Intraoperative Radiation Exposure of Orthopaedic Surgeons-Mismatch Between Concerns and Protection
Received: 16-Mar-2018 / Accepted Date: 29-Mar-2018 / Published Date: 06-Apr-2018 DOI: 10.4172/2329-6879.1000273
Abstract
Objective: Although orthopaedic surgeons frequently utilize intraoperative imaging, there is a lack of knowledge about their patterns of radiation protection. The goal of this study was thus to fill this gap by evaluating the use of protection against radiation in relation to concerns, safety guidelines and instructions. Methods: A survey addressing the issue was performed in 531 orthopaedic and trauma surgeons. The questionnaire comprised 26 questions concerning the use of intraoperative radiation in clinical practice, concerns about it and protection against.
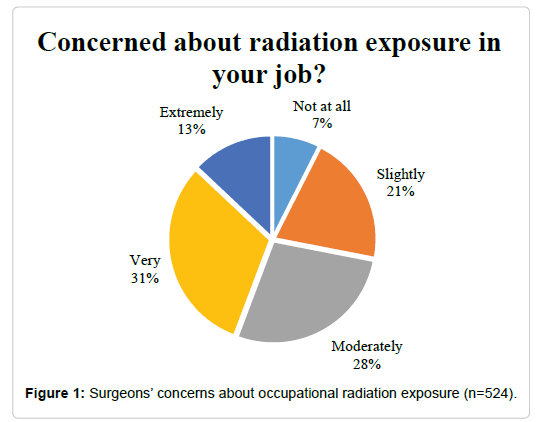
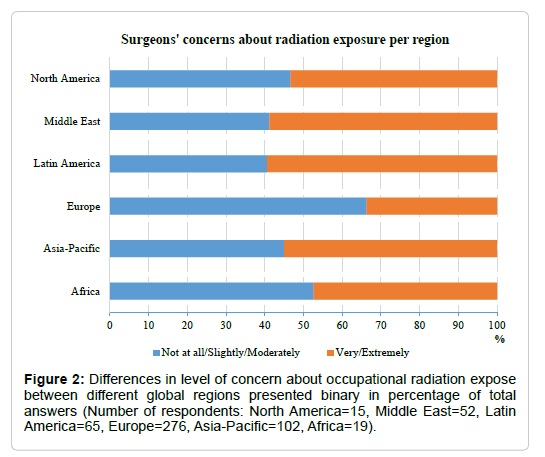
Results: Over 31% of the surgeons are very concerned about their radiation exposure in their job and about 48% are slightly to moderately concerned. Surgeons from Asia-Pacific, Latin America, and Middle East are significantly more concerned about radiation in their job compared to European surgeons (p<0.002). However, only one fifth of the surgeons wear a dosimeter and half of them never use it. Nearly 65% of the surgeons always wear a lead apron, but only 30.8% wear a thyroid protection. Lead gloves and lead glasses were always worn by only 2.5 % (13/531) and 3.1% (16/531) respectively. Half of the respondents are aware of the radiation protection officer in their clinic, but 38.8% stated the issue has never been the subject of training at their institution. Internal training significantly affects the usage of dosimeters (odds ratio=2.97, 95% confidence interval: 2.00 – 4.39; p<0.001).
Conclusion: Although most operating surgeons worry about their exposure, the knowledge and the practical implementation of radiological protection measures in clinical practice is still insufficient. Education is key for better radiation protection in orthopaedic practice.
Keywords: Radiation Protection; Radiation Safety; Radiation Dosimeters; Fluoroscopy; Orthopedic Surgeons; Occupational Health; Operating Rooms
Introduction
Intraoperative imaging using fluoroscopy is increasing in trauma and orthopaedic surgery due to the development of less invasive approaches. This results in an increasing risk for surgeons of being exposed to ionizing radiation, either by scattered radiation or less often in the primary beam [1,2]. Many studies have investigated the radiation doses surgeons are exposed to during different fluoroscopically guided orthopaedic procedures [3-5]. The highest radiation exposures are observed in spinal surgery and intramedullary nailing of long bones [3,4,6]. Especially, the radiation doses to the hands are critical as surgeons often put their hands into the direct beam to position the extremity during fluoroscopy [7]. The level of exposure depends on the surgical technique and experience of the surgeon that influence the duration of imaging [8]. The distance and position of the radiation source play key roles, and also the imaging unit used may have a n impact [1,3].
Ionizing radiation produces a high amount of energy that is absorbed by the tissue leading to direct and indirect effects such as the formation of reactive free radicals, inhibition of cell mitosis, and nucleus damage [9,10]. Within the last decades, an increased risk of cancer has been observed for medical professionals of various specialties exposed to ionizing radiation [11]. It was reported that the incidence of malignant diseases increased among the exposed personnel in an orthopaedic hospital [12] and an increased risk of breast cancer in female orthopaedic surgeons has been detected [13,14].
Methods to reduce radiation exposure in clinical practice are wellknown: increased distance from radiation source, decreased radiation exposure time, shielding and contamination control by monitoring of the equipment [1]. Shielding protection is typically achieved using lead garments such as the lead apron which can attenuate 90% of the radiation with the common thickness of 0.25mm [15]. Attenuation of X-rays can also be achieved for other parts of the body, e.g. 20% by wearing normal glasses, between 30 to 70% by lead glasses, and up to 90% by a thyroid gland shield [16]. Sterile protective gloves have been reported to have a large variation in attenuation properties, reducing the exposure from 7% to 50% [17]. Numerous studies have shown the effectiveness of the lead apron and thyroid collar to reduce radiation exposure [18-20].
Surgeons seem often uninformed about the usage of protection gear leading to unnecessary radiation exposure for both the operating team as well as the patients. A recent study reported that the usage of an apron, a dosimeter and a thyroid shield on a regular basis is observed only in 54% of the operating room personnel [21]. Furthermore, there is an inconsistency in education in medical physics and the occupational prevention of radiation exposure in trauma surgeons and medical technical assistants [2,22]. The goal of the present study was to learn about radiation protection patterns of orthopaedic and trauma surgeons in context with their personal concerns against radiation exposure. By using a targeted survey, availability and use of protective gear as well as policies and surveillance of radiation management at their institution were explored.
Materials And Methods
An interactive questionnaire (Appendix 1) was developed and refined during pilot testing in a group of medical doctors, non-medical scientists and persons with no medical background. Opportunity sampling was used by presenting the questionnaire to trauma and orthopaedic surgeons during international training courses of the AO Foundation in Switzerland. Participation in the survey was voluntarily. Surgeons were asked to provide information about their demographics, subspecialty, professional experience, personal concerns about radiation exposure, use of dosimeter, frequency and time of radiation exposure, position of the radiation source during surgery, and use of protection wear and lead. In addition they should give information regarding radiation safety guidelines at their institution. Multiple answers were allowed for several questions.
The statistical analysis was performed using SAS statistical software (version 9.4 SAS Institute, Cary, NC, USA). A multivariable logistic regression analysis was used to evaluate the association between surgeons' concerns about radiation exposure and (a) region, (b) experience in practicing surgery, (c) workplace, (d) experience in surgeries requiring radiation, and (e) average time of intraoperative radiation. The relationship between the use of dosimeter and the variables (a) region, (b) experience in practicing surgery, (c) workplace, (d) concerns about occupational radiation exposure, (e) instruction on safety guidelines in the hospitals was explored in a second multivariable logistic regression model.
Results
Demographics of respondents
A total of 1898 surgeons participated in the courses, 531 surgeons (19%) answered the questionnaire. 52.2% (276/529) of them worked in Europe. The vast majority, meaning 88.5% (469/530) were between 25 to 54 years old. They mainly worked in a university hospital (49.9%; 265/531) or other hospital (35%; 186/531) and a minority of 12.2% (65/531) in a private practice. 25.7% (136/530) of the surgeons had less than 5 years of experience in practicing surgery. All demographic details are presented in Table 1. 18.8% (100/531) were specialized in the field of the upper extremity, 34.7% (184/531) in the lower extremity, 12.6% (67/531) in pelvic, and 17.5% (93/531) in spine surgery.
| Characteristic | N=531 |
|---|---|
| Gender, n (%) | 529 |
| Female | 52 (9.8) |
| Male | 477 (90.2) |
| Age, n (%) | 530 |
| 18 to 24 | 2 (0.4) |
| 25 to 34 | 154 (29.1) |
| 35 to 44 | 178 (33.6) |
| 45 to 54 | 137 (25.8) |
| 55 to 64 | 50 (9.4) |
| 65 to 74 | 9 (1.7) |
| Region, n (%) | 529 |
| Africa | 19 (3.6) |
| Asia-Pacific | 102 (19.3) |
| Europe | 276 (52.2) |
| Latin America | 65 (12.3) |
| Middle East | 52 (9.8) |
| North America | 15 (2.8) |
| Experience in Practicing Surgery, n (%) | 530 |
| <5 years | 136 (25.7) |
| 5-10 years | 99 (18.7) |
| 11–15 years | 108 (20.4) |
| 16–20 years | 76 (14.3) |
| >20 years | 111 (20.9) |
| Workplace, n (%) | 531 |
| University Hospital | 265 (49.9) |
| Non-University Hospital | 186 (35.0) |
| Private Practice | 65 (12.2) |
| Both University Hospital and Private Practice | 4 (0.8) |
| Both Non-University Hospital And Private Practice | 1 (0.2) |
| Other | 10 (1.9) |
Table 1: Summary of participants’ demographics.
Use of radiation and exposure
77.4% (411/531) of surgeons use a 2D C-arm for intraoperative imaging. Additionally, 14.9% (79/531) of the surgeons work with a 3D C-arm, and 17.3% (92/531) with a mini C-arm. The O-arm and the CT are rarely used by respective 5.8% and 6.0% (31/531; 32/531 respectively). More than half (282/525) of the participants reported the necessity to use intraoperative imaging in 26% to 75% of their surgeries (Table 2). Even 30.3% (159/525) reported to use radiation in over 75% of surgeries. With 38.8% (201/518) of surgeons, the majority used intraoperative imaging for a duration of 61 to 180 seconds. Surgeons worked with an inferior position of the radiation source during most surgeries. 40.1% (209/521) reported to be rarely exposed to the beam during surgery, but 15.9% (83/521) are often directly exposed.
| Characteristics | N=531 |
|---|---|
| What Percentage of the Surgeries You Perform Require Radiation, n (%) | 525 |
| >75% | 159 (30.3) |
| 51%-75% | 164 (31.2) |
| 26%-50% | 118 (22.5) |
| ≤ 25% | 84 (16.0) |
| Average Time of Radiation Use Intraoperatively, n (%) | 518 |
| <30 seconds | 77 (14.9) |
| 30-45 seconds | 72 (13.9) |
| 46-60 seconds | 97 (18.7) |
| 61-180 seconds | 201 (38.8) |
| >180 seconds | 71 (13.7) |
| Main Position of the Radiation Source During Operations, n (%) | 515 |
| Always Inferior | 70 (13.6) |
| Mainly Inferior | 171 (33.2) |
| Equally Inferior/Superior | 86 (16.7) |
| Mainly Superior | 97 (18.8) |
| Always Superior | 17 (3.3) |
| Unknown | 74 (14.4) |
| How Often is a Part of Your Body Directly Exposed to the Beam During Surgery, n (%) | 521 |
| Never, I Always Keep It Out of the Beam | 80 (15.4) |
| Seldom, Only If Unavoidable | 209 (40.1) |
| Sometimes | 124 (23.8) |
| Often | 83 (15.9) |
| Unknown | 25 (4.8) |
Table 2: Frequency and practices of occupational radiation usage.
Concerns about radiation
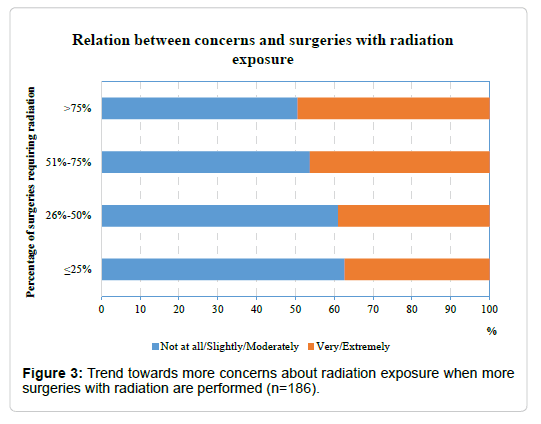
31.3% (164/524) of the surgeons were very concerned about their occupational radiation exposure, and 48.3% (253/524) were slightly to moderately concerned (Figure 1). Concerns about radiation exposure are graphically presented according to region (Figure 2) and participant's experience in surgeries requiring radiation (Figure 3). The results of the multivariable logistic regression model are shown in Table 3. Compared to their European colleagues, surgeons from Asia-Pacific, Latin America and Middle East were significantly more concerned about radiation exposure during their work whereas there was no evidence for a significant difference for surgeons from Africa and North America. Participants with more than 20 years of experience in practicing surgery were almost twice more likely to be concerned about radiation compared to participants with less than 5 years surgical experience (OR=1.90; p=0.026). The workplace, the experience in surgeries requiring radiation, and the average time of intraoperatively used radiation were not found to influence the concerns about occupational radiation exposure.
| Variable | Category | Odds Ratio | 95% CI1 | p value |
|---|---|---|---|---|
| Region | Europe | 1 | - | - |
| Africa | 1.63 | (0.60;4.39) | 0.335 | |
| Asia-Pacific | 2.61 | (1.55;4.40) | <.001 | |
| Latin America | 2.86 | (1.56;5.24) | <.001 | |
| Middle East | 2.82 | (1.48;5.38) | 0.002 | |
| North America | 1.59 | (0.54;4.74) | 0.402 | |
| Experience in Practicing Surgery | <5 years | 1 | - | - |
| 5-10 years | 0.89 | (0.50;1.58) | 0.695 | |
| 11–15 years | 0.97 | (0.54;1.73) | 0.905 | |
| 16–20 years | 1.22 | (0.65;2.29) | 0.532 | |
| >20 years | 1.9 | (1.08;3.34) | 0.026 | |
| Workplace | University Hospital | 1 | - | - |
| Non-University Hospital | 0.67 | (0.44;1.01) | 0.054 | |
| Private Practice/Other | 0.84 | (0.48;1.47) | 0.544 | |
| What Percentage of the Surgeries You Perform Require Radiation | >75% | 1 | - | - |
| 51%-75% | 0.95 | (0.59;1.52) | 0.828 | |
| 26%-50% | 0.68 | (0.40;1.15) | 0.15 | |
| ≤ 25% | 0.56 | (0.31;1.01) | 0.054 | |
| Average Time of Radiation Use Intraoperatively | <61 seconds | 1 | - | - |
| 61-180 seconds | 1.24 | (0.83;1.85) | 0.3 | |
| >180 seconds | 0.69 | (0.38;1.25) | 0.223 | |
| CI1: Confidence Interval | ||||
Table 3: Effect of various factors on the surgeons’ concerns about their occupational radiation exposure (“Extremely/Very concerned” versus “Not at all/ Slightly/Moderately”) using multivariable logistic regression analysis.
Patterns of protection against radiation
Respective 49% and 21% of surgeons reported to wear a dosimeter never (255/520) or always (109/520). Although dosimeters were regularly collected by the hospital in 81.2% of surgeons who wear a dosimeter (216/266), only 56.2% of these surgeons received feedback about the amount of radiation measured by their own dosimeter. The annual radiation dose limit was reached in 12.5% (33/265). Despite this, only 19 surgeons were banned from surgeries using radiation for a certain time period. 64.6% (332/514) of the participants always wear a lead apron, and 30.8% (159/517) always a thyroid collar. Lead gloves and lead glasses were always worn by only 2.5 % (13/517) and 3.1% (16/514) respectively. According to the multivariable logistic regression analysis, region, experience, workplace or concern does not seem to influence the attitude to wear this ionizing radiation measurement device.
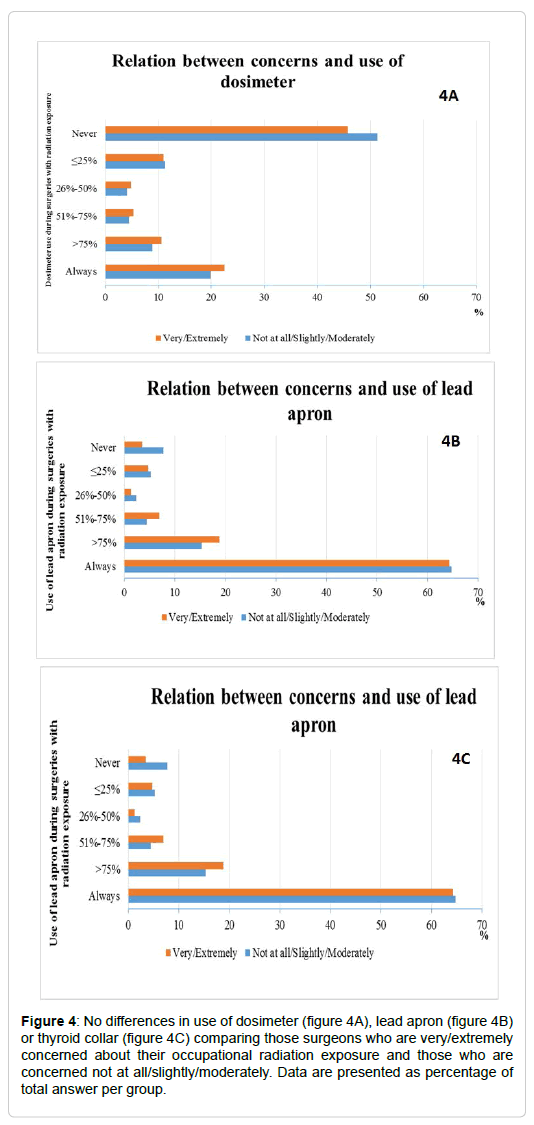
Use of protection in relation to personal concerns and professional experience
Concerns had no influence on the attitude to wear a dosimeter. It is always worn by approximately 23% of the surgeons independent if they rate themselves as being extremely concerned (22.7%; 15/66) or not at all (23.1%; 9/39) (Figure 4a). But if surgeons were extremely concerned, 73.1% (49/67) of them decided to always use an apron compared to 52.6% (20/38) of their colleagues without concerns (Figure 4b). Despite of extreme concerns, the thyroid collar is worn by only 41.8% (28/67) of these surgeons (Figure 4c), and 79.4% and 77.9% of them never wear gloves (54/68) or lead glasses (53/68), respectively. More surgeons with less than 5 years of surgical experience always wear an apron (71.1%; 96/135) and thyroid collar (32.6%; 44/135) compared to surgeons with up to 20 years or more of experience (59.0%; 62/105, and 22.6%; 24/106 respectively).
Figure 4: No differences in use of dosimeter (figure 4A), lead apron (figure 4B) or thyroid collar (figure 4C) comparing those surgeons who are very/extremely concerned about their occupational radiation exposure and those who are concerned not at all/slightly/moderately. Data are presented as percentage of total answer per group.
Use of protection in relation to safety guidelines and instructions
Of surgeons who are aware of safety guidelines at their hospital, the majority (173/244) always uses a lead apron, but only 35.5% (87/245) and 24.5% (60/245) a respective thyroid collar and dosimeter. Even if surgeons did not know whether safety guidelines exist, 66.7% (84/126) of them always wear an apron. In the multivariable analysis, the only factor associated with dosimeter use was the instruction received about safety guidelines in participants' hospital, with those receiving any radiation safety instructions being three times more likely to use dosimeter compared to those with no instruction at all (OR=2.97; 95%CI: 2.00-4.39; p<0.001). Among participants who received adequate radiation safety instructions, an apron and thyroid collar is always used in 76.3% (58/76) and 38.2% (29/76), respectively. If there were none or only limited safety instructions, protective gear was applied less. Being aware of the responsible person for radiation safety leads to an increased use of apron (71.7%; 182/254), thyroid collar (35%; 90/257) and dosimeter (27.7%; 71/256).
Discussion
The answers of our survey confirm the frequent use of intraoperative imaging in orthopaedic surgery. The survey also reveals varying levels of concerns about radiation. Interestingly, these concerns vary between regions and tend to increase with higher use of intraoperative imaging. However, we could not detect any link between higher levels of concerns about radiation and more active patterns of protection against radiation. In other words: there is a mismatch between concern and action. This is surprising because simple measures of radiation protection like thyroid collar or protective apron are capable to reduce radiation exposure significantly.
Our survey also quantified the low regular use of protective apron (64.6%), thyroid collar (30.8%) or dosimeter (21%) in current clinical orthopaedic practice despite availability. Striking to observe that only less than 5% of the surgeons in our survey reported to always wear lead gloves or lead glasses during surgeries; especially considering that the hands of the surgeons are the part of the body with the highest level of exposure [2,7]. The need to manually position the extremity for imaging may contribute to the increased exposures as well as the type of fluoroscopy unit, e.g. mini C-arm or standard C-arm. However, the influence of the fluoroscopy unit is controversially discussed [7,23-25].
In agreement with our results, a recently published survey of consultants, medical students and medical staff from two German hospitals also reported that 84% wear a lead apron, but only 33% and 44% use a respective thyroid shield and dosimeter during more than half of their clinical routine with radiation exposure [21]. These results highlight that improper use of safety gear is a problem affecting surgical staff at large and not only orthopaedic surgeons.
In addition, our survey has shown that nearly half of the participants do not use a dosimeter at all, and of the surgeons who wear it, only 56.2% get feedback about the measured radiation dose. The exact quantification of the individual radiation exposure by personal dosimeter is therefore unreliable and most likely grossly underestimated. Moreover it seems to be of limited value if dosimeters are not under regular control and proper feedback is not provided to the surgeons. A policy that would enforce the surgeons to wear it and report the radiation exposure may increase awareness and potentially result in better protection against radiation exposure. This conclusion is drawn since our survey revealed that the dosimeter is worn significantly more often when the surgeons got at least some instructions about safety guidelines. We also observed a trend of increased use of all available safety protection in case the surgeons were aware of the responsible person for safety guidelines in their institute or got safety instructions. On the one hand, these findings indicate that there may be clear deficits in regular safety instructions, and on the other hand even some instructions have a positive impact. Therefore, the key to better protection against radiation exposure is awareness and education. Measures at hospital level are necessary to reinforce both.
Many studies have shown that the position of the surgeons and of the intraoperative device can reduce the levels of radiation exposure [26,27]. It is suggested that the surgeons should always stand on the detector side if lateral images are required and the X-ray source should be below the table for an anterio-posterior image [28]. Our survey indicates that the radiation source is placed inferior in around half of the surgeries, i.e. the radiation emitting source is positioned under the table and the detector is placed above. However, 22.1% of the surgeons stated that the radiation source is mainly to always placed superior. It is critical that 74 surgeons were not aware of the position of the radiation source at all. Surgeons and the operating team need to be trained about the correct positioning of the image intensifier. Experience and training could lead to a reduction of intra-operative X-ray exposure [8]. Virtual training systems have been shown to give excellent results nowadays [29,30].
The main limitation of the study is that participating doctors are only a sample of voluntary course participants who were interested in improving surgeries and in this survey, and may not be representative for other orthopaedic and trauma surgeons. Also, the irregular distribution of the participants within the regions may have an impact on the results. A randomly selected ideal sample would have added more information because the distribution of surgeons would eventually show more differences. For example, orthopaedic surgeons from the under-represented regions of Africa, Middle-East and Latin America may use different techniques with less fluoroscopy.
In summary, our results show that despite the elevated level of exposure to ionizing radiation and increased levels of concerns about radiation orthopaedic surgeons fail to follow basic safety measures. In order to reduce this work hazard, it is crucial to implement policies to ensure that information about the risks and clear safety guidelines are provided, protection gear and dosimeters are readily available and worn at all times and that appropriate actions are taken when the radiation limits are beyond threshold.
Conclusion
The use of intraoperative radiation nowadays is inevitable, but the level of exposure for surgical staff can be easily decreased if appropriate measures are taken. Information and knowledge seem to have major impact on the use of protective gear and for this reason better education regarding radiation exposure and protection is urgently needed.
Acknowledgement
The authors are grateful to Ursula Saiti and Diarmuid De Faoite from AO Clinical Investigation for setting up the survey. They also want to thank Brigitte Gallo from AO Clinical Investigation for her contributions to the first draft of manuscript. Finally, the financial support from AO Foundation via AO TK Trauma to make this project possible is highly appreciated.
References
- Rehani MM, Ciraj-Bjelac O, Vano E, Miller DL, Walsh S, et al. (2010) ICRP Publication 117. Radiological protection in fluoroscopically guided procedures performed outside the imaging department. Ann ICRP 40: 1-102.
- Singer G (2005) Occupational radiation exposure to the surgeon. J Am Acad Orthop Surg 13: 69-76.
- Matityahu A, Goldhahn S, Joeris A, Richter PH, Gebhard F et al. (2017) The great unknown – A systematic literature review about risk associated with intraoperative imaging during orthopaedic surgeries. Injury 48: 1727-1734.
- Yu E, Khan SN (2014) Does less invasive spine surgery result in increased radiation exposure? A systematic review. Clin Orthop Relat Res 472: 1738-1748.
- Â Kesavachandran CN, Haamann F, Nienhaus A (2012) Radiation exposure of eyes, thyroid gland and hands in orthopaedic staff: a systematic review. Eur J Med Res 17: 28.
- Agarwal A (2011) Radiation risk in orthopedic surgery: Ways to protect yourself and The patient. Operative Techniques Sports Med 19: 220-223.
- Hoffler CE, Ilyas AM (2015) Fluoroscopic radiation exposure: Are we protecting ourselves adequately? J Bone Joint Surg Am 97: 721-725.
- Blattert TR, Fill UA, Kunz E, Panzer W, Weckbach A, et al. (2004) Skill dependence of radiation exposure for the orthopaedic surgeon during interlocking nailing of long-bone shaft fractures: A clinical study. Arch Orthop Trauma Surg 124: 659-664.
- Azzam EI, Jay-Gerin JP, Pain D (2012) Ionizing radiation-induced metabolic oxidative stress and prolonged cell injury. Cancer Lett 327: 48-60.
- Â Stewart FA, Akleyev AV, Hauer-Jensen M, Hendry JH, Kleiman NJ, et al. (2012) ICRP publication 118: ICRP statement on tissue reactions and early and late effects of radiation in normal tissues and organs-threshold doses for tissue reactions in a radiation protection context. Ann ICRP 41:321-322.
- Sigurdson AJ, Doody MM, Rao RS, Freedman DM, Alexander BH, et al (2003) Cancer incidence in the US radiologic technologists health study, 1983-1998. Cancer 97: 3080-3089.
- Mastrangelo G, Fedeli U, Fadda E, Giovanazzi A, Scoizzato L, et al. (2005) Increased cancer risk among surgeons in an orthopaedic hospital. Occup Med (Lond) 55: 498-500.
- Chou LB, Chandran S, Harris AH, Tung J, Butler LM (2012) Increased breast cancer prevalence among female orthopedic surgeons. J Womens Health (Larchmt) 21: 683-689.
- Chou LB, Cox CA, Tung JJ, Harris AH, Brooks-Terrell D, et al. (2010) Prevalence of cancer in female orthopaedic surgeons in the United States. J Bone Joint Surg Am 92:240-244.
- Bushberg JT, Seibert JA, Leidholdt Jr EM, Boone JM (2011) The essential physics of medical imaging. Lippincott Williams & Wilkins, Philadelphia pp 583-632.
- Â Tse V, Lising J, Khadra M, Chiam Q, Nugent R, et al. (1999) Radiation exposure during fluoroscopy: Should we be protecting our thyroids? Aust N Z J Surg 69: 847-848.
- Wagner LK, Mulhern OR (1996) Radiation-attenuating surgical gloves: effects of scatter and secondary electron production. Radiology 200: 45-48.
- Tuohy CJ, Weikert DR, Watson JT, Lee DH (2011) Hand and body radiation exposure with the use of mini C-arm fluoroscopy. J Hand Surg Am 36: 632-638.
- Â B Van der Merwe (2012) Radiation dose to surgeons in theatre. S Afr J Surg 50: 26-29.
- Von Wrangel A, Cederblad A, Rodriguez-Catarino M (2009) Fluoroscopically guided percutaneous vertebroplasty: Assessment of radiation doses and implementation of procedural routines to reduce operator exposure. Acta Radiol 50: 490-496.
- Jentzsch T, Pietsch CM, Stigler B, Ramseier LE, Seifert B, et al. (2015) The compliance with and knowledge about radiation protection in operating room personnel: A cross-sectional study with a questionnaire. Arch Orthop Trauma Surg 135: 1233-1240.
- Oddy MJ, Aldam CH (2006) Ionising radiation exposure to orthopaedic trainees: The effect of sub-specialty training. Ann R Coll Surg Eng 88: 297-301.
- Â Athwal GS, Bueno RA, Wolfe SW (2005) Radiation exposure in hand surgery: Mini versus standard C-arm. J Hand Surg Am 30: 1310-1316.
- Â Giordano BD, Baumhauer JF, Morgan TL, Rechtine GR 2nd (2009) Patient and surgeon radiation exposure: comparison of standard and mini-C-arm fluoroscopy. JBJS 91: 297-304.
- Vosbikian MM, Ilyas AM, Watson DD, Leinberry CF (2014) Radiation exposure to hand surgeons' hands: A practical comparison of large and mini C-Arm fluoroscopy. J Hand Surg Am 39: 1805-1809.
- Dresing K (2011) X-ray in trauma and orthopedic surgery. Physical and biological impact, reasonable use, and radiation protection in the operating room. Oper Orthop Traumatol 23: 70-78.
- Lee K, Lee KM, Park MS, Lee B, Kwon DG, et al. (2012) Measurements of surgeons' exposure to ionizing radiation dose during intraoperative use of C-arm fluoroscopy. Spine (Phila Pa 1976) 37: 1240-1244.
- Â Richter P, Dehner C, Scheiderer B, Gebhard F, Kraus M (2013) Emission of radiation in the orthopaedic operation room: A comprehensive review. OA Musculoskeletal Med 2: 11.
- Â Bott OJ, Teistler M, Duwenkamp C, Wagner M, Marschollek M, et al. (2008) virtX - evaluation of a computer-based training system for mobile C-arm systems in trauma and orthopedic surgery. Methods Inf Med 47: 270-278.
- Bott OJ, Wagner M, Duwenkamp C, Hellrung N, Dresing K (2009) Improving education on C-arm operation and radiation protection with a computer-based training and simulation system. Int J Comput Assist Radiol Surg 4: 399-407.
Citation: Joeris A, Goldhahn S, Kalampoki V, Gebhard F (2018) Intraoperative Radiation Exposure of Orthopaedic Surgeons – Mismatch Between Concerns and Protection. Occup Med Health Aff 6: 273. DOI: 10.4172/2329-6879.1000273
Copyright: © 2018 Joeris A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 6246
- [From(publication date): 0-2018 - Feb 03, 2025]
- Breakdown by view type
- HTML page views: 5477
- PDF downloads: 769