Case Report Open Access
Intraosseous Malignant Peripheral Nerve Sheath Tumor of the Thoracic Spine: A Case Report and Review of Literature
Jung-Hee Lee and Chaisiri Chaichankul*Phramongkutklao College of Medicine, Bangkok, Thailand.
- *Corresponding Author:
- Dr. Chaisiri Chaichankul
Phramongkutklao College of Medicine
Bangkok, Thailand
E-mail: chaichankulc@yahoo.com
Received Date: February 22, 2016; Accepted Date: March 07, 2016; Published Date: March 13, 2016
Citation: Lee JH, Chaichankul C (2016) Intraosseous Malignant Peripheral Nerve Sheath Tumor of the Thoracic Spine: A Case Report and Review of Literature. J Orthop Oncol 2:107. doi:10.4172/2472-016X.1000107
Copyright: © 2016 Lee JH, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Orthopedic Oncology
Abstract
At the present time, only few reports including systematic reviews of malignant peripheral nerve sheath tumors (MPNSTs) with spinal involvement have been existed. Although there were reports of both MPNSTs of paraspinal soft tissue (type 1) resulting in secondary vertebral destruction and MPNSTs primarily originated from intraosseous of vertebra itself (type 2), these kinds of tumors are exceptionally rare. In this present report, we hereby demonstrated a case of type 2 MPNSTs which is not related to neurofibromatosis type 1 (NF 1) occurring in the thoracic spine and reviewed the clinical, radiologic, and pathologic as well as shared part of our experience in treating this rare condition. Interestingly, MPNSTs usually have a high rate of recurrence both local and metastasis even in the cases of successful en bloc resection with adjuvant therapy, but not in ours for 5-year follow up.
Keywords
Thoracic spine; Intraosseous malignant peripheral nerve sheath tumor; En bloc spondylectomy
Introduction
Malignant peripheral nerve sheath tumors (MPNSTs) are known as rare tumors [1]. Although they constitute 3-10% of all soft tissue sarcomas [2], the incidence of MPNSTs in general population is seldom reported (less than 1%) [3]. Given that the MPNSTs with spinal involvement are even more unusual. From previous literature, MPNSTs can be found sporadically ranging from 43-57% and nearly half of all MPNSTs associated with neurofibromatosis type 1(NF-1) [4]. In addition, the history of prior radiotherapy can be related to 3-11% of these tumors as well [5,6]. According to few reports as well as scant review literatures have been existed [3,4,7,8], the MPNSTs with spinal involvement are still considered as an infrequent topic. There were previous reports about MPNSTs at paraspinal soft tissue (type 1) resulting in secondary vertebral destruction [2] and MPNSTs primarily originated from intraosseous of vertebra itself (type 2); however, these kinds of tumors are still exceptionally rare, particularly for type2 MPNSTs.
In this present report, we hereby described a case of type 2 MPNSTs not related to NF-1 occurring in the thoracic spine and demonstrated the clinical, radiologic, and pathologic findings as well as shared part of our experience in treating this rare condition as well as reviewed some related literature.
Case Report
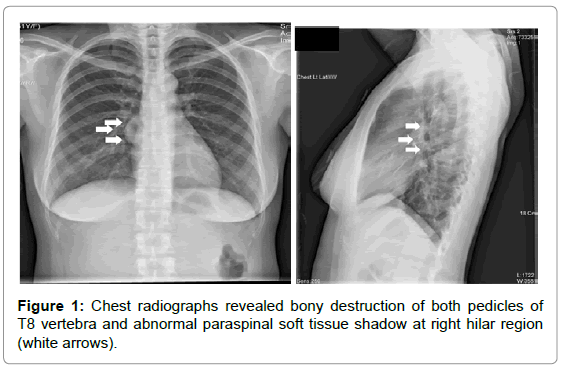
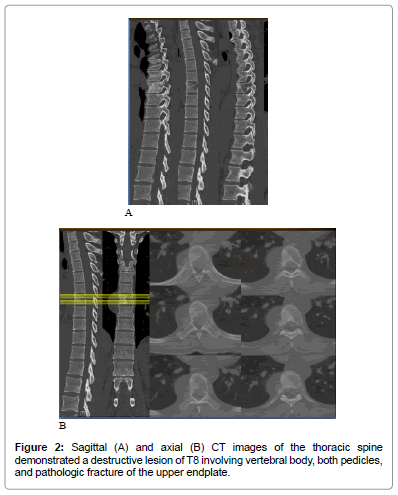
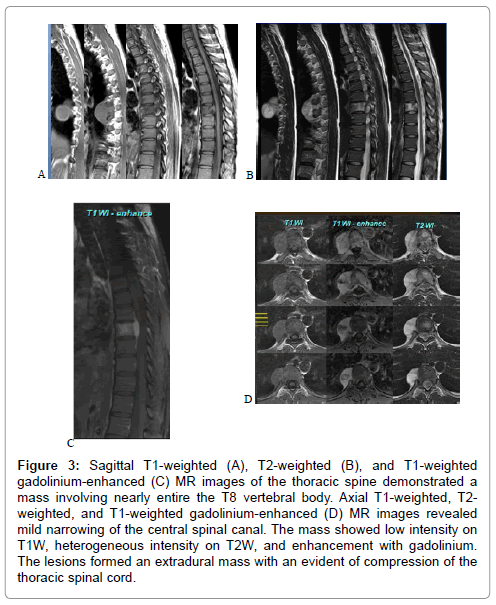
A 30-year-old woman initially presented to internal medicine outpatient clinic with a history of 2-week back pain, epigastric pain and insignificant weight loss. Systems review was noncontributory, except those details stated in the history of present illness. After gastroduodenoscopy and esophagography had revealed normal results, she was referred to our clinic. On examination, her gait and posture were demonstrated within normal limit. Neurological function was presented normal with good motor power, intact sensation and normal reflexes as well. No definite area of back pain could be located by physical examination. The earlier chest radiographs, however, revealed abnormal findings (Figure 1) with further supported by CT scan (Figure 2). An obtained MRI scan was performed and delineated an expansive soft-tissue mass which invaded the T8 vertebral body as well as both pedicles from T7 to T9 vertebra diffusely (Figure 3). According to relatively high prevalence of spinal metastasis including the other more common pathologies were suspected, PET/CT and whole body bone scan were performed. Whereas whole body bone scan did not demonstrate any abnormality focal tracer uptake, PET/CT scan showed an abnormal soft tissue uptake at the paraspinal area from T7 to T9.
Figure 3: Sagittal T1-weighted (A), T2-weighted (B), and T1-weighted gadolinium-enhanced (C) MR images of the thoracic spine demonstrated a mass involving nearly entire the T8 vertebral body. Axial T1-weighted, T2- weighted, and T1-weighted gadolinium-enhanced (D) MR images revealed mild narrowing of the central spinal canal. The mass showed low intensity on T1W, heterogeneous intensity on T2W, and enhancement with gadolinium. The lesions formed an extradural mass with an evident of compression of the thoracic spinal cord.
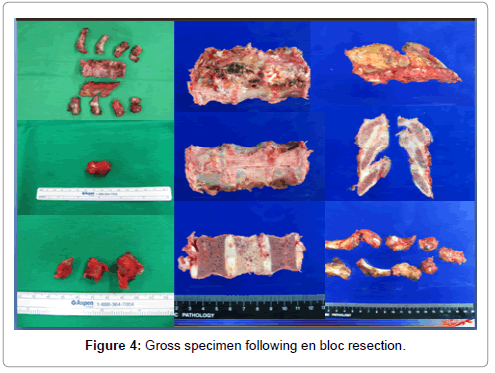
Because of several abnormalities from imaging findings, the authors decided to do the surgery with the goal of complete mass removal followed by reconstruction simultaneously. The removal tissues can be taken to make a definite diagnosis by the histopathological studies as well. Preoperatively, angiography and embolization was done using coils and gelfoam by interventional radiologist. Laminectomy of T7 to T9 and resection of both 7th to 9th proximal ribs were done initially. Then, en bloc resection of the tumor was undertaken in a fashion of single posterior approach by senior spine surgeon (JHL) under somatosensory and motor-evoked potential monitoring. The extradural mass together with T8 vertebra was completely excised, in conjunction with T7 and T9 corpectomy (Figure 4). Intraoperatively, the paraspinal mass was shown as minimal adherent to the pleura of right lung. After the https://www.omicsonline.org/open-access/enhancing-the-antitumor-effects-of-cancer-peptide-vaccine-therapy-2157-7560-1000330.php?aid=77294 in spinal canal was separated from dural sac and excised completely, an expandable cage used for reconstruction of the levels between T7 to T9 was filled in the defect. Finally, the pedicular screw fixation and fusion with mixed auto-iliac crest bone graft and tricalcium phosphate from the levels of T4 to T12 was performed.
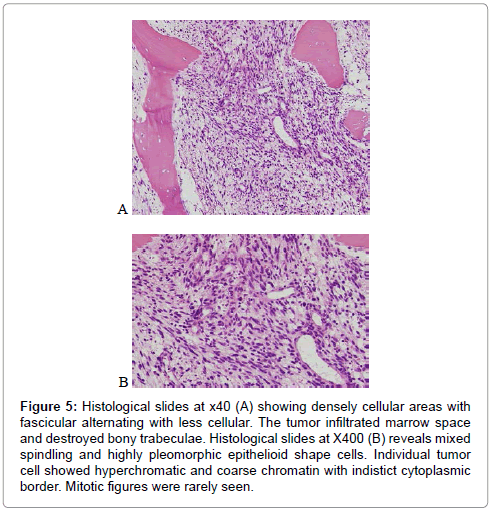
Histopathologically, the sections from the excised soft tissue mass revealed densely cellular fascicles alternating with hypocellular, myxoid zones and occasional nuclear palisading. Cytomorphologically, the nuclei were wavy, buckled, comma-shaped, and oval whereas cytoplasm was pale. Tumor cells displayed nuclear atypia and pleomorphism but generally lack of mitotic figures (Figure 5). In several foci, Wagner- Meissner body- like structure was identified. The sections from the T8 vertebral body and the 8th rib showed the same histologic picture as from the excised soft tissue mass.
Figure 5: Histological slides at x40 (A) showing densely cellular areas with fascicular alternating with less cellular. The tumor infiltrated marrow space and destroyed bony trabeculae. Histological slides at X400 (B) reveals mixed spindling and highly pleomorphic epithelioid shape cells. Individual tumor cell showed hyperchromatic and coarse chromatin with indistict cytoplasmic border. Mitotic figures were rarely seen.
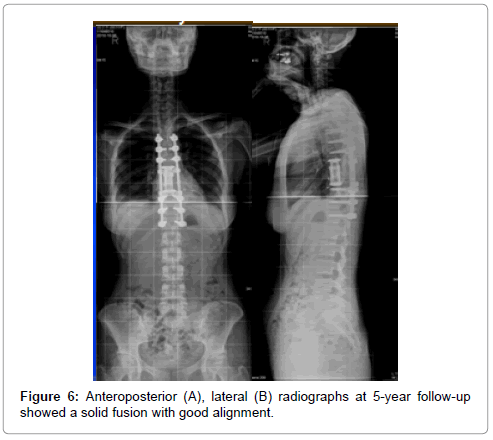
Postoperatively, plain spine radiographs confirmed satisfactory reconstruction, fixation, and sufficient resection. There were no change of motor, sensation and reflexes postoperatively. The patient was given local radiotherapy by receiving 49Gy in 23 fractions over 8 weeks to the effected spine. At 5-year follow-up, the plain radiographic images showed a solid fusion and acceptable appearance (Figure 6). Of note, the patient was asymptomatic without local recurrent or distant metastasis supported by MRI, whole body bone scan and PET/CT for 5-year follow-up.
Discussion
MPNSTs are kinds of soft tissue sarcomas arising from peripheral nerves or thought to be differentiated from nerve sheath elements including Schwann cells, fibroblasts, perineural cells or pluripotent cells of neural crest origin [7,9]. In the past, MPNSTs have interchangeable names as malignant schwannoma, malignant neurilemmoma, neruofibrosarcoma, or neurogenic sarcoma [7,10-14]. According to the previous reports, the occurrence of MPNSTs in NF-1 patients was 3% to 4.6%, and nearly 50% found in NF-1 patients [6,15]. We can classify the spinal MPNSTs into two types as described by Zhu et al. Specifically, type 1 or soft tissue type which can be further subclassified as type 1A (dumbbell) and type 1B (paravertebral) and type 2 or intraosseous type which the tumors originated from vertebral elements without soft tissue involvement [4]. Although MPNSTs generally arise as a result of malignant transformation of neruofibromas in patients with NF-1, it is not our case. Our presented case is type 2 (intraosseous) because intraoperative finding demonstrated the tumor mass originated from T8 vertebral body and outgrew as paraspinal soft mass that did not attach to the neighboring neural structures. From our current knowledge, this type of spinal MPNSTs has a small number of reported cases in the literatures [3,8,16,17]. The authors discovered only one paper written by Gnanalingham K et al, which reported about intraosseous MPNST occurred in the thoracic spine [8]. Furthermore, their surgical strategy reported in that paper was totally different from ours [8]. Because of the unspecific imaging findings of MPNSTs, inclusion of the differential diagnoses of other common primary bone sarcomas, spinal metastases and other common spinal pathologies should be kept in mind. For such a reason, the histopathological studies are necessary for definite diagnosis. Initially, the differential diagnoses were schwannomas, MPNSTs and other spindle cell sarcomas. In this patient, the histological and immunohistochemical studies revealed the most diagnosis of malignant peripheral nerve sheath tumor [3,4]. Although the demonstration of antibodies to S-100 were negative as well as the mitoses were seldom observed, the histologic features aimed to the diagnosis of low grade malignant peripheral nerve sheath tumor due to diffuse nuclear atypia, increased cellularity with abundant epithelioid features, and the result of ki-67 proliferation index>5% [3,4]. Of note, although the S-100 protein staining was negative in our case, the degree and pattern of staining for S100 can be varied in MPNSTs as described in previous studies [4,18].
Despite almost of malignant primary spinal tumors have an unfavorable outcome to chemotherapy and conventional radiotherapy, there are many studies supported to surgical treatment especially by the method of en bloc excision with negative surgical margin [19,20]. Recently, there was a retrospective study revealed that postoperative prognosis for MPNTs was quite poor with high recurrence and low survival rate in the condition of positive surgical margin [4,5,6,21- 23]. As demonstrated by previous study that patients with positive surgical margins have a 1.8-fold risk of local recurrence and a 1.1- fold risk of distant metastasis at 10-year cumulative incidence [22]. In addition, there is an increasing evidence of en bloc spondylectomy in the improvement on rate of local control and disease-free survival for primary malignant spinal tumors [24,25]. Theoretically, a complete surgical excision is critical to achieve optimal local control and overall survival for the spinal MPNSTs. However, even after total en bloc resection, about 32-65% of MPNSTs are realized to recur in a median interval of 5 to 32 months both local and metastasis [5,6,9,22]. Total en bloc spondylectomy can be performed through staged or simultaneous anterior and posterior approach, or posterior-only approach [26]. Originally, en bloc means to remove the lesion in a single piece; however, for the complexity of the spine and related structures, en bloc can mean remove the lesion in its entirety [27]. In this present case, we selected a posterior-only approach because of the benefit of achieving complete tumor resection and circumferential spinal reconstruction in a single setting. Due to the advancement of anatomical knowledge around spine, modern instruments, and neuromonitoring, en bloc for type 2 MPNSTs can be safely performed.
In conclusion, we reported a very rare case of primary intraosseous MPNSTs of the thoracic spine. From our review, to date, total en bloc spondylectomy could be the treatment of choice for the selected case of the spinal MPNSTs. Posterior-only approach can be performed safely with a delicate preoperative surgical planning and management in selected patient. For our case report, although evidence of local recurrence or metastasis spread were absent during the 5-year follow up, the longer period of follow up and a higher number of cases are necessary for further study.
References
- Chamoun RB, Whitehead WE, Dauser RC (2009) Primary disseminated intradural malignant peripheral nerve sheath tumor of the spine in a child: case report and review of the literature. PediatrNeurosurg 45:230-236
- Weiss SW, Goldblum JR, Enzinger, Weiss’s (2001) soft tissue tumours. Mosby Inc, St Louis
- Moon SJ, Lee JK, Seo BR, Kim JH, Kim SH, et al. (2008) An intraosseous malignant peripheral nerve sheath tumor of the cervical spine: a case report and review of the literature. Spine (Phila Pa 1976) 33: E712-716.
- Zhu B, Liu X, Liu Z, Yang S, Liao HI, et al. (2012) Malignant peripheral nerve sheath tumours of the spine: clinical manifestations, classification, treatment, and prognostic factors. Eur Spine J 21: 897-904.
- Wanebo JE, Malik JM, VandenBerg SR, Wanebo HJ, Driesen N, et al. (1993) Malignant peripheral nerve sheath tumors. A clinicopathologic study of 28 cases. Cancer 71: 1247-1253.
- Ducatman BS, Scheithauer BW (1983) Postirradiationneurofibrosarcoma. Cancer 51: 1028-1033.
- Ogawa BK, Skaggs DL, Kay RM (2009) Malignant peripheral nerve sheath tumor of the lumbar spine. Am J Orthop (Belle Mead NJ) 38: E89-92.
- Gnanalingham K, Bhattacharjee S, O'Neill K (2004) Intraosseous malignant peripheral nerve sheath tumor (MPNST) of the thoracic spine: a rare cause of spinal cord compression. Spine (Phila Pa 1976) 29: E402-405.
- Baehring JM, Betensky RA, Batchelor TT (2003) Malignant peripheral nerve sheath tumor: the clinical spectrum and outcome of treatment. Neurology 61: 696-698.
- D'Agostino AN, Soule EH, Miller RH (1963) Sarcomas of the Peripheral Nerves and Somatic Soft Tissues associated with Multiple Neurofibromatosis (Von Recklinghausen's Disease). Cancer 16: 1015-1027.
- D' Agustino AN, Soule EH (1963) Primary malignant neoplasms of nerves (malignant neurilemomas) in patients without manifestations of multiple neurofibromatosis (von Recklinghausen's disease). Cancer 16:1003-14.
- Sordillo PP, Helson L, Hajdu SI, Magill GB, Kosloff C, et al. (1981) Malignant schwannoma--clinical characteristics, survival, and response to therapy. Cancer 47: 2503-2509.
- Feldkamp MM, Lau N, Provias JP, Gutmann DH, Guha A (1996) Acute presentation of a neurogenic sarcoma in a patient with neurofibromatosis type 1: a pathological and molecular explanation. Case report. J Neurosurg 84: 867-873.
- Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, et al. (2007) The 2007 WHO classification of tumours of the central nervous system. ActaNeuropathol 114: 97-109.
- Sørensen SA, Mulvihill JJ, Nielsen A (1986) Long-term follow-up of von Recklinghausen neurofibromatosis. Survival and malignant neoplasms. N Engl J Med 314: 1010-1015.
- Miyakoshi N, Nishikawa Y, Shimada Y, Okada K, Yoshida M, et al. (2007) Intraosseous malignant peripheral nerve sheath tumor with focal epithelioid differentiation of the thoracic spine. Neurol India 55: 64-66.
- Khan RJ, Asgher J, Sohail MT, Chughtai AS (1998) Primary intraosseous malignant peripheral nerve sheath tumor: a case report and review of the literature. Pathology 30: 237-241.
- Hirose T, Scheithauer BW (1998) Perineurial malignant peripheral nerve sheath tumor (MPNST): a clinicopathologic, immunohistochemical, and ultrastructural study of seven cases. Am J SurgPathol 22: 1368-78
- Grobmyer S, Reith JD, Shahlaee A, Bush CH, Hochwald SN (2008) Malignant Peripheral Nerve Sheath Tumor: molecular pathogenesis and current management considerations. J SurgOncol 97: 340-349.
- Fisher CG, Saravanja DD, Dvorak MF, Rampersaud YR, Clarkson PW, et al. (2011) Surgical management of primary bone tumors of the spine: validation of an approach to enhance cure and reduce local recurrence. Spine (Phila Pa 1976) 36: 830-836.
- Kourea HP, Bilsky MH (1998) Subdiaphragmatic and intrathoracicparaspinal malignant peripheral nerve sheath tumors: a clinicopathologic study of 25 patients and 26 tumors. Cancer 82: 2191-203
- Wong WW, Hirose T, Scheithauer BW, Schild SE, Gunderson LL (1998) Malignant peripheral nerve sheath tumor: analysis of treatment outcome. Int J RadiatOncolBiolPhys 42: 351-360.
- Anghileri M, Miceli R (2006) Malignant peripheral nerve sheath tumors: prognostic factors and survival in a series of patients treated at a single institution.Cancer 107: 1065-74
- Dirix LY, Somville J, van Oosterom AT (1996) Diagnosis and treatment of soft tissue sarcomas in adults. CurrOpinOncol 8: 289-298.
- Heslin MJ, Lewis JJ, Nadler E, Newman E, Woodruff JM, et al. (1997) Prognostic factors associated with long-term survival for retroperitoneal sarcoma: implications for management. J ClinOncol 15: 2832-2839.
- Tomita K, Kawahara N, Baba H, Tsuchiya H, Nagata S, et al. (1994) Total en bloc spondylectomy for solitary spinal metastases. IntOrthop 18: 291-298.
- Hsieh PC, Li KW, Sciubba DM, Suk I, Wolinsky JP, et al. (2009) Posterior-only approach for total en bloc spondylectomy for malignant primary spinal neoplasms: anatomic considerations and operative nuances. Neurosurgery 65: 173-181.
Relevant Topics
- 3D Printing in Limb-Sparing Surgery
- Adamantinoma
- Aneurysmal Bone Cysts
- Chondrosarcoma
- Chordomas
- Cryosurgery
- Enchondroma
- Ewing’s Sarcoma
- Fibrous Dysplasia
- Giant Cell Tumor of Bone
- Immunotherapy for Osteosarcoma
- Liquid Biopsy in Orthopedic Oncology
- Malignant Osteoid
- Metastatic Bone Cancer
- Molecular Profiling of Bone Tumors
- Multilobular Tumour of Bone
- Orthopaedic Oncology
- Osteocartilaginous Exostosis
- Osteochondrodysplasia
- Osteoma
- Osteonecrosis
- Osteosarcoma
- Primary Bone Tumors
- Sarcoma
- Secondary Bone Tumours
- Targeted Therapy in Bone Sarcomas
- Tumours of Bone
Recommended Journals
Article Tools
Article Usage
- Total views: 12884
- [From(publication date):
March-2016 - Jan 15, 2025] - Breakdown by view type
- HTML page views : 12119
- PDF downloads : 765