure 1).
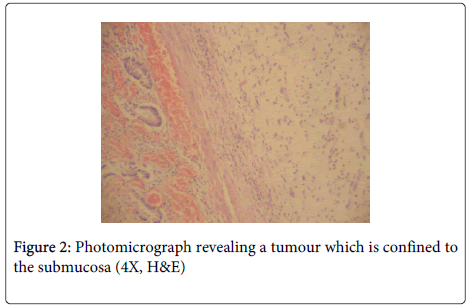
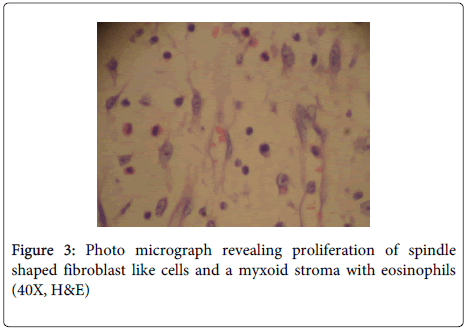
Microscopy: Representative sections examined from the polyp reveal an ulcerated small bowel mucosa and proliferation of spindle shaped fibroblast like cells arranged concentrically around blood vessels in the submucosa and reaching upto the muscularis propria (Figure 2). These cells are spindled shaped having vesicular chromatin, visible nucleoli and indistinct cytoplasm. The stroma is myxoid with presence of chronic inflammatory cells comprising predominantly of eosinophils, plasma cells and lymphocytes (Figure 3).
Discussion
Inflammatory fibroid polyp is a benign GI tumor that appears grossly as a localized, submucosal, sessile polypoid mass. IFP was first described by Vanek in 1949 as “gastric submucosal granulomas with eosinophilia” and a variety of names such as eosinophilic granulomas, hemangiopericytoma, polypoid fibroma, gastric fibroma with eosinophils and inflammatory pseudotumor [11].
Stomach is the most commonly involved location, and most lesions are located in the gastric antrum along the lesser and greater curvatures. It occurs less frequently in the distal ileum and very rarely in the colon, jejunum, duodenum and esophagus [1]. IFP can be found in all age groups, but peak incidence is between the sixth and seventh decades [12]. Nausea, vomiting, gastrointestinal bleeding, change in bowel habits, constipation or abdominal distension are the nonspecific symptoms and signs of intussusception [5,6]. Obstruction symptoms, such as vomiting and abdominal pain, were frequent initial symptoms of those with IFPs in the small intestine [13].
In the case reported here, an adult female presented with abdominal distension, colicky pain and vomiting. Grossly a sessile, polypoidal tumor was located at one end of the ileum measuring 4 cm in maximum diameter which was responsible to cause ileo-ileal intussusception in this patient.
Macroscopically it can be seen as a sessile or a polypoid lesion, usually measure between 2 and 5 cm in diameter. However, there are also giant IFPs with a size of up to 12.5 cm in diameter having been reported [13]. Microscopically the lesion is composed of myofibroblasts, blood vessels and various inflammatory cells including eosinophils, lymphocytes and plasma cells [14].
While the pathogenesis of IFP is unknown, development on an allergic basis, neural hyperplasia and form of granulation tissue has been suggested in the etiology [15].
Pre-operative diagnosis is of always important, if malignant lesion is confirmed preoperatively, radical resection is more confident; if benign lesion is diagnosed, limited resection is enough [16]. Operative resection of the involved intestine with macroscopically clear margins is the treatment of choice for IFPs. Inadequate resection margins may leave involved bowel and predispose to disease recurrence. To date, there have been two reported cases in the literature where IFPs recurred after incomplete resection [16,17,18].
The gastrointestinal stromal tumour (GIST) is an important consideration in the histological differential diagnosis of IFPs, and in morphologically ambiguous cases, immunohistochemistry is used to make a distinction between the two. Both tumours are positive for CD34 and vimentin, but GISTs are positive for CD117 (c-kit), while IFPs are not [19,20].
IFPs have no metastatic potential. They remain dormant until they are large enough to produce local symptoms that are dependent on their location. Small bowel lesions are not usually diagnosed pre-operatively because they present with vague symptoms of bowel obstruction due to intussusception. Laboratory investigations and plain radiographs are not helpful in making the diagnosis as they will demonstrate non-specific findings that are more in keeping with bowel obstruction [21].
Various studies have been published in the past also concluded that, intussusception secondary to IFPs of the small intestine are difficult to diagnose without recognition of its clinical and pathological characteristics. CT is useful in confirming an anatomical abnormality however; histological examination establishes the final diagnosis of IFPs [21,22].
Conclusion
Though IFP is a rare entity it should generally be taken into consideration as a differential diagnosis of peduncular polyp of the small intestine. IFP of small intestine is not fatal and patients remain asymptomatic in their daily life except for intussusception or bowel obstruction, if healthy bowel margins are secured macroscopically during segmental resection.
References
- Kim YI, Kim WH (1988) Inflammatory fibroid polyps of gastrointestinal tract. Evolution of histologic patterns. Am J ClinPathol 89: 721-727.
- HELWIG EB, RANIER A (1953) Inflammatory fibroid polyps of the stomach. SurgGynecolObstet 96: 335-367.
- Navan PJJ, Colina RF, Sanchez L, Cester CJ (1983) Inflammatory fibroid polyp of the gastrointestinal tract. An Immunohistochemical& electron microscopic study. Cancer 51: 1682-1690.
- Azar T, Berger DL (1997) Adult intussusception. Ann Surg 226: 134-138.
- Weilbaecher D, Bolin JA, Hearn D, Ogden W 2nd (1971) Intussusception in adults. Review of 160 cases. Am J Surg 121: 531-535.
- Akçay MN, Polat M, Cadirci M, Gencer B (1994) Tumor-induced ileo-ileal invagination in adults. Am Surg 60: 980-981.
- Hutchinson H, Hutchinson J (1946) Jonathan Hutchinson, life and letters. (1st Edn) Wm Heinemann Medical Books: London.
- Ishii M, Teramoto S, Yakabe M, Yamamato H, Yamaguchi Y, et al. (2007) Small intestinal intussusceptions caused by percutaneous endoscopic jejunostomy tube placement. J Am GeriatrSoc 55: 2093-2094.
- Archimandritis AJ, Hatzopoulos N, Hatzinikolaou P, Sougioultzis S, Kourtesas D, et al. (2001) Jejunogastric intussusception presented with hematemesis: a case presentation and review of the literature. BMC Gastroenterol 1: 1.
- Begos DG, Sandor A, Modlin IM (1997) The diagnosis and management of adult intussusception. Am J Surg 173: 88-94.
- VANEK J (1949) Gastric submucosal granuloma with eosinophilic infiltration. Am J Pathol 25: 397-411.
- de la Plaza R, Picardo AL, Cuberes R, Jara A, Martínez-Peñalver I, et al. (1999) Inflammatory fibroid polyps of the large intestine. Dig Dis Sci 44: 1810-1816.
- Nkanza NK, King M, Hutt MS (1980) Intussusception due to inflammatory fibroid polyps of the ileum: a report of 12 cases from Africa. Br J Surg 67: 271-274.
- Harned RK, Buck JL, Shekitka KM (1992) Inflammatory fibroid polyps of the gastrointestinal tract: radiologic evaluation. Radiology 182: 863-866.
- Gönül II, Erdem O, Ataoglu O (2004) Inflammatory fibroid polyp of the ileum causing intussusception: a case report. Turk J Gastroenterol 15: 59-62.
- Anthony PP, Morris DS, Vowles KD (1984) Multiple and recurrent inflammatory fibroid polyps in three generations of a Devon family: a new syndrome. Gut 25: 854-862.
- Chen HP, Liu KW, Lee CT, Hwang JC (2010) Inflammatory fibroid polyp of colon presented with colonic intussusception: report of a case. E-Da Med J 1.
- McGreevy P, Doberneck RC, McLeay JM, Miller FA (1967) Recurrent eosinophilic infiltrate (granuloma) of the ileum causing intussusception in a two-year-old child. Surgery 61: 280-284.
- Cooper HS. Intestinal neoplasms (1999) In: Sternberg SS, Antonioli DA, Carter D, Mills SE, Oberman HA (Ed) Diagnostic surgical pathology, (3rd Edn) Lippincott Williams & Wilkins, Philadelphia: 1423-1424.
- Wysocki AP, Taylor G, Windsor JA (2007) Inflammatory fibroid polyps of the duodenum: a review of the literature. Dig Surg 24: 162-168.
- Cawich S, Gibson T, Mitchell D, Williams E, Newnham M, et al. (2007) Adult intussusception from an inflammatory fibroid polyp: a case report and review of literature. The internet journal of pathology 7: 1.
- Rabbani K, Narjis Y, Jgounni R, Semlani Z, Difaa A, et al. (2012) Adult intussusception caused by an inflammatory fibroid ileal polyp. ActaChirBelg 112: 157-159.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 14606
- [From(publication date):
December-2014 - Jul 11, 2025] - Breakdown by view type
- HTML page views : 10005
- PDF downloads : 4601