Case Report Open Access
Intradural Extramedullary Schwannoma of the Thoracic Spine with Intratumoral Haemorrhage
Drevelegas K1, Bangeas P1, Moumtzouoglou A1, Karagiannidis A2, Zaramboukas T3 and Drevelegas A1*1Department of Neuroradiology, Interbalkan Medical Center, Thessaloniki, Greece
2Department of Neurosurgery, Interbalkan Medical Center, Thessaloniki, Greece
3Department of Pathology, Interbalkan Medical Center, Thessaloniki, Greece
- *Corresponding Author:
- Antonios Drevelegas
Radiology Department, Interbalkan Medical Centre
57001, Pylaia, Thessaloniki, Greece
Tel: +302310400213
E-mail: adrevelegas@gmail.com
Received date: August 21, 2017; Accepted date: August 28, 2017; Published date: August 31, 2017
Citation: Drevelegas K, Bangeas P, Moumtzouoglou A, Karagiannidis A, Zaramboukas T, et al. (2017) Intradural Extramedullary Schwannoma of the Thoracic Spine with Intratumoral Haemorrhage. OMICS J Radiol 6:272. doi: 10.4172/2167-7964.1000272
Copyright: © 2017 Drevelegas K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Radiology
Abstract
Schwannomas are the commonest intradural extramedullary tumors of the spine, mostly present in the cervical and lumbar regions. Spinal schwannomas with intratumoral haemorrhage are very rare lesions. Authors here present a 40-year’s old male with a 2 year history of pain in the thoracic region and acute onset of spastic paraparesis and cauda equina syndrome. Magnetic Resonance Imaging (MRI) of his thoracic spine demonstrated a heterogeneous intradural extramedullary lesion with no associated enhancement. After emergent removal of the mass, histopathology revealed schwannoma with intratumoral haemorrhage.
Keywords
Spinal tumors; Schwannoma; Haemorrhage; MRI
Introduction
Spinal schwannomas are schwannomas arising from nerves within the spinal canal. They are the most common intradural extramedullary spinal tumors representing 30% of such lesions followed by meningiomas (25% cases) [1]. They are most commonly located in cervical and lumbar regions because of the higher density of nerve roots at that regions [2,3]. Haemorrhagic spinal schwannomas are usually presented with motor symptoms as well as with pain, numbness and paresthesias. Until present, only 11 cases of haemorrhagic schwannomas have been described in the international literature.
We report a case of a thoracic intradural extramedullary schwannoma with acute intratumoral haemorrhage in an adult male patient who had sudden onset of monoplegia of the right lower extremity and paraparesis of the left.
Case Report
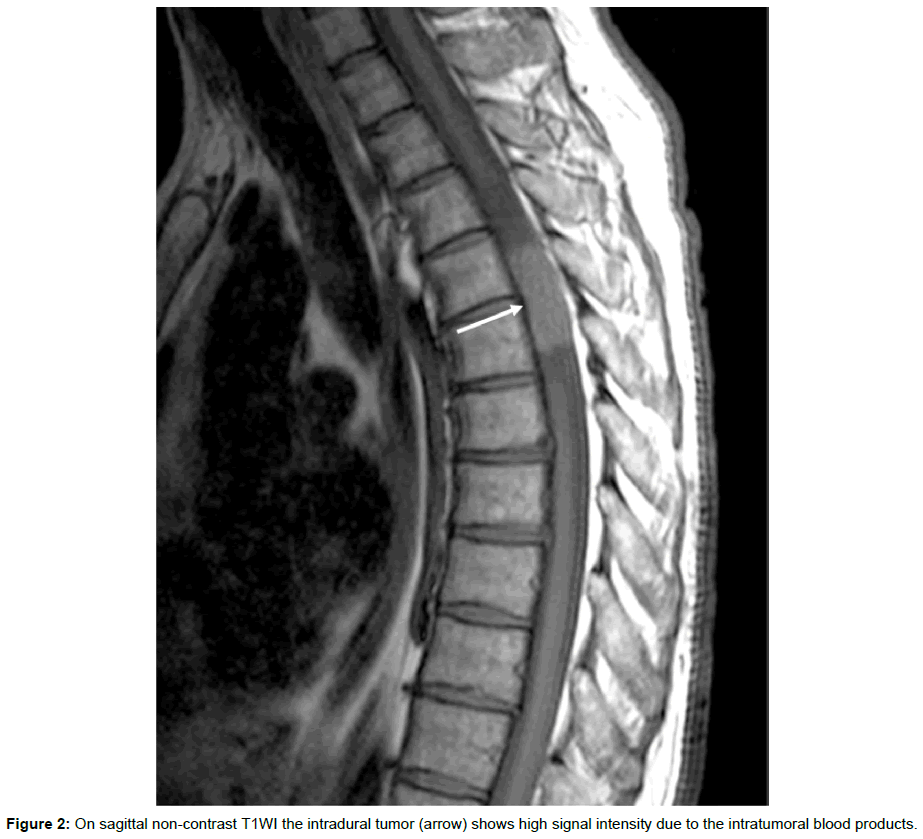
40-years old male patients with symptoms of thoracic spine ache since 2 years ago. He presented to the emergency department of our hospital with increasing pain and numbness of bilateral lower limbs and associated symptoms of cauda equina syndrome within the last 24 h. Neurologic examination revealed bilateral babinski sign and very brisk tendon reflexes. Severe muscle weakness of the left rectus femoris, quadriceps and anterior tibial muscles as well as of the right foot muscles on the motor examination also noted. MRI examination of the thoracic spine demonstrated an intradural mass lesion in the right lateral aspect of the intradural compartment at the level T4-T5 displacing the spinal cord to the left side (Figure 1). The tumor showed high signal intensity on non-contrast T1WI consistent with blood degrading products (Figure 2). After intravenous contrast administration, no evidence of abnormal enhancement pattern presents (Figure 3).
The patient was operated on emergency. Under general anesthesia, posterior laminectomy from T4 to T5 performed. A “chocolate” colored vascularized mass with a surrounding capsule and associated displacement of the regional spinal cord to the left and ventrally was identified and enbloc removed (Figure 4). Consequently, it was sent to the pathologic department for histopathologic correlation. Wound closure was performed in layers and the patient was transferred to the intensive care unit for recovery. Post-operative period was uneventful. The patient presented promptly significant clinical improvement and managed to become ambulant with support in 5 days.
In histological examination, a spindle cell tumor was observed. The tumor cells had elongated normal nuclei without atypia or mitoses and fascicular or storiform arrangement. Extensive haemorrhagic infiltration was observed, but no necrosis (Figure 5A). Immunohistochemically the tumor cells were positive for S100 protein (Figure 5B). According to the previously described features, the diagnosis of a schwannoma was documented.
Discussion
Schwannomas are benign encapsulated neoplasms of Schwann cells (WHO grade I). They arise eccentrically from their parent nerve. They are composed of spindle cells of types: Antoni A and Antoni B [3,4]. In the Antoni A pattern of growth, elongated cells with cytoplasmic processes are arranged in fascicles in areas of moderate to high cytoplasmic ratio with little stromal matrix; acellular areas lie between opposing rows of parallel nuclei (Verocay bodies). In the Antoni B pattern of growth, the tumour is less densely cellular with meshwork of cells along with microcysts and myxoid changes [1].
Patients commonly present with segmental pain. As spinal schwannomas usually arise from the dorsal sensory roots, radicular sensory changes also occur. Weakness is less common. Myelopathy may occur if the lesion is large.
MRI is the examination of choice in the diagnosis of spinal tumors. Typical schwannomas are iso- or hypointense on T1-weighted image, markedly hyperintense on T2-weighted sequence and shows intense homogeneous enhancement in post contrast study [5]. Sometimes they are inhomogeneous on T2-weighted images with hyperintense and hypointense areas due to cyst formation, hemorrhage or dense collagen deposition [6].
Haemorrhagic schwannomas show variable signal intensity on MRI depending on the ages of blood product. In acute haemorrhage the tumor is isointense on T1WI and hypointense on T2WI, in early subacute hemorrhage, as in our patient, hyperintense on T1WI and hypointense on T2WI. In late subacute hemorrhage appears hyperintense on T1/ T2WI and hypointense on T1/T2WI in chronic haemorrhage [7].
Two main theories have been proposed for the occurrence of tumoral haemorrhage. According to the vascular theory, there occurs spontaneous thrombosis of hyalinised tumor vessels with resultant distal tumor necrosis and secondary bleed or alternately, vascular tumors may get obliterated by endothelial proliferation with recanalization resulting in haemorrhage. The second one, mechanical theory, postulates that movements of spine induce traction on tumor vessels resulting in haemorrhage and this usually occur in thoracolumbar lesions [8-10]. Other postulates of haemorrhage (including subarachnoid space) include central ischemic necrosis due to tumor growth or malignant transformation with neovascularisation [9,11]. In our case, because of the absence of prior clinical manifestations and occurrence of symptoms after a minor trauma, we speculate that the latter theory would be more suitable. This is due to its location in the cervico-thoracic region wherein, probably because of the increased mobility of this segment compared to the thoraco-lumbar ones noted in most other cases, haemorrhage would have occurred.
Conclusion
Intradural extramedullary schwannoma with intratumoral haemorrhage is a very rare occurrence. MRI represents the examination of choice in the diagnosis of an intradural extramedullary tumor with spontaneous haemorrhage. Patients with acute paraplegia from a haemorrhagic spinal tumor are considered as neurosurgical emergency. Urgent tumor resection represents the treatment of choice [12].
Conflict of Interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
References
- Abul-Kasim K, Thurnher MM, McKeever P, Sundgren PC (2008) Intradural spinal tumors: current classification and MRI features. Neuroradiology 50: 301-314.
- Ciappetta P, D'urso PI, Colamaria A (2008) Giant craniovertebral junction hemorrhagic schwannoma: case report. Neurosurgery 62: E1166-E1166.
- Conti P, Pansini G, Mouchaty H, Capuano C, Conti R (2004) Spinal neurinomas: retrospective analysis and long-term outcome of 179 consecutively operated cases and review of the literature. Surg Neurol 61: 34-43.
- Kumar V, Abbas AK, Fausto N, Mitchell R (2007) Disease of peripheral nervous system. In: Kumar V (ed.) Robbins Basic Pathology (8th edn.). Philadelphia: Saunders Elsevier p: 899.
- Skolnik AD, Loevner LA, Sampathu DM, Newman JG, Lee JY, et al. (2016) Cranial nerve schwannomas: diagnostic imaging approach. Radiographics 36: 1463-1477.
- Pawha P, Sze G (2009) Neoplastic disease of the spine and spinal cord. In: Scott W (ed.) Magnetic Resonance Imaging of the Brain and Spine (4th edn.). Philadelphia: Lippincott Williams & Wilkins, p: 1538.
- Friedman DP, Tartaglino LM, Flanders AE (1992) Intradural schwannomas of the spine: MR findings with emphasis on contrast-enhancement characteristics. AJR 158: 1347-1350.
- Atlas SW, Thulborn KR (2009) Intracranial Hemorrhage. In: Atlas SW (ed.) Magnetic Resonance Imaging of the Brain and Spine (4th edn.). Philadelphia: Lippincott Williams & Wilkins, p: 657.
- Ng PY (2001) Schwannoma of the cervical spine presenting with acute haemorrhage. J Clin Neurosci 8: 277-278.
- Parmar H, Pang BC, Lim CT, Chng SM, Tan KK (2004) Spinal schwannoma with acute subarachnoid hemorrhage: a diagnostic challenge. Am J Neurorad 25: 846-850.
- Cordan T, Bekar A, Yaman O, Tolunay Ş (1999) Spinal subarachnoid hemorrhage attributable to schwannoma of the cauda equina. Surg Neurol 51: 373-375.
- Parmar H, Patkar D, Gadani S, Shah J (2001) Cystic lumbar nerve sheath tumours: MRI features in five patients. J Med Imag Rad Oncol 45: 123-127.
Relevant Topics
- Abdominal Radiology
- AI in Radiology
- Breast Imaging
- Cardiovascular Radiology
- Chest Radiology
- Clinical Radiology
- CT Imaging
- Diagnostic Radiology
- Emergency Radiology
- Fluoroscopy Radiology
- General Radiology
- Genitourinary Radiology
- Interventional Radiology Techniques
- Mammography
- Minimal Invasive surgery
- Musculoskeletal Radiology
- Neuroradiology
- Neuroradiology Advances
- Oral and Maxillofacial Radiology
- Radiography
- Radiology Imaging
- Surgical Radiology
- Tele Radiology
- Therapeutic Radiology
Recommended Journals
Article Tools
Article Usage
- Total views: 4888
- [From(publication date):
August-2017 - Mar 29, 2025] - Breakdown by view type
- HTML page views : 4065
- PDF downloads : 823