Intravascular Lymphoma: Look for the Less Obvious!
Received: 29-Mar-2018 / Accepted Date: 24-Apr-2018 / Published Date: 02-May-2018 DOI: 10.4172/2476-2253.1000115
Abstract
Intravascular large B cell lymphoma (IVBCL) is a rare subtype of extranodal large B-cell lymphoma with a distinct presentation. Anatomically the disease is characterized by the proliferation of clonal lymphocytes within small vessels with relative sparing of the surrounding tissue. The clinical symptoms of the disease are dependent on the specific organ involvement, which often includes the central nervous system and skin. Because of the various modes of presentation and the rarity of IVBCL, the diagnosis is challenging and made post-mortem in most cases. The tumor is often disseminated at the time of diagnosis and prognosis is poor, even with aggressive chemotherapy. The spectrum of neurological presentations of IVBCL can be heterogeneous. We report a case of intravascular lymphoma diagnosed on autopsy.
Keywords: Lymphoma; Lymphoproliferative disease
Abbreviations
IVBCL: Intravascular Large B Cell Lymphoma
Introduction
Intravascular large B cell lymphoma (IVBCL) is a rare type of non- Hodgkin’s lymphoma (NHL) characterized by the proliferation of lymphoma cells within the lumina of small blood vessels, particularly capillaries and post-capillary venules, without an obvious extravascular tumor mass or readily observable circulating lymphoma cells in the peripheral blood. This type of lymphoma has also been described as intravascular lymphomatosis, angiotropic large cell lymphoma, and malignant angioendotheliomatosis. Originally described by Pfleger et al. in 1959 as an endothelial neoplasm with cutaneous involvement, this lymphoproliferative disease is now regarded as a well-defined entity in the WHO classification of lymphoid malignancy revised in 2017 [1]. The clinical presentation is varied and often includes symptoms related to organ dysfunction caused by occlusion of blood vessels [2]. The diagnosis is challenging and, especially in the past, was usually recognized at the autopsy. In recent years, the heightened awareness of IVBCL has resulted in more patients being diagnosed during life, thereby allowing for treatment. The true incidence is unknown. Median age at diagnosis is in the sixth to seventh decades; there is no sex predilection [2].
There are two types of presentation: a Western form and an Asian variant, seen mainly in Japan. This lymphoma shows a propensity to manifest itself more frequently with CNS and cutaneous symptoms in Western countries or with hemophagocytic syndrome in Asian countries, mainly Japan [3,4].
Patients may be asymptomatic or symptomatic, presenting with fever of unknown origin, mental status, or personality changes.
Case Presentation
An ex-smoker, diabetic, hypertensive 76-year-old man was admitted to our hospital with weight loss of about 10 kg in recent months, progressive cognitive decline, psycho-motor agitation, confusion and subsequent ideo-motor slowdown in the context of a clinical history of relapsing ischemic stroke and worsening cognitive decay over a period of about 5 months. Some months before he had first episode of confusion, dysarthria, left facial deficiency of central type and postural instability, with a diagnosis of "cerebral ischemia in the frontal and right globuspallidus" and he began cardiovascular therapy with Clopidogrel. Later he underwent a new hospitalization for acute force deficit and drowsiness and subsequently discharged with the diagnosis of multiple ischemic lesions of the left and right hemisphere. During hospitalization in our hospital the brain CT scan revealed a lowdensity area in the cortical-subcortical right parietal lobe; laboratory tests showed elevated serum lactate dehydrogenase (LDH), beta-2 microglobulin, elevated sedimentation rate (VES) and elevated neuron specific enolase (NSE) and elevated antinuclear antibody (ANA). As cerebral vasculitis was suspected, corticosteroid therapy was initiated but clinical response was mild and transient.
Subsequently, clinical condition worsened complicating with metabolic acidosis, ipovolemic hypernatremia, sepsis, septic shocks, leading to a fatal evolution.
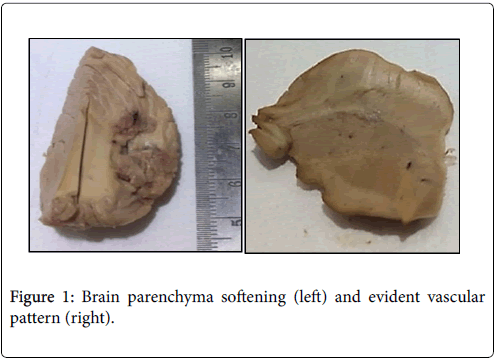
Autopsy revealed diffuse edema of the brain with multiple softening areas, the largest in the right frontal seat (3 cm) and in the right cerebellar seat (2.7 cm). The vascular pattern appears particularly evident throughout the brain (Figure 1).
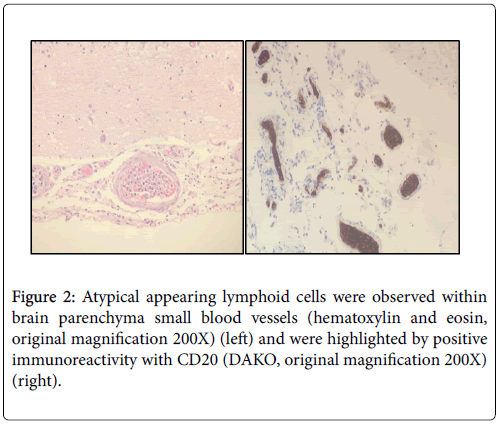
Histological examination of cerebral and cerebellar tissue was characterized by areas of ischemic necrosis with colliquative phenomena. The areas vary in size from macroscopic to point. In the small and medium caliber vessels, we documented aggregates of large size atypical lymphoid cells obstructing vascular lumen. These cells showed immunohistochemical stain for CD20 and were also documented in other tissue as lung, kidney and heart (Figure 2).
Discussion
The clinical diagnosis of IVBCL may be difficult. Cases with cutaneous involvement can be confirmed by skin biopsy, but neurological symptoms can be heterogenous and could be interpreted as vasculitis [5,6]. Delays in diagnosis due to the subtlety and focal nature of the intravascular infiltrates often lead to a terminal disease with death before chemotherapy is initiated. [6,7]
Moreover, from the pathogenetic point of view, the precise mechanisms responsible for intravascular localization are at the moment largely unknown. Ponzoni et al. in an elderly but still valid immunohistochemical study proposed a very intriguing model. In a few words, in IVBCL, the second phase of the neoplastic cellendothelial interaction, termed locking, is altered due to the lack on the surface of neoplastic cells of several molecules, as CD29 (beta integrin) and CD54 (ICAM-1), thus preventing movement of neoplastic cells through the vessels [1].
Other explanations have included the aberrant expression of CD11a and CD49d (VLA-4) on IVBCL cells as a possible mechanism because these adhesion molecules would enable tumor cells to home to CD54 (CD11a ligand) and CD106 (CD49d ligand), which are expressed on endothelial cell surfaces, and alternatively, a deficiency in the Hermes-3-defined homing receptor antigen and lack of the receptor for peanut agglutinin [5,8,9].
Furthermore, as IVBCL is up till now a fatal disease characterized by an aggressive course and a short outcome, in 2005, under the sponsorship of the International Extranodal Lymphoma Study Group, pathologists and clinicians, discussed during an operative meeting in Locarno, Switzerland, all the problematic aspects, such as the definition of the disease, the clinical variants and therapeutic strategies, and the histopathologic features and their differential diagnoses [10].
Conclusion
In conclusion, our case of IVBCL suggest, once more, that this special type of lymphoproliferative disease, must be kept distinct, in all clinical situations refractory to treatments considered for the primary diagnosis, even performing random biopsy in apparent uninvolved organs.
Acknowledgement
The authors are deeply grateful to the laboratory staff for excellent technical assistance.
References
- Ponzoni M, Arrigoni G, Gould VE, Del Curto B, Maggioni M, et al. (2000) Lack of CD 29 (beta1 integrin) and CD 54 (ICAM-1) adhesion molecules in intravascular lymphomatosis. Hum Pathol 31: 220-226.
- Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, et al. (2017) WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues: World Health Organization Classification of Tumours. (4thedn) IARC Publications, Lyon, France.
- Ferreri AJ, Campo E, Seymour JF, Willemze R, Ilariucci F, et al. (2004) Intravascular lymphoma: clinical presentation, natural history, management and prognostic factors in a series of 38 cases, with special emphasis on the 'cutaneous variant'. Br J Haematol 127: 173-183.
- Murase T, Nakamura S, Kawauchi K, Matsuzaki H, Sakai C, et al. (2000) An Asian variant of intravascular large B-cell lymphoma: clinical, pathological and cytogenetic approaches to diffuse large B-cell lymphoma associated with haemophagocytic syndrome. Br J Haematol 111: 826-834.
- Zuckerman D, Seliem R, Hochberg E (2006) Intravascular lymphoma: the oncologist's "great imitator". Oncologist 11: 496-502.
- Garcia-Munoz R, Rubio-Mediavilla S, Robles-de-Castro D, Munoz A, Herrera-Perez P, et al. (2014) Intravascular large B cell lymphoma. Leuk Res Rep 3: 21-23.
- Prayson RA (2016) Intravascular lymphoma mimicking vasculitis. J Clin Neurosci 34: 224-225.
- Kanda M, Suzumiya J, Ohshima K, Tamura K, Kikuchi M, et al. (1999) Intravascular large cell lymphoma: clinicopathological, immuno-histochemical and molecular genetic studies. Leuk Lymphoma 34: 569-580.
- Ferry JA, Harris NL, Picker LJ, Weinberg DS, Rosales RK et al. (1988) Intravascular lymphomatosis (malignant angioendotheliomatosis). A B-cell neoplasm expressing surface homing receptors. Mod Pathol 1: 444-452.
- Ponzoni M, Ferreri AJ, Campo E, Facchetti F, Mazzucchelli L, et al. (2007) Definition, diagnosis, and management of intravascular large B-cell lymphoma: proposals and perspectives from an international consensus meeting. J Clin Oncol 25: 3168-3173.
Citation: Bianchi A, Falcone L, Ricci L, Tombini M, Annibali O (2018) Intravascular Lymphoma: Look for the Less Obvious!. J Cancer Diagn 3: 116. DOI: 10.4172/2476-2253.1000115
Copyright: © 2018 Bianchi A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 5594
- [From(publication date): 0-2018 - Apr 04, 2025]
- Breakdown by view type
- HTML page views: 4777
- PDF downloads: 817