Case Report Open Access
Intramedullary Spinal Cord Metastasis of Bladder Carcinoma: A Case Report
Zümre Arican Alicikus1, Nesrin Dagdelen1*, Ilknur Bilkay Görken1, Tülay Canda2 and Ugur Mungan31Dokuz Eylül University Medical Faculity Department of Radiation Oncology, Balçova- Izmir, Turkey
2Dokuz Eylül University Medical Faculity Department of Pathology, Balçova- Izmir, Turkey
3Dokuz Eylül University Medical Faculity Department of Urology, Balçova- Izmir, Turkey
- *Corresponding Author:
- Nesrin Dagdelen
Dokuz Eylül University Medical Faculity
Department of Radiation Oncology, Balçova- Izmir, Turkey
Tel: (0090) 5056107388
E-mail: nesrin_akt@hotmail.com
Received date: May 20, 2014; Accepted date: June 26, 2014; Published date: June 30, 2014
Citation: Alicikus ZA, Dagdelen N, Görken IB, Canda T, Mungan U (2014) Intramedullary Spinal Cord Metastasis of Bladder Carcinoma: A Case Report. J Palliat Care Med 4:179. doi:10.4172/2165-7386.1000179
Copyright: © 2014 Alicikus ZA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Abstract
Objective: Intramedullary spinal cord metastasis (ISCM) is a rare type of central nervous system involvement of cancer and there are only two cases of bladder cancer's ISCM in literature. This is the third one presenting with an ISCM of bladder cancer, but is the only one presenting without any additional metastases.
Clinical information: A 76-year-old man had radical radiotherapyand adjuvant chemotherapy for bladder cancer four months ago, and was with no evidence of disease. He suffered from sudden severe pain on his neck and progressive weakness of the extremities. The deep tendon reflexes were hypoactive in upper extremities and absent in lower extremities. There was no other neurological deficit. Magnetic resonance imaging scan revealed an enhancing intramedullary lesion at the level of third cervical vertebra with peritumoural edema. Immediately, his corticotherapy was started and subtotal mass resection with laminectomy was performed. The pathological examination showed a metastatic carcinoma of the bladder cancer. Then, he had fractionated external beam radiotherapy to the cervical region with corticotherapy. After two months with a better neurological state, his clinical state worsened and he died of a cardiopulmonary arrest.
Conclusion: There is no consensus on the best therapy, however, it can be well palliated with combination therapy of surgery, irradiation and corticosteroids.
Keywords
Bladder carcinoma; Intramedullary tumour; Spinal cord metastases
Abbreviations
DTR: Deep Tendon Reflexes; H & E: Hematoxylin and Eosin; ISCM: Intramedullary Spinal Cord Metastasis; TE: Time eco; TSE: Turbo Spin Eko; W: Weighted
Introduction
Intramedullary spinal cord metastasis (ISCM) is a rare type of central nervous system involvement of systematic malignant tumours. One to 3.4 percent of spinal cord lesions are metastatic [1-4]. Most of the intramedullary metastases occur primarily from lung cancer while the others originate from breast cancer, malign melanoma, ovarian tumour, Hodgkin’s disease, colorectal carcinoma, thyroid carcinoma and renal cell carcinoma [1,3,5-11]. There is a long list of primary tumours that metastasize to the spinal cord, but ISCM of bladder cancer is documented in only two case reports [3,12]. To our knowledge, this report will be documenting the third case of intramedullary metastasis originating from bladder cancer, however it is the only one presenting without any additional metastases.
Case Report
A 76-year-old man with no comorbid disorders had painless haematuria for 2 months. Initially, he was treated with antibiotics, which was discontinued because of no response. The urinary system ultrasonography showed a thickness (7 mm) in the wall of bladder’s basis and 52×21 mm papillary lesion on the left wall were found. Then, a cystourethroscopy was performed and 50 mm tumour arising from the basis of the bladder and involving the left wall was found. The excisional biopsy showed a high-grade (grade 3) urothelial cell carcinoma invading into muscularis propria and with carcinoma in-situ focuses and, the stage was pathologically T2a. There was no metastasis on thoracoabdominal computerized tomography. As a primary treatment, radical surgery or organ preservation treatment with radical radiotherapy were explained to the patient. As the patient refused surgery, he underwent radical radiotherapy with concomitant cisplatine chemotherapy. After completion of radiochemotherapy, he received 2 cycles of adjuvant chemotherapy. On the follow up period, he had no evidence of disease.
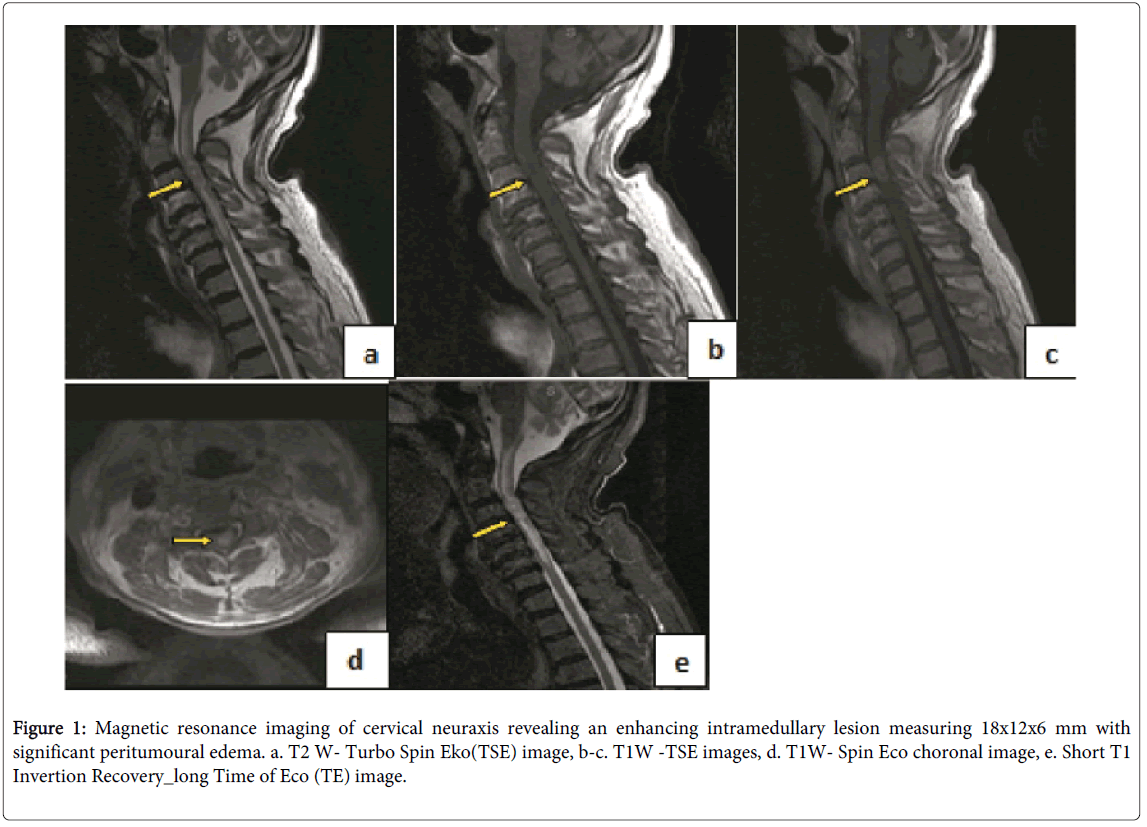
After four months of disease free interval, he had a sudden severe pain on his neck. Afterwards, he started to suffer from weakness of left upper - lower and a week later weakness of right upper - lower extremities. In the physical examination, muscle strength was 1/5 and 1-2/5 on the left side and right side, respectively. The deep tendon reflexes (DTR) were hypoactive in upper extremities and absent in lower extremities. Sensory loss or other neurological deficits were not observed. Magnetic resonance imaging scan of the brain and the whole neuraxis revealed an enhancing intramedullary lesion at T1–T2 weighted images, measuring 18×12×6 mm with significant peritumoural edema (Figure 1). The lesion was at the level of third cervical vertebra. The edema reached to the medulla cranially and to the seventh cervical vertebra caudally. There was no metastasis established in MRI and CT scan of brain and CT scan of thorax and abdomen.
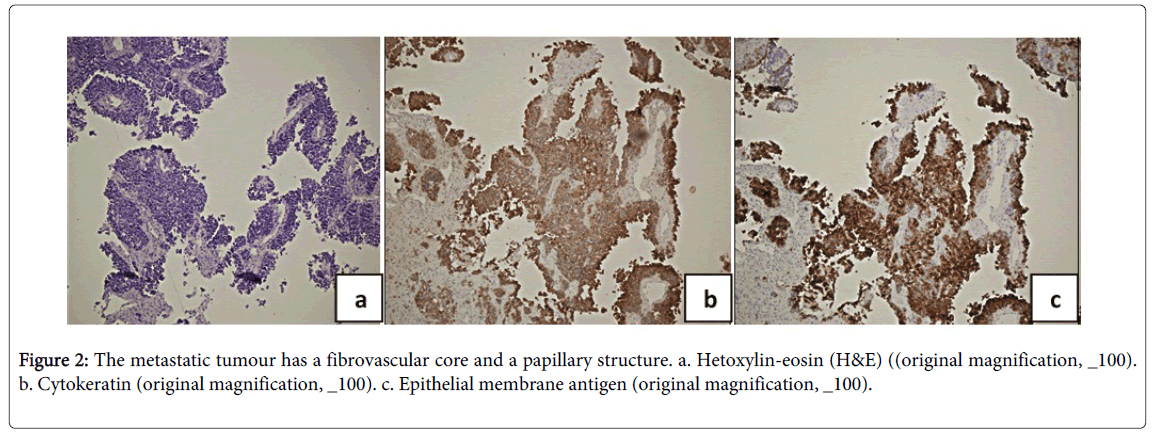
Immediately, corticotherapy (dexamethasone 16 mg/day) was started. Surgical operation was considered as initial treatment because of the rapid progression of the symptoms and to have a histopathological diagnosis. Peroperative pathology was reported as suspectly ependymoma. The subtotal mass resection with laminectomy of the third cervical vertebra was performed. The final pathological examination showed a “metastatic carcinoma”. Due to his previous bladder carcinoma history, immunohistochemical stains were performed. Immunohistochemically, the tumour cells were cytokeratin (+), glial fibrillary acidic protein (GFAP) (-), epithelial membrane antigen (EMA) (+), prostate specific antigen (PSA) (-), prostatic acid phosphatise (PSAP) (-), tyroid transcription factor-1 (TTF-1) (focally +), S-100 (-), Vimentin (-), chromogranin (-), sinaptofizin (-), p63 (focally +). The final pathological diagnosis was reported as metastatic bladder carcinoma (Figure 2).
Figure 1: Magnetic resonance imaging of cervical neuraxis revealing an enhancing intramedullary lesion measuring 18x12x6 mm with significant peritumoural edema. a. T2 W- Turbo Spin Eko(TSE) image, b-c. T1W -TSE images, d. T1W- Spin Eco choronal image, e. Short T1 Invertion Recovery_long Time of Eco (TE) image.
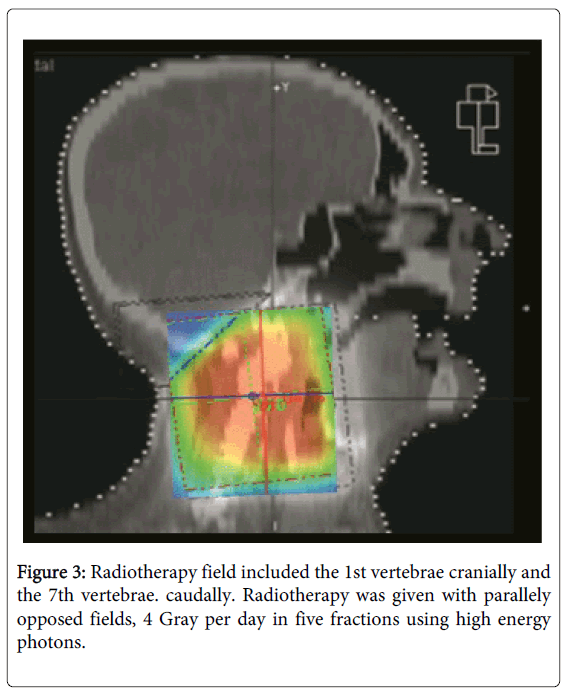
After surgery, he had fractionated external beam radiotherapy to the cervical region combined with corticotherapy. Because of the patient’s demand and his general health condition, a short radiotherapy fractionation schedule was chosen. Radiotherapy was performed with 4 Gray daily fractions in five days (Figure 3). After completion of radiotherapy, he had clinical improvement. Before his discharge from hospital, two months after surgery, the final physical examination showed muscle strength as 3/5, 3/5 and 1/5 in bilateral upper, right lower and left lower limbs, respectively. The DTRs were hypoactive in both upper and lower extremities. As in the initial physical examination, neither sensory loss nor other neurological deficits were detected. The corticotherapy medication was tapered and he was given an exercise program. In the light of general condition of the patient, palliative chemotherapy was not considered.
On the follow up period, two months after the end of radiotherapy, his clinical state worsened gradually and he died of a cardiopulmonary arrest.
Discussion
Intramedullary spinal cord metastasis is an unusual type of cancer metastases. Incidence is reported as 1-3.4 % in the literature [1-4]. The most common primary site is lung accounting for 50-64%, followed by breast carcinoma (15%) [1,8,10,11]. In less than 2% of cases, the primary tumour site is unknown. The most common location of ISCM is the thoracic cord (42%) followed by the cervical cord (31%) [8]. In our patient, the metastasis was located at the cervical cord.
It is rare that the metastasis of central nervous system (CNS) occurs only in the spinal cord. In 50-59% of cases there are concurrent brain metastases [10,12]. However, unlike the other two cases, no brain metastasis was determined in our patient [3,12].
There are many suggested pathogenetic mecanisms for ISCM. The most common one is believed to be hematogenous spread, while the others are dissemination through the vertebral venous plexus and via direct invasion of nerve roots [8,10].
As reported in review of Grem et al., the most frequent presenting complaints are pain and motor deficit [8]. In our patient, pain was the initial symptom and was followed by weakness of the extremities. Sudden onset of neurological deficit and rapid progression are the most consistent characteristics of ISCM and this is helpful in distinguishing it from the slow growing primary spinal intramedullary tumours [8,13]. The distribution of the weakness is asymmetric in most patients with ISCM, as it was in our patient and in one of the two other cases [8,12]. Paresthesia is less frequent as an initial symptom. There was also no sensory deficit in our patient, but both of the other two ISCM of bladder cancer cases had sensory deficits [3,12]. Dysfunction of bowel and bladder are unusual early manifestations of intramedullary spinal cord metastasis. Other common findings include a diminished sensory level, pathological reflexes, and Brown-Séquard's syndrome [1,8,14,15].
In the past, computed tomography myelography was used, but it had false negative findings [11]. As the MRI tecnology improved, MR imaging became the most sensitive and specific test for detection of ISCM [11,14,15]. Nowadays, it is the gold standard method. The use of gadolinium-enhanced MR images has further improved sensitivity, because they make it possible to distinguish metastatic tumour sites from surrounding edema, so it helps the surgeon to localize the sites for surgical planning.T2-weighted MR images are very sensitive in delineating intramedullary lesions. This lesions have greater water content, so they have an abnormal MRI signal as well as the reactive peritumoral edema. An enhancing central metastatic tumor nodule may be demonstrated by additional use of gadolinium. However, there is still no technique that is capable of distinguishing ISCM from primary spinal cord neoplasm or other non-neoplastic lesions [11]. MRI with gadolinium was performed in our patient and the other two cases to determine the ISCM lesion [3,12]. Complete brain and spine imaging, preferably with MRI, as performed in our patient, is important before treatment decisions. MRI is also helpful to evaluate the response to therapy and to discern the presence of multiple metastatic lesions in the neuraxis [1,10,14].
Radiotherapy, chemotherapy and surgery are treatment options for intramedullary spinal cord metastases. However, there is no consensus on which treatment is the best one. Mostly, ISCM is unresectable without causing additional neurological deficits. Due to the fact that these tumors invade the spinal cord, ISCM resection and dissection from normal tissues is difficult. Radiotherapy with or without steroids is accepted as a gold standard in worldwide, especially in patients with early diagnosis and radiosensitive tumours such as lymphoma or oat-cell carcinoma who have long-lasting remission with radiation [1,3,8,14]. In other patients, improvement of their neurological symptoms without increase in survival time is observed. Within 6 months after standard radiation therapy, 80% of patients are paraplegic or dead. Combination of steroids and radiation therapy has no additional survival benefit, but steroids can provide improvement in the symptoms by acutely reducing peritumoral edema [14,16]. Intramedullary spinal cord metastasis is very rare, so that no randomized trials can be established to determine the best radiation dose and the fractionation schedule. In the literature, various treatment schedules were used usually with a total dose of 20 - 40 Gray with conventional techniques [7,16,17]. Parikh and Heron used fractionated radiosurgical treatment for their ISCM of renal cell carcinoma case. They used a dose of 15 Gy to the 80% isodose line in 3 fractions, over 5 days. They concluded that CyberKnife stereotactic radiotherapy was feasible, safe, and efficient to treat a patient with an ISCM [18].
In addition,as the optimal fractionation schedule is unknown, decision of short or long-course radiation therapy scheme depends on many prognostic factors such as, tumour type, patients general health condition and performance status, as well as the frequency of other metastatic sites [19]. Our patient had poor performance status that led us and the patient to choose a short-course radiotherapy. One of the urothelial ISCM cases in the literature had no therapy, and the other one had 10 fractions of irradiation reaching a total dose of 30 Grays [3,12].
Highly radioresistant tumours as well as the well encapsulated or cystic intramedullary spinal cord metastases should be considered for surgical intervention. Cystic tumours are more easily removed without damaging the normal structures [14]. However, surgical decision depends on various factors, such as the comorbidities and general condition of patient, risk of anesthesia and dissemination of the primary malignancy [11,14,17].
Grem et al. suggest that surgery could be useful for establishing the diagnosis, but did not provide neurologic improvement. The best therapeutic results were achieved by radiotherapy [8]. However, a more recent study by Sutter et al,. determined in their case report and literature review that surgery provides improvement in neurological status and survival in patients with ISCM [14]. Due to improvements of surgical techniques, many patients might have benefit from more effective surgical treatment modalities such as radical, open excision, minimally invasive surgery like endoscopy to ultraminimal/noninvasive spinal radiosurgery [6].
Chemotherapy alone is not choice of treatment for ISCM cases, but can be used in combination with other treatment modalitites, especially in chemosensitive tumours like small cell lung cancer [11,12]. Chemotherapy, especially when combined with radiotherapy, has an effect on survival, depending on the chemosensitivity of the tumour [7]. Carboplatin is considered as the most effective agent [7,20].
Providing successful palliation and improving patients’ quality of life requires multidisciplinary strategic treatment planning [6]. Our patient’s treatment started with corticotherapy, and then he underwent surgery. After surgical excision, radiotherapy was performed with tapered continuation of corticotherapy. The case of Crowley et al. was also treated with a multidisciplinary strategy [3].
The survival is usually shorter than 6 months in patients with ISCM, but there are some cases living more, depending on early treatment of metastasis and radiosensitivity of the tumour [1,5,7,8,20]. The survival after radiotherapy was only two months in our patient. Then, his clinical state worsened gradually, but he died of a cardiopulmonary arrest. The short duration of palliation time can be explained with relative radioresistance and incomplete excision of the tumour and the cause of death may be a result of worsened clinical state. Crowley et al had an urothelial ISCM case living only 2 weeks after radiotherapy [3].
There are only two more cases of urothelial ISCM. So this makes it impossible to give a certain message about management of urothelial ISCM. All the three case, including ours, have different managaments, and it is based on the patient’s conditions. So one can only make some general suggestions about urothelial ISCM, concerning that this is a relative radioresistance tumour.
Because the 3/4 of patients have a primary malignancy, aggressive surgical approaches is often not indicated [11]. Radiotherapy is a non-invasive and effective palliative method for this group of patient who have short survival with any treatment method. If the metastases are suspicious or the patient is expected to have a long survival, combined modality treatment should be used.
As a result experience related with ISCM is very limited. However, all findings of our patient were consistent with the literature.
Conclusion
In this case report we present a patient, who was diagnosed and treated for bladder cancer, after a short period of time, he suffered from intramedullary spinal cord metastasis. ISCM resulting from bladder cancer is extremely rare. To our knowledge, our case study is the third documented ISCM case from which the primary site is bladder. The patient underwent surgery and radiotherapy with concomitant corticotherapy which are the most effective palliation methods for patients with intramedullary spinal cord metastasis.
Acknowledgment
We appreciate Merih Güray M.D, Associate Professor of Pathology at the Dokuz Eylül University for the histopathological images and descriptions.
References
- Cordan T, Bekar A, Türeyen K, Dogan S, Tolunay S (1994) Intramedullary Spinal Cord Metastasis: Case Report. Turkish Neurosurgery 4: 171 - 173.
- Costigan DA, Winkelman MD ( 1985) Intramedullary spinal cord metastasis J Neurosurg 62: 227-233.
- Crowley RW, Sherman JH, Le BH, Jane JA Sr. (2008) Intramedullary spinal cord metastasis from bladder carcinoma: Case report. Neurosurgery 63: E611-E612.
- Schiff D, O’Neill BP (1996) Intramedullary spinal cord metastases: Clinical features and treatment outcome. Neurology 47: 906–912.
- Aryan HE, Farin A, Nakaji P, Imbesi SG, Abshire BB (2004) Intramedullary spinal cord metastasis of lung adenocarcinoma presenting as brown-sequard syndrome. Surgical Neurology 61: 72-76.
- Asadi M, Rokni-Yazdi H, Salehinia F, Allameh FS (2009) Metastatic renal cell carcinoma initially presented with an intramedullary spinal cord lesion: a case report. Cases J 2:7805.
- Fakih M, Schiff D, Erlich R, Logan TF (2001) Intramedullary spinal cord metastasis (ISCM) in renal cell carcinoma: a series of six cases. Ann Oncol 12:1173-1177.
- Grem JL, Burgess J, Trump DL (1985) Clinical features and natural history of intramedullary spinal cord metastasis. Cancer 56: 2305-2314.
- Isoya E, Saruhash Y, Katsuura A, Takahashi S, Matsusue Y, et al. (2004) Intramedullary spinal cord metastasis of ovarian tumor. Spinal Cord 42: 485-487.
- Kaya RA, Dalkilic T, Ozer F, Aydin Y (2003) Intramedullary spinal cord metastasis: a rare and devastating complication of cancer--two case reports. Neurol Med Chir (Tokyo) 43: 612-615.
- Sung W-S, Sung M-J, Chan JH, Manion B, Song J, et al. (2013) Intramedullary Spinal Cord Metastases: A 20-Year Institutional Experience with a Comprehensive Literature Review. World Neurosurgery 79: 576-584.
- Abdulazim A, Backhaus M, Stienen MN, Citak M, Brokinkel B, et al. (2011) Intramedullary spinal cord metastasis and multiple brain metastases from urothelial carcinoma. J ClinNeurosci 18: 1405-1407.
- Hrabalek L (2010) Intramedullary Spinal Cord Metastases: Review Of The Literature. Biomed Pap Med FacUnivPalacky Olomouc Czech Repub 154:117–122.
- Sutter B, Arthur A, Laurent J, Chadduck J, Friehs G (1998) Treatment options and time course for intramedullary spinal cord metastasis. Report of three cases and review of the literature. Neurosurg Focus 4:e3.
- Villegas AE, Guthrie TH (2004) Intramedullary Spinal Cord Metastasis in Breast Cancer: Clinical Features, Diagnosis, and Therapeutic Consideration. The Breast Journal 10: 532-535.
- Newton HB, Ray-Chaudhury A, Malkin MG (2008) Chapter 6 - Overview of Pathology and Treatment of Intramedullary Spinal Cord Metastases: Handbook of Neuro-Oncology NeuroImaging. San Diego, Academic Press, 50-53.
- Dam-Hieu P, Seizeur R, Mineo JF, Metges JP, Meriot P, et al. (2009) Retrospective study of 19 patients with intramedullary spinal cord metastasis. ClinNeurolNeurosurg 111: 10-17.
- Parikh S, Heron DE (2009) Fractionated radiosurgical management of intramedullary spinal cord metastasis: A case report and review of the literature. Clinical Neurology and Neurosurgery 111: 858-861.
- Hashii H, Mizumoto M, Kanemoto A, Harada H, Asakura H, et al. (2011) Radiotherapy for patients with symptomatic intramedullary spinal cord metastasis. J Radiat Res 52: 641-645.
- Bakshi A, Biswas G, Deshmukh C, Prasad N, Nair R, et al. (2006) Successful complete regression of isolated intramedullary spinal cord metastases from epithelial ovarian carcinoma with chemotherapy and radiotherapy. Indian J Cancer 43: 136-138.
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 13880
- [From(publication date):
June-2014 - Apr 02, 2025] - Breakdown by view type
- HTML page views : 9383
- PDF downloads : 4497