Clinical images Open Access
Intratissue Percutaneous Electrolysis (EPI®) in the Treatment of Achilles Tendinopathy
Jose Manuel Sánchez-Ibáñez*Sports Rehabilitation Center (CEREDE), Barcelona, Spain
- *Corresponding Author:
- Jose Manuel Sánchez-Ibáñez
Sports Rehabilitation Center (CEREDE)
Barcelona Clinic, Spain
Tel: +34 934 523 510
E-mail: drsanchez@cerede.es
Received date: December 12, 2016; Accepted date: December 16, 2016; Published date: December 19, 2016
Citation: Sánchez-Ibáñez JM (2016) Intratissue Percutaneous Electrolysis (EPI®) in the Treatment of Achilles Tendinopathy. J Nov Physiother 7: i101. doi: 10.4172/2165-7025.1000i101
Copyright: © 2016 Sánchez-Ibáñez JM. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Novel Physiotherapies
Intratissue Percutaneous Electrolysis
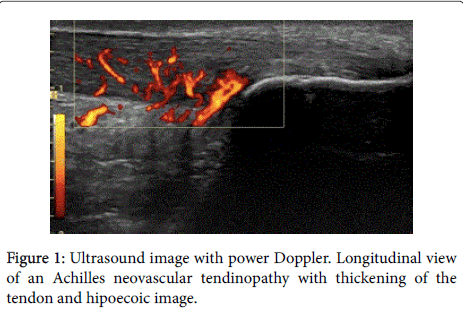
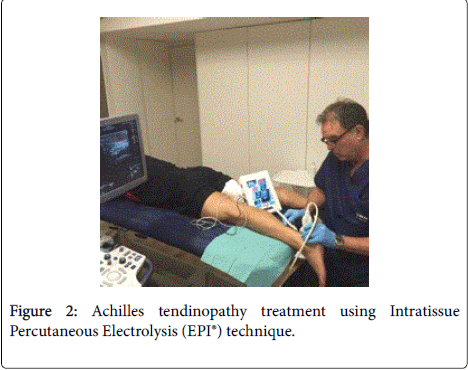
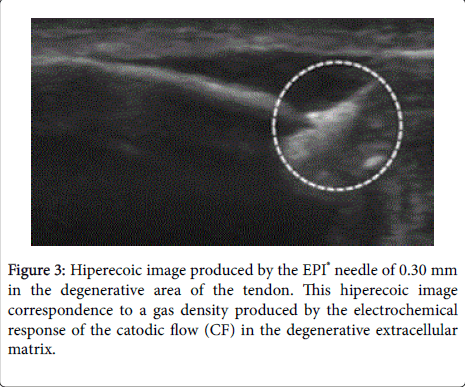
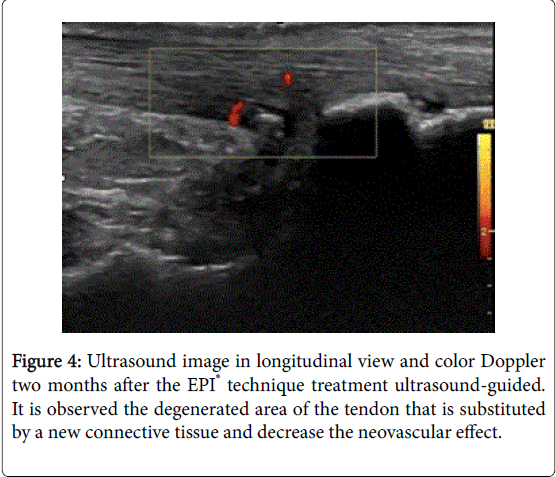
Intratissue percutaneous electrolysis (EPI®) ultrasound-guided treatment [1-5] is the application of a direct current (DC) whose catodic flow is transferred to the area of the degenerative tendon [6-8] using an acupuncture needle. This accumulated electrical charge (AEC) in the degenerative tissue will produce the activation of the molecular, cellular and biological processes necessary to restore the regeneration mechanisms of the tendon (Figures 1 and 2). In recent studies it has been demonstrated that EPI® technique is effective in tendinopathy and sport muscular injuries (Figures 3 and 4).
References
- Sànchez-IbàñezJM (2015) Ultrasound-Guided EPI® Technique: New Treatment for for Degenerative Tendinopathy. J Nurs Care 4: 310.
- Sànchez-IbàñezJM, Fernández ME, MonllauJC, Alonso-Díez A, Jesús Sánchez-García J, et al. (2015) New Treatments for Degenerative Tendinopathy, focused on the Region-Specific of the Tendon. Rheumatology (Sunnyvale) 5:173.
- Sànchez-IbàñezJM, Fernàndez ME, Moreno C, Marti D, Belón P (2015) Ultrasound-Guided EPI® technique and eccentric exercise, new treatment for Achilles and Patellar tendinopathy focused on the region-specific of the tendon. OrthopMuscular Syst 4: 200.
- Abat F, Valles SL, Gelber PE, Polidori F, Sanchez-Ibáñez JM et al. (2015) An experimental study of muscular injury repair in a mouse model of notexin-induced lesion with EPI® technique. BMC Sports Sci Med Rehabil 7:7.
- Sanchez-IbañezJM, Colmena C, Benabent J, Garcia-Herreros S, Valles SL (2013) New Technique in Tendon Sport Recovery. Percutaneous Electrolysis Intratissue (EPI®). Int J Phys Med Rehabil 1: 113.
- Abat F, Gelber P, Polidori F, MonllauJC, Sánchez-Ibáñez JM (2014) Clinical results after ultrasound-guided intratissue percutaneous electrolysis (EPI®) and eccentric exercise in the treatment of patellar tendinopathy over a 10-year follow- up. Knee Surg Sports TraumatolArthrosc23: 1046-1052.
- Sánchez-Ibáñez JM, Alves R, Polidori F, Valera F, Minaya F, et al. (2013) Effectiveness of ultrasound-guided EPI® technique in the treatment of insertional patellar tendinopathy in soccer players. Br J Sports Med 47:e2.
- Sánchez-Ibáñez JM (2008) Ultrasound guided percutaneous electrolysis (EPI) in patients with chronic insertional patellar tendinophaty:a pilot study. Knee Surg Sports TraumatolArthrosc 16: 220-221.
Relevant Topics
- Electrical stimulation
- High Intensity Exercise
- Muscle Movements
- Musculoskeletal Physical Therapy
- Musculoskeletal Physiotherapy
- Neurophysiotherapy
- Neuroplasticity
- Neuropsychiatric drugs
- Physical Activity
- Physical Fitness
- Physical Medicine
- Physical Therapy
- Precision Rehabilitation
- Scapular Mobilization
- Sleep Disorders
- Sports and Physical Activity
- Sports Physical Therapy
Recommended Journals
Article Tools
Article Usage
- Total views: 3882
- [From(publication date):
February-2017 - Jul 12, 2025] - Breakdown by view type
- HTML page views : 3012
- PDF downloads : 870