Intraepiphyseal Osteoid Osteoma of Proximal Tibial Epiphysis Treated by En bloc Excision under CT Guidance: A Case Report
Received: 30-Sep-2021 / Accepted Date: 14-Oct-2021 / Published Date: 21-Oct-2021 DOI: 10.4172/2472-016X.1000155
Abstract
Intra epiphyseal osteoid osteoma is a very rare occurrence with only a few cases reported in literature. They present with nonspecific and atypical clinical features and often have subtle radiographic findings. As the growth plate is open, they can present with features of painful arthritis, further delaying the diagnosis. Serial plain radiographs and further imaging with CT scan forms an essential part of diagnostic work up. We report a case of intra epiphyseal osteoid osteoma, presented with typical findings of osteoid osteoma, but had subtle radiological findings. Hence the diagnosis was delayed but later confirmed with CT scan. As the lesion was very small, en bloc resection was done under CT guidance, which led to complete recovery of the lesion without development of any complications.
Keywords: Intra-epiphyseal, Osteoid osteoma, CT guided en bloc resection
Introduction
Osteoid osteoma is the third most common benign tumour, occurring in the second and third decades of life [1-3]. In majority of cases, they occur in the diaphysis or metaphysis of long bones and present with characteristic dull aching pain, worse at night and relieved by salicylates. Characteristic radiographic features like, the radiolucent nidus with surrounding sclerosis leads to easy diagnosis [2-4]. However, intra epiphyseal or intra-articular location of the lesion can cause atypical presentation and radiographic findings. This leads to delayed diagnosis and treatment [4-8].
We report a case of intra-epiphyseal osteoid osteoma in a 16 year old boy, in whom the diagnosis was made after a delay of almost one year. He had recurrent episodes of pain which was relieved with analgesics and serial X-rays taken 5 months apart did not have any significant findings. Further imaging with plain radiographs and CT correlated MRI led to the diagnosis, later confirmed by histopathological examination. Complete resolution of the lesion was possible with en bloc resection done under CT guidance.
Case Study
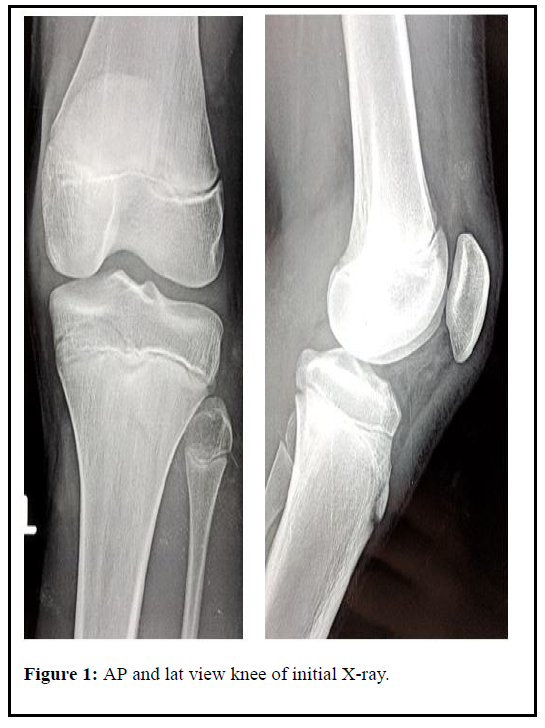
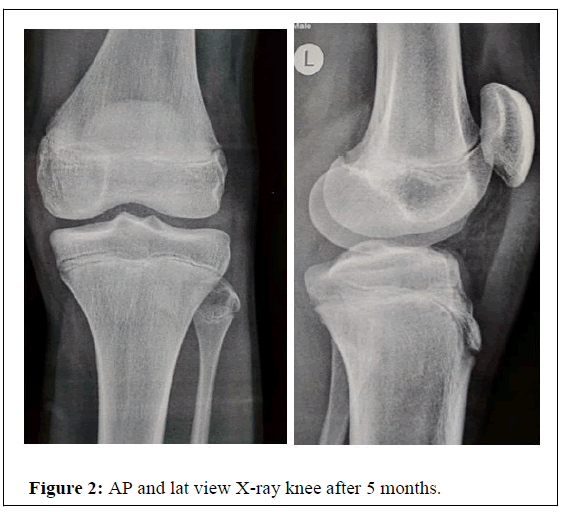
A 16 year old boy presented to our OPD with 11 month history of pain over his proximal third of leg and swelling over the same site for the 3 months. The pain started with an injury to the left leg while playing, which gradually relieved with analgesics. However, he developed recurrent episodes of pain at the same site, with associated night pain, but repeated orthopedic consultations (at various hospitals) failed to reveal any pathological lesion both clinically and radiologically (serial X-rays taken 5 months apart and an MRI) observed in Figures 1 and 2. The swelling and pain gradually increased in severity.
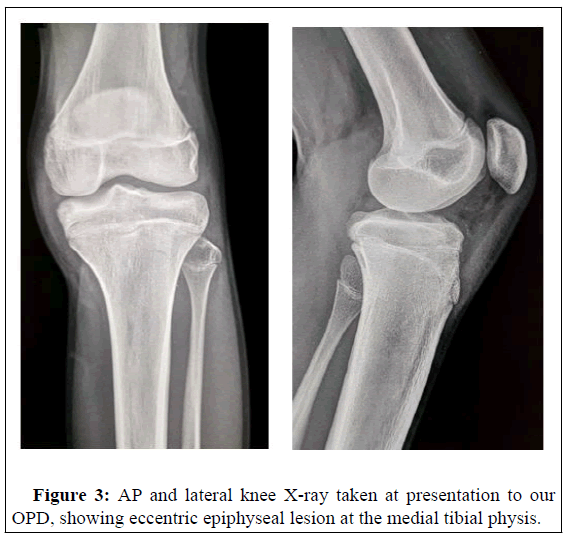
On examination a swelling was palpable on the anteromedial aspect of proximal third of left leg. There was no joint effusion. Active and passive range of motion was full but terminally painful and there was no knee instability. Tenderness was present over the swelling towards the medial joint line area. Inguinal lymph nodes were palpable on the left side. There was no obvious calf and thigh muscle atrophy. Routine blood tests were within normal range. Review of initial plain radiographs taken at the beginning of his symptoms (5 months apart) did not reveal any significant findings. Subsequently, another plain Xray was taken which revealed a tiny eccentric epiphyseal lesion with surrounding sclerosis, collapse of medial tibial plateau and minimal soft tissue shadow in Figure 3.
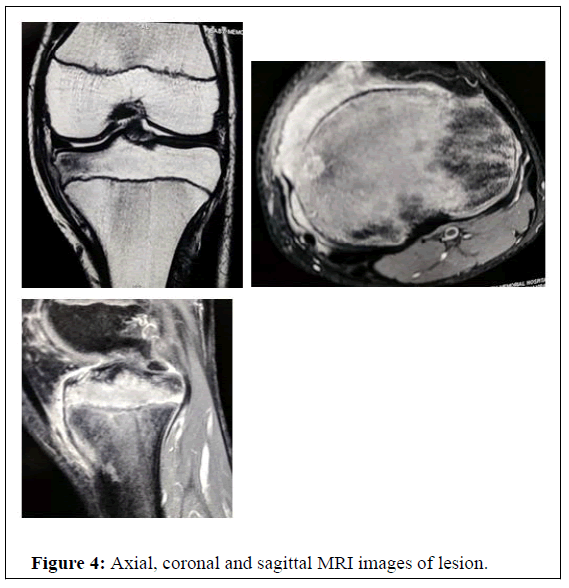
MRI with CT correlation showed bone marrow hyperintensity on STIR and Fat Saturated PD in the medial tibial condyle and intercondylar region involving the epiphysis and medial metaphysis and soft tissue edema deep to MCL and was interpreted as post traumatic bone contusion by the radiologist in Figure 4. Differential diagnosis included early osteomyelitis, osteoid osteoma with bone marrow edema.
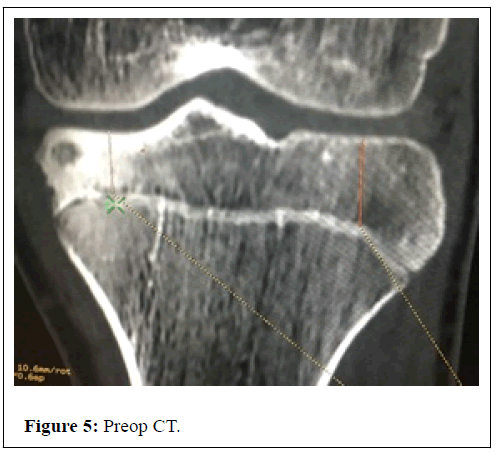
Under local anesthesia and MAC, a CT guided aspiration was done, but the aspirate contained only blood. Hence, an open en bloc excision of the lesion under CT guidance was performed under spinal anaesthesia observed in Figures 5 and 6. The procedure was done with aseptic precautions and with great care without causing damage to the physis or articular cartilage.
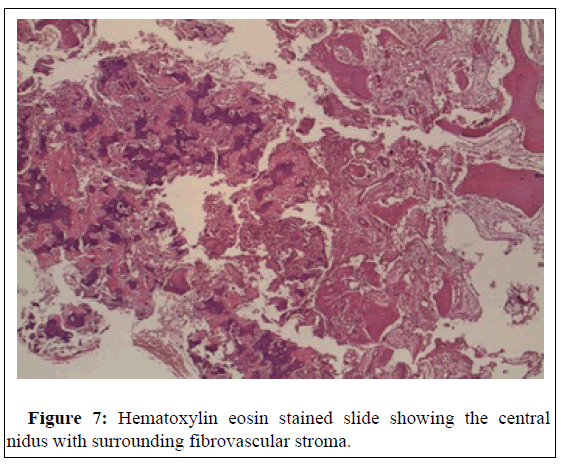
Histopathological examination confirmed the diagnosis of osteoid osteoma shown in Figure 7. The patient was relieved of his symptoms following the procedure.
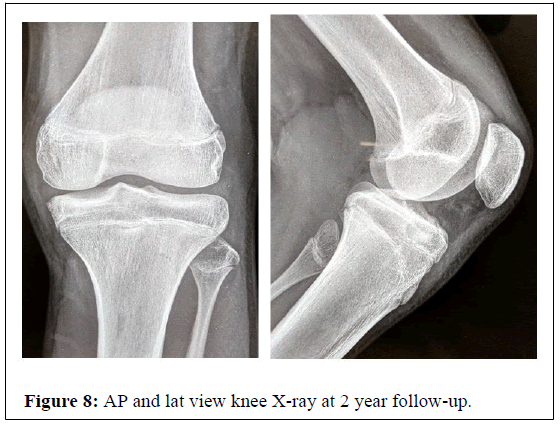
Latest follow up at 2 years after surgery, the child was not having any symptoms or growth disturbance and the plain X-ray showed complete resolution of the lesion in Figure 8.
Results and Discussion
Osteoid osteoma is the third most common benign tumour, accounting for approximately 10% of all benign skeletal tumours. It is commonly seen in the age group 10-30 years, with a male preponderance in the ratio 3:1 [3,9]. Our patient was a 16 year old boy at the time of diagnosis.
The most common site of lesion is in the subperiosteal region of diaphysis of long bones, the femur and tibia being common loci. Approximately 13% of the osteoid osteoma are intra-articular (epiphyseal and intracapsular), the hip joint being the commonest site. The spine and small bones are less commonly affected [5-8,10]. The skull and flat bones are rarely affected.
The most common clinical presentation is pain, a dull unremitting type, initially mild and later increases in severity over time. Worsening of pain at night time is typically seen. However intra articular lesions present with atypical symptoms, including variable articular pain that is difficult to distinguish from other arthropathies. The classic response of pain to salicylates usually seen in osteoid osteoma may be absent in intra articular lesions [1,2]. But features of monoarticular arthritis like synovitis, joint tenderness, effusion, soft tissue swelling can be seen in intra articular osteoid osteoma. This occurs when the nidus communicate with the joint space or growth plate and allows the inflammatory mediators (PGE2, PGI2) to pass through them and produce the symptoms. This can also cause growth disturbances [3]. In our patient there was no communication the joint space, hence synovitis or other features were absent.
The average time to diagnosis is 2-3.5 years and it is possible only through a combination of clinical, radiographic, CT and scintigraphic features [3,5,10]. Clinical symptoms may be present 5-8 months before onset of any typical radiographic findings. The osteoid osteoma appears as a small radiolucent nidus surrounded by sclerotic bone. If less than 3 mm in size, the nidus may be not detected reliably. Periarticular osteopenia may also be seen regionally. In intra articular lesions, where the bone deposition from intracapsular periosteum is less, the nidus may be difficult to detect [9]. The initial radiographs did not detect the lesion in our patient, but it was seen in later radiographs. Hence repeated radiographs may be helpful in uncertain cases.
Double density sign is the typical scintigraphic feature seen in osteoid osteoma, however this may be absent in intra articular lesions [3]. Only focal accumulation of isotope may be seen, in the area corresponding to the nidus. We did not do a scintigraphy as the lesion was intra epiphyseal.
The investigation of choice in diagnosing osteoid osteoma is computed tomography (CT scan) [1,9,10]. Osteoid osteoma appears as a small well demarcated, low attenuated nidus surrounded by dense sclerotic reaction. Foci of calcification may be seen. Presence of fine, linear low density vascular channels that can surround osteoid osteoma has been recently described as a CT finding. Computed tomography with 2-3 mm slice thickness of axial or coronal imaging, reconstructed with bony algorithm is ideal for diagnosis. Accurate preoperative localization has been possible with the use of CT scans and percutaneous ablation under CT guidance is a well-established modality of treatment [10].
Magnetic resonance imaging of osteoid osteoma can mimic an aggressive lesion and hence the interpretation of MRI must be done with reference to plain radiographs and CT scans [11,12].
Histologically the appearance of the nidus is that of well demarcated area consisting of interlacing, irregular bone trabeculae of varying mineralization. A zonal arrangement of trabecular architecture may be demonstrated, with periphery being less mineralized, with more cells and the central part being more sclerotic. The nidus may be surrounded by reactive bone formation with thickened trabeculae and a loose fibrovascular stroma [9,13-15]. Histopathological examination of our patient also showed these features typical of osteoid osteoma.
It has been reported in various studies that if osteoid osteoma is not excised, complete resolution can occur in 6 to 15 years, which can be reduced to 2 to 3 years by administration of NSAID’s [9,16,17].
Well planned surgical approach and good imaging modalities are needed for accurate location of lesion and complete excision, especially in intra epiphyseal lesions. The complete ablation or excision of the nidus causes regression of reactive bone sclerosis and complete resolution of symptoms [18-22].
Conclusion
Intra epiphyseal osteoid osteoma in a skeletally immature individual may present with atypical clinical and radiological features. A high index of suspicion with judicious and meticulous use of imaging modalities can lead to the correct diagnosis. Treatment of intra epiphyseal lesions should be aimed at en bloc excision of the lesion with minimal damage to the physis and articular cartilage, which helps in complete resolution of symptoms without causing any growth disturbances.
References
- Allen SD, Saifuddin A (2003) Imaging of intraarticular osteoid osteoma. Clin Radiol 58: 845-852.
- Georgoulis AD, Papageorgiou CD, Moebius UG, Rossis J (2002) The diagnostic dilemma created by osteoid osteoma that presents as knee pain. Arthroscopy 18: 32-37.
- Baghdadi T, Mortazavi SMJ (2005) Intraepiphyseal oateoid osteoma of proximal tibia epiphysis: a case report. Acta Medica Iranica 43.
- Pogliacomi F, Vaienti E (2003) Misdiagnosed iuxta-articular osteoid osteoma of the calcaneus following an injury. Acta Biomed Ateneo Parmense. 74: 144-150.
- Torg JS, Loughran T, Pavlov H, Schwamm H, Gregg J, et al. (1985) Osteoid osteoma. Distant, periarticular, and subarticular lesions as a cause of knee pain. Sports Med 2: 296-304.
- Sanchis-Alfonso V, Rosello-Sastre E, Castellanos J, Esquerdo J (1994) Intra-articular osteoid osteoma of the humerus with synovitis simulating chronic monoarthritis of the elbow in a recreational tennis player. Knee Surg Sports Traumatol Arthrosc 2: 45-46.
- Cassar-Pullicino VN, McCall IW, Wan S (1992) Intra-articular osteoid osteoma. Clin Radiol 45: 153-160.
- Heuijerjans W, Dandy DJ, Harris D (1986) Arthroscopic excision of an intra-articular osteoid osteoma at the knee. Arthroscopy 2: 215-216.
- Farhad SE, Jacobson JA, John L (2001) Intrarticular osteoid osteoma: sonographic findings in three patients with radiographic, CT, MRI imaging correlation. AJR 177: 1391-1395.
- Beeman PJ, Crowe JE, Sumner TE (1981) Osteoid osteoma of ossification centre of tibia. Skeletal Radiol 7: 71-74.
- Alani WO, Bartal E (1987) Osteoid osteoma of the femoral neck simulating an inflammatory synovitis. Clin Orthop Relat Res 223: 308-312.
- Kattapuram SV, Kushner DC, Phillips WC, Rosenthal DI (1983) Osteoid osteoma: an unusual cause of articular pain. Radiol 147: 383-387.
- Van-Horn JR, Karthaus RP (1989) Epiphyseal osteoid osteoma. Two case reports. Acta Orthop Scand 60: 625-627.
- Destian S, Hernanz-Schulman M, Raskin K, Genieser N, Becker M, et al. (1988) Epiphyseal osteoid osteoma distal end of femur. Skeletal Radiol 17: 141-143.
- Odaka T, Koshino T, Saito T (1987) Intraarticular epiphyseal osteoid osteoma of the distal femur. J Pediatr Orthop 7: 331-333.
- Frassica FJ, Waltrip RL, Sponseller PD, Ma LD, McCarthy EF (1996) Clinicopathologic features and treatment of osteoid osteoma and osteoblastoma in children and adolescents. Orthop Clin North Am 27: 559-574.
- Gitelis S, Schajowicz F (1989) Osteoid osteoma and osteoblastoma. Orthop Clin North Am. 20: 313-325.
- Jaffe H (1935) Osteoid osteoma: a benign osteoblastic tumour composed of osteoid and atypical bone. Arch Surg 31: 709-728.
- Unni KK (1996) Osteoid osteoma. In Uni KK, edn Dahlin’s bone tumours: General aspects and dataon 11.087 cases. 5th edn. Philadelphia. PA: Lippincott Raven Publish pp: 121-130.
- Campanacci M (1999) Osteoid osteoma. In: Campanacci M, ed. Bone and Soft Tissue Tumours. Padova, Italy. Piccin Nuova Libraria SPA pp: 391-414.
- Jaffe HL, Lichtenstein L (1940) Osteoid osteoma: Further experience with this benign tumour of bone. With special reference to cases showing the lesion in relation to shaft cortices and commonly misclassified as instances of sclerosing non suppurative osteomyelitis or cortical bone abscess. J Bone Joint Surg Am 22: 645-682.
- Brody JM, Brower AC, Shannon FB (1992) An unusual epiphyseal osteoid osteoma. AJR Am J Roentgenol 158: 609-611.
Citation: Davis J (2021) Intraepiphyseal Osteoid Osteoma of Proximal Tibial Epiphysis Treated by En bloc Excision under CT Guidance: A Case Report. J Orthop Oncol 7:155. DOI: 10.4172/2472-016X.1000155
Copyright: © 2021 Davis J. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2674
- [From(publication date): 0-2021 - Nov 14, 2025]
- Breakdown by view type
- HTML page views: 1990
- PDF downloads: 684