Intravenous Ketamine Produces Long-Term Pain Relief in a Patient with Fibromyalgia
Received: 27-Jan-2016 / Accepted Date: 17-Feb-2016 / Published Date: 20-Feb-2016
Abstract
Fibromyalgia is a common chronic widespread pain disorder for which there remains no gold standard treatment option. Here, we report a case of fibromyalgia in a female patient whose pain was refractory to treatment options such as a radiofrequency ablation, opioid analgesics and other pharmacotherapies. The patient commenced an experimental intravenous ketamine infusion therapy at the Florida Spine Institute (Clearwater, FL) and achieved complete remission from her chronic pain, an improved quality of life, and was able to reduce her reliance on multiple analgesic medications. Most interestingly, the patient has continued to report no pain in regular follow up visits for more than one year since her last ketamine infusion.
Keywords: Fibromyalgia; Ketamine; Analgesia; Chronic pain; Intravenous; Opioids
4745Abbreviations
FM: Fibromyalgia; IV: Intravenous; PCP: Phencyclidine; USFDA: United States Food and Drug Administration; ACR: American College of Rheumatology; VAS: Visual Analog Scale
Introduction
Ketamine (2-(2-chlorophenyl)-2-(methylamino)-cyclohexanone) is a second-generation anesthetic, first synthesized in the early 1960s as a safer alternative to phencyclidine (PCP) [1]. It exists in two stereoisomeric forms, S(+) and R(-). The S(+) isomer is the most potent NMDA receptor antagonist known and is approximately three to four times that of the R(-) isomer. It has been used as a dissociative anesthetic since it’s approval by the United States Food and Drug Administration (FDA) in 1970. Today, it is experiencing a strong resurgence in off-label use as an analgesic for chronic pain thought to be neuropathic in origin [2].
Neuropathic pain has failed to be completely understood in the scientific community. The medical management of neuropathic pain generally consists of five main classes of oral medications: antidepressants with reuptake blocking effect, anticonvulsants with sodium-blocking action, anticonvulsants with calcium modulating actions, tramadol, and opiates [3]. Unfortunately, these treatment options have failed to adequately manage the pain levels of patients with a chronic neuropathic pain condition such as fibromyalgia (FM).
FM is even more poorly understood from a mechanistic perspective but some regard it as neuropathic in origin [4]. It’s diagnosis criteria is often highly debated and varies drastically, however, the American College of Rheumatology (ACR) have recently published a widely used set of criteria for the diagnosis of FM [5]. According to the ACR, a patient satisfies diagnostic criteria for FM if the following three conditions are met:
• Widespread pain index (WPI) ≥ 7 and symptom severity (SS) scale score ≥ 5 or WPI 3-6 and SS scale score ≥ 9.
• Symptoms have been present at a similar level for at least 3 months.
• The patient does not have a disorder that would otherwise explain the pain.
Unsurprisingly, treatment options for FM are no different than those described for the treatment of neuropathic pain [4]. Furthermore, these treatment options have led to unsatisfactory outcomes and have pushed the scientific and medical community to begin searching for alternative therapeutic options. Experimental treatments include the intravenous infusion of various agents such as morphine, lidocaine, or ketamine. A previous double-blind, placebocontrolled clinical study evaluated the analgesic efficacy of the each of these agents in 31 patients with FM. These investigators reported no improvement in the morphine group, some improvement in the lidocaine group, and a significant reduction in pain intensity in the group that received intravenous ketamine [6]. These authors conclude that NMDA antagonism is a promising target for the treatment of FM. This NMDA hypothesis has fueled many studies involving nonanesthetic doses of ketamine infused over several hours often for four consecutive days or more for treating chronic pain [7,8]. Another recent study found that non-anesthetic doses of ketamine reduced muscle pain, temporal summation, and referred pain in FM patients [9]. Although not yet established as a gold standard treatment option, ketamine infusions represent a glimmer of hope for a subset of patients who desperately need just that.
Case Report
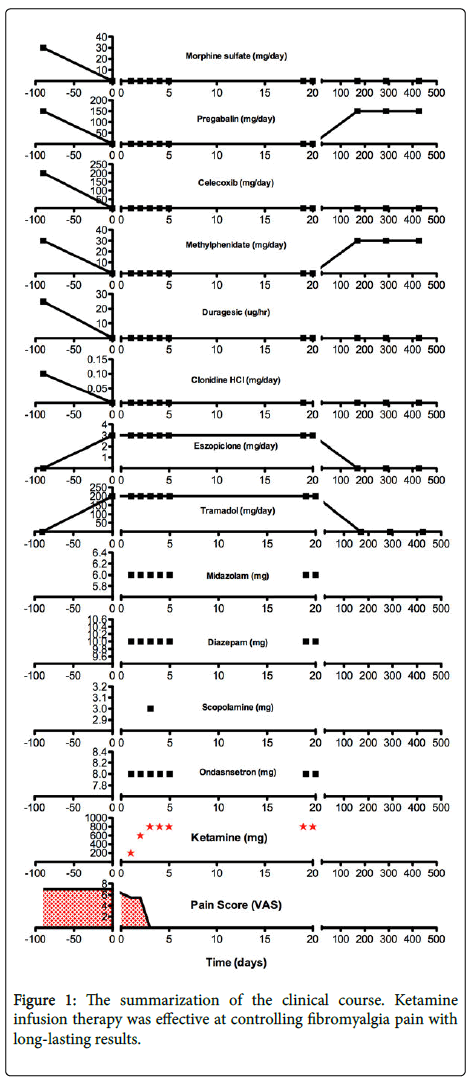
A 61-year old female was referred to the Florida Spine Institute (Clearwater, FL) and presented with chronic pain that had previously been under management by her primary care physician. Figure 1 illustrates this patient’s clinical course, described herein. Over the course of three years the patient underwent a medical branch block (lubmbar), achieving 50% pain relief.
Approximately three months after the medial branch block, she underwent radiofrequency ablation of the left lumbar region. One year later, she underwent bilateral lumbar radiofrequency ablation. On June 26, 2014, the patient was diagnosed with FM and her active medication list at that time included morphine sulfate (15 mg tablet, twice daily), pregabalin (150 mg Lyrica capsule, once daily), celecoxib (200 mg Celebrex capsule, once daily), transdermal fentanyl patch (Duragesic 25 ug/h patch, replaced every 72 h), methylphenidate (10 mg Ritalin tablet, three times daily), and clonidine hydrochloride (0.1 mg tablet, once daily). Still her pain levels, which were measured using a standard pain questionnaire that quantitatively scored pain levels using a Visual Analog Scale (VAS), were reported as 7/10. Due to the patient’s underwhelming results with all other pain treatments, we discussed the possible benefits and risks of intravenous (IV) ketamine therapy for pain relief related to FM to which the patient agreed was her preferred course of action. The patient was tapered off fentanyl and morphine sulfate per physician instruction and on September 24, 2014, her active medication list included eszopiclone (3 mg Lunesta tablet, once daily), tramadol (50 mg Ultram, as needed up to 4 times daily), and clonidine hydrochloride (0.1 mg tablet, once daily).
On October 13, 2014, the patient started a five-day IV ketamine treatment protocol at the Florida Spine Institute, overseen by Dr. Ashraf Hanna. For the first day, the patient was infused over the course of 4 h with 200 mg ketamine, 10 mg diazepam (Valium), and an IV push of 8 mg ondasnsetron (Zofran) in 100 ml of normal saline. Following the first infusion, the patient reported a pain score of 5-6/10. On the second day, the patient was infused over the course of 4 h with 600 mg ketamine, 6 mg midazolam (Versed), 10 mg diazepam (Valium), and an IV push of 8 mg ondansetron (Zofran) in 100 ml bag of normal saline. On the third day, the ketamine dosage was escalated to 800 mg/100 mL of normal saline. No serious complications were experienced throughout the treatment protocol. Minor complications included nausea, which was controlled with a scopolamine patch (1.5 mg every 72 h, as needed), and agitation towards the end of infusion. The patient reported complete abolishment of pain following the third infusion (0/10 by VAS). The fourth infusion remained unchanged from the third. Following completion of the fourth infusion, the patient reported complete abolishment of pain (0/10 by VAS). The fifth day of consecutive infusion utilized the same dosages as days 3 and 4 (800 mg ketamine). Following completion of the fifth infusion, her pain levels remained at 0/10.
Approximately two weeks following the completion of the ketamine infusion, the patient reported back to the clinic for a two-day booster infusion regimen (800 mg ketamine in 100 mL normal saline over four hours). Her pain levels remained 0/10 at this time and the booster was well tolerated on both days of booster infusion. Five months post ketamine therapy, the patient reported back to the clinic for a follow up visit. She reported active medications including only pregabalin (150 mg Lyrica capsule, once daily) and methylphenidate (10 mg Ritalin tablet, three times daily). Her pain levels remained 0/10 at this time. She has continued quarterly follow up visits to the clinic, reporting pain levels of 0/10 at each. Her most recent visit was more than one year since her last ketamine infusion and still denies having any pain.
Conclusion
To the best of our knowledge, this is the longest-lasting positive treatment outcome in a FM patient treated with IV ketamine infusion. A previous double blind, active placebo controlled trial using twentyfour (twelve per group) FM patients found only short-term analgesic effects that appeared to follow the pharmacokinetics of ketamine [10]. However, this study utilized a much lower dose of ketamine infused once for only thirty minutes. In contrast, Sigtermans et al. utilized a 100 hour infusion regimen with doses titrated up to 20-30 mg per hour. They reported pain relief in Complex Regional Pain Syndrome (CRPS) Type 1 patients for up to three months from their last infusion using this regimen [11]. Similarly, Schwartzman et al. used a daily four-hour infusion of ketamine for 10 days in CRPS patients and achieved statistically significant reductions in many pain parameters for three months post infusion [12]. Taken together with the present case study, there is significant evidence to suggest that dose and duration of ketamine infusion is paramount to achieve long duration analgesia in neuropathic pain patients. These findings merit further investigation via a large, randomized, placebo-controlled clinical trial with multiple dose levels and a long-term follow-up period such that a gold standard regimen can be established for the treatment of patients with notoriously difficult to treat chronic neuropathic pain conditions such as FM or CRPS.
Disclosures
The authors declare that there is no conflict of interest regarding the publication of this paper.
References
- Quibell R, Prommer EE, Mihalyo M, Twycross R, Wilcock A (2011) Ketamine*. J Pain Symptom Manage 41: 640-649.
- Baron R (2009) Neuropathic pain: a clinical perspective. HandbExpPharmacol 194: 3-30.
- Martinez-Lavin M (2006) Fibromyalgia is a neuropathic pain syndrome. J Rheumatol 33: 827-828.
- Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg DL, Katz RS, et al. (2010) The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res (Hoboken) 62: 600-610.
- Sorensen J, Bengtsson A, Bäckman E, Henriksson KG, Bengtsson M (1995) Pain analysis in patients with fibromyalgia. Effects of intravenous morphine, lidocaine, and ketamine. Scand J Rheumatol 24: 360-365.
- Kosharskyy B, Almonte W, Shaparin N, Pappagallo M, Smith H (2013) Intravenous infusions in chronic pain management. Pain Physician 16: 231-249.
- Sheehy KA, Muller EA, Lippold C, Nouraie M, Finkel JC, et al. (2015) Subanesthetic ketamine infusions for the treatment of children and adolescents with chronic pain: a longitudinal study. BMC Pediatr 15: 198.
- Graven-Nielsen T, Aspegren Kendall S, Henriksson KG, Bengtsson M, Sörensen J, et al. (2000) Ketamine reduces muscle pain, temporal summation, and referred pain in fibromyalgia patients. Pain 85: 483-491.
- Noppers I, Niesters M, Swartjes M, Bauer M, Aarts L, et al. (2011) Absence of long-term analgesic effect from a short-term S-ketamine infusion on fibromyalgia pain: a randomized, prospective, double blind, active placebo-controlled trial. Eur J Pain 15: 942-949.
- Sigtermans MJ, van Hilten JJ, Bauer MC, Arbous MS, Marinus J, et al.(2009) Ketamine produces effective and long-term pain relief in patients with Complex Regional Pain Syndrome Type 1. Pain 145: 304-311.
- Schwartzman RJ, Alexander GM, Grothusen JR, Paylor T, Reichenberger E, et al. (2009) Outpatient intravenous ketamine for the treatment of complex regional pain syndrome: a double-blind placebo controlled study. Pain 147: 107-115.
Citation: Hanna AF, Smith AJ (2016) Intravenous Ketamine Produces Long-Term Pain Relief in a Patient with Fibromyalgia. Fibrom Open Access 1:104.
Copyright: ©2016 Hanna AF, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Usage
- Total views: 18293
- [From(publication date): 3-2016 - Apr 05, 2025]
- Breakdown by view type
- HTML page views: 17208
- PDF downloads: 1085