Research Article Open Access
Intervertebral Disc Prolapse: Comparison between Two Manual Techniques
Tanushree Neral, Monalisa Pattnaik and Patitapaban Mohanty*Department of Physical Therapy, Swami Vivekanand National Institute of Rehabilitation Training and Research, Cuttack, India
- *Corresponding Author:
- Patitapaban Mohanty, Ph. D
Associate Professor, Department of Physical Therapy
Swami Vivekanand National Institute of Rehabilitation Training and Research
Olatpur, Bairoi, Cuttack, India
Tel: +91-9437487139
Fax: +91-671-2805862
E-mail: ppmphysio@rediffmail.com
Received date: June 03, 2016; Accepted date: July 12, 2016; Published date: July 22, 2016
Citation: Neral T, Pattnaik M, Mohanty P (2016) Intervertebral Disc Prolapse: Comparison between Two Manual Techniques. J Nov Physiother S3:010. doi:10.4172/2165-7025.S3-010
Copyright: © 2016 Neral T, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Novel Physiotherapies
Abstract
Background: Low Back pain is one of the most common medical problems and lumbar disc prolapse is estimated to account for approximately 37% of cases of low back pain. Purpose: To compare McKenzie repeated extension and Cyriax concept in intervertebral disc prolapse. Method: 30 subjects with acute or subacute low back pain were recruited and randomly divided into two groups. Group I received McKenzie listing correction followed by repeated extension exercises and Extension Mobilization. Group II received Cyriax listing correction followed by Traction. Total duration of treatment was 2 weeks i.e., 5 days/ week. Results: Both the groups showed reduction in pain and improvement in ROM over time but there was no significant difference between the 2 groups. Conclusion: The study suggests that both McKenzie and Cyriax approaches are effective without significant difference between them in managing low back pain, function and range of motion of lumbar spine in patients with Prolapsed Intervertebral Disc.
Keywords
Low Back pain; Lumbar spine; Iliac spines; Muscle tension; Sciatic nerve; Intervertebral disc
Introduction
Low Back pain is one of the most common medical problems that cause a significant amount of disability and incapability. Being the most common structure to be affected, the intervertebral disc is prevalent source of low back pain. The main feature of back pain is pain in the lumbar region, often accompanied by restriction in range of motion and functional limitations.
Lumbar disc prolapse is estimated to account for approximately 37% of cases of low back pain. Back pain and its related disability cause an important socioeconomic burden to society [1]. It is a significant cause of time off work [2].
Over the last decades there has been increasing evidence of links between manual therapy and its effect on acute low back pain due to prolapsed intervertebral disc.
McKenzie developed a system of assessment and treatment for back pain based on symptom response to spinal loading [3]. According to McKenzie, the structures will be a source of constant pain until the stress is removed either by reduction of the derangement or by an adaptive lengthening. A main parameter of evaluation is observing for centralization or peripheralization of the symptoms where centralization has shown to be a strong predictor for positive outcome of conservative care [3]. Within session changes are presumed to occur and several studies also have confirmed that immediate changes do occur following manual therapy of the lumbar spine.
James Cyriax popularized lumbar traction during the 1950s and 1960s as a treatment for disc protrusions. Cyriax described three beneficial effects of traction
1. Distraction to increase the intervertebral space.
2. Tensing of the posterior longitudinal ligament to exert centripetal force at the back of the joint.
3. Suction to draw the protrusion toward the center of the joint [4]. Interesting effects of using traction in reducing the herniated nuclear material and low back pain have been reported in literatures.
However, while numerous studies have looked at the effects of McKenzie extension and Cyriax concept on symptom relief, to date no work has specifically compared both of the treatments. This provided the focus for the present work.
Methodology
Design
Experimental Pre test – Post test comparative analysis design.
Sample
30 subjects (19 males and 11 females), (age range 18-50 years) with acute or subacute low back pain were recruited.
Inclusion criteria
Patient diagnosed as low back pain due to prolapsed intervertebral disc in the Magnetic Resonance Image (MRI), presence of dermatomal pain distribution radiating below knee or leg characterized by unilateral radiculopathy and obliterated lumbar lordosis, acute or subacute, i.e. low back pain less than 12 weeks of duration or recurrent episodes of pain, positive straight leg raise, patient’s symptoms centralizing with repeated extension movements.
Exclusion criteria
Contraindications to manual therapy.
Sampling
Random.
Outcome Measures
Pain by VAS: Horizontal visual analog scale (VAS) was used. It is shown to be valid and sensitive [5,6] and has a reasonable degree of reproducibility [7].
Functional outcome measure by Oswestry disability index: It is composed of 10 sections (containing 10 functional activities). Each section has got 6 options, with scoring from 0-5. Patient had to mark in only one box that applies to them.
This test has been shown to be reliable, valid and responsive functional outcome measure for evaluation of patients with low back pain with associated problems [8].
Range of motion: Modified schober test: With the subject in relaxed standing, mark was made at the level of the bisector of the line running between the left and the right posterior superior iliac spines and another mark was made on the spine 15 cm directly above the first and distance between both the marks were measured.
The difference between the measurements in erect and flexion positions indicates the outcome of the lumbar flexion whereas the difference between the measurements in erect and extension positions indicates the outcome of the lumbar extension.
Procedure
After approval from ethical committee, the subjects fulfilling the inclusion and exclusion criteria were recruited and assigned randomly into 2 groups. All participants underwent an initial baseline assessment of lumbar range of motion, Visual analogue scale and Oswestry Disability Index.
The intervention period was of 2 weeks, for 5 days/week. At the completion of 2 weeks all participants received a follow-up assessment.
Group I received McKenzie listing correction followed by Extension exercises and Extension Mobilization.
McKenzie listing correction - Apply 10 - 15 rhythmical side gliding pressures.
Lying prone in extension - Maintain the position for 5 - 10 minutes.
Extension in lying - Repeat the exercise 10 times.
Extension mobilization - Rhythmically repeat to same segment 10 times.
Group II subjects received Cyriax listing correction followed by traction.
Cyriax listing correction - Re-apply 8 -10 times.
Traction was applied in prone or supine according to degree of pain or limitation of lumbar movements. Continuous traction with 40%-50% of body weight is applied for 10 minutes.
Data analysis
The data was analyzed by using 2×2 ANOVA, where there was one between factor with two levels (Group – McKenzie and Cyriax) and one within factor (Time - pre and post). Pair wise post HOC comparisons were done using Tukey’s HSD using a 0.05 level of significance.
Results
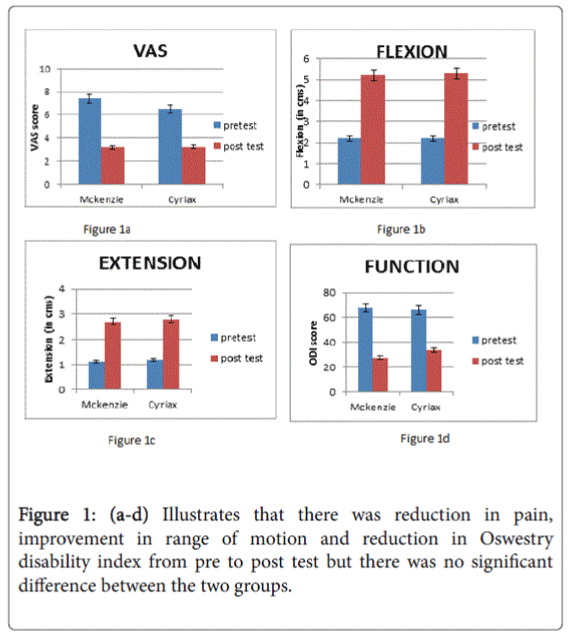
There was a main effect for the time but the main effect for the group did not achieve significant level. This main effect did not attain significance for the group × time interaction for all outcomes (Table 1 and Figures 1a-1d).
| Dependent variable | Effect for Time | Effect for Group | Group x Time interaction | |
|---|---|---|---|---|
| Pain (VAS) | F(1,28,0.05)=297.654, P = 0.000 |
F(1,28,0.05)= 1.493, P = 0.232 |
F(1,28,0.05)=4.651, P = 0.052. |
|
| ROM | Flexion | F(1,28,0.05)=673.273 P=0.000 |
F(1,28,0.05)=0.384, P=0.541 |
F(1,28,0.05)=0.766, P=0.389 |
| Â Extension | F(1,28,0.05)=233.739 P=.000 |
F(1,28,0.05)=0.150, P=0.701 |
F(1,28,0.05)=0.766, P=0.389 |
|
| Oswestry Disability | F(1,28,0.05)=293.528 P=0.000 |
F(1,28,0.05)=1.034, P=0.318 |
F(1,28,0.05)=3.130, P=0.088 |
|
Table 1: Main effect for the time.
Discussion
Pain (VAS)
In the present study both the groups showed reduction in pain over time but after completion of treatment there was no significant difference between the 2 groups. The mechanical stimulation of the posterior annulus of the lumbar intervertebral disc can reproduce the symptoms of the patients with severe back pain.
At least the outer third of the annulus fibrosus is innervated and there are evidences that in painful and degenerated discs, the innervation is more extensive. Internally displaced disc tissue, perhaps a precursor to full herniation, may press directly on the painful outer annulus and thereby give rise to back pain [9].
Robertson et al. described that the pain worsening with movements may be related to an increase in mechanical noxious stimuli on the posterior annulus and the nerve root, resulting from both annular tension and posterior migration of nuclear contents resulting from antero-posterior pressure gradient set up across the disc by anterior loading that occurs with lumbar flexion [10].
Significant improvement in back pain were found in present study in McKenzie group that reduced by 62.8%. The reduction in VAS seen in this group may be explained by its neurophysiological and mechanical effects.
Reduction in pain may be attributed to the fact that, repeated movements of spinal column, caused “Centralization”, where radiating symptoms originating from the spine and referred distally, are caused to move proximally towards the midline of the spine, and thus is utilized to reverse the internal derangement of the disc as long as the integrity of the disc wall is maintained, causing centralization, and pain relief.
By McKenzie extension, an offset load applied to the disc in symptom specific direction of spinal bending, applies a reductive force or load onto displaced nuclear content, redirecting it back towards its more physiologic central location. The symptom generating annulus or nerve roots are mechanically decompressed, resulting in a lessening of nociceptive stimuli and centralization of pain [11]. Extension movements may relieve pain by reducing the forces acting on pain sensitive tissues. It acts to transfer compressive forces from the disc – vertebral body unit to apophyseal joints which lies posterior to them, so that, the nucleus pressure is reduced. Also, repeated extension movements increase the height of the spine presumaly by unloading the disc and permitting rehydration [12].
A provocative case report by April et al. supports the above findings of rapid reversal of pain and full recovery in patients of prolapsed intervertebral disc with a sciatic list using McKenzie’s directional preference of repeated extension exercise [11].
Pain is also an emotional disturbance, which has some psychological influence too [13]. Manual therapy exerts a psychological influence on pain perception of the patient. Stress, muscle tension and pain are interrelated. Clinicians by prescribing McKenzie approach helps to reassure patients that their pain is largely due to factors which are potentially controllable, and has strong psychological effects on patients [14].
The reduction in pain seen in the Cyriax group may be possibly be attributed to the fact that traction following correction of lateral shift reduces pain by relieving pressure on the dorsal root ganglion or mechanically stimulating large diameter nerve fibres, thereby silencing ectopic discharges. Improved nerve conduction could result from improved blood flow or alleviation of mechanical compression resulting from herniation [15]. Theories on the physiologic effects of traction suggest that stimulation of proprioceptive receptors in vertebral ligaments and mono-segmental muscles may alter or inhibit abnormal neural input from those structures [16].
Traction is beneficial for relieving pain by its mechanism that it helps in extending and mobilizing the soft tissue of the back, decompressing the intervertebral discs and releasing pressure on trapped nerve, releasing muscle spasm by distraction and reduces hydrostatic pressure in the discs [17].
Range of motion (ROM)
There was significant improvement in Range of motion of lumbar spine in both the groups at the end of the study. However, there was no significant difference between the two groups.
Sustained and repeated flexion of lumbar spine stresses the nucleus posteriorly. This coincides with a rising of intradiscal pressure and increased tangential stress on posterolateral disc wall, as it is the weakest part of annular wall, having least radius, is thinner and least firmly attached to bone [18].
Obstruction to extension range of motion of lumbar spine may be caused by excessive postero-lateral displacement or accumulation of fluid nucleus, thus the displacement locks the patient in the position of LIST [19] and narrowing of spinal canal [20]. Thus with extension movement patient experiences more pain as there is more compression of the nerve within the spinal canal resulting in limitation of range of motion.
Laslett hypothesized that a contralateral shift is caused by space occupying disc herniation pushing the trunk away from the painful side, forcing the vertebrae apart so, the posterior margins cannot approximate [19,21]. Any attempt of extension movement results in pain and thus limitation of extension of lumbar spine.
Loss of flexion range of motion in prolapsed intervertebral disc of lumbar spine manifests as limited end range or deviation from normal pathway of flexion. This loss may be due to altered position of the nucleus i.e. postero-laterally and deviation may occur to avoid sciatic nerve root irritation [19].
Also, the presence of an entrapped or adherent sciatic nerve root is unable to lengthen adequately and doesn’t allow flexion to occur in sagittal plane [22,23].
Mechanism by which McKenzie group improved in extension range of motion may be attributed to the fact that, correction of lateral shift by applying side gliding pressure opens the intervertebral space laterally which is then followed with extension movement of lumbar spine. This produces reduction of the disc disturbances,making impression that the pain moved from unilateral to central position and there is significant reduction in intensity of pain and centralization [21]. As the coronal plane movement is followed by sagittal movement i.e., extension, there is gain in lumbar extension ROM [24].
Hypothetically, pain from an Adherent nerve root is caused by mechanical deformation of structurally impaired soft tissues and experiments have shown the adherences between disc and nerve roots can occur after disc prolapse or injury [25,26].
These adhesions and contractions of connective tissue in and around the nerve cause symptoms, until remodeling of the affected structures has occurred [19]. Remodelling is achieved through repeatedly stressing the tissue [27,28]. In the study, with repeated extension, posterior annulus is under compression loading and reduced tangential stress and with the hydrostatic mechanism intact, the nucleus moves anteriorly [29]. This may be one of the reason that account for changes in mobility of lumbar spine with improvement in extension range by 66% and flexion range by 54%.
Improvement in flexion range of motion of lumbar spine by may be attributed to the fact that listing correction and repeated lumbar extension may reduce nuclear migration back in an annular tear or may realign a facet joint in such a way as to reduce painful stimuli. As centralization is achieved, low back pain become focused near the centre of the spine and slowly decrease which in turn increases the flexibility of the low back [30].
In Cyriax group, the patient was positioned prone or supine, with the traction belts exerting a pull to anterior or posterior aspect of the joint. Cyriax recommended the criteria of patient comfort, pattern of pain and limitation of trunk movement [4].
The tension upon posterior and anterior longitudinal ligaments created by traction causes a pressure drop and ligamentous centripetal force “sucks back” the herniated nuclear material [31]. Herniated disc repositioning or the vertebral bodies’ realignment caused restoration of more normal lumbar flexion and extension range of motion [32].
Traction given in supine produced a flexion moment as well as axial distraction of lumbar spine. The movement produced lead to reduction in anterior disc height and increase in posterior disc height [33]. There may be an increase in tension of posterior annular fibres and posterior longitudinal ligament which prevented excessive posterior movements of disc materials [34], as well as, the axial distraction of spine tend to reduce pressure, thus generated a significant flexion moment [35].
Function (ODI)
There was significant reduction in Oswestry Disability Index in both the groups at the end of the study. However, there was no significant difference between the two groups.
Normal pain free range of motion is essential for normal function. This holds true for any joint in the body and accordingly for the Lumbar spine. The components of Oswestry Disability Index viz. pain intensity, personal care, lifting, walking, sitting, standing, sleeping, social life, travelling and employment, are directly related to patients pain. The reduction in Oswestry Disability Index scores seen in both the groups may be due to reduction of pain and improvement in range of motion.
The patients with lumbar disc herniation have impaired mobility and lowered muscle strength [36] and this inadequate strength and endurance affects the function. The lumbar extensor muscles have a large potential for strength improvement when isolated through pelvic stabilization in McKenzie group [37].
Whereas in Cyriax group, it may be attributed to its biomechanical effect that the greatest increase in hydration of unloaded disc takes place within the first hour of load removal [37]. The trunk flexibility pointed towards fluid exchange resulting in improved function [38].
Conclusion
The results of the study suggests that both McKenzie and Cyriax approach are effective without significant difference between them in managing low back pain, function and range of motion of lumbar spine in patients with Prolapsed Intervertebral Disc.
Limitations
The limitations of the following study identified were short duration of the study, small sample size, no follow-up and no control group.
References
- Carroll LJ, Cassidy JD, Côté P (2000) The Saskatchewan Health and Back Pain Survey: the prevalence and factors associated with depressive symptomatology in Saskatchewan adults. Can J Public Health 91: 459-464.
- Philadelphia Panel (2001) Philadelphia Panel Evidence-Based Clinical Practice Guidelines on Selected Rehabilitation Interventions for Low Back Pain. PhysTher 81: 1641-1674.
- McKenzie RA, May S (2003) The Lumbar Spine: Mechanical Diagnosis and Therapy (2nd edtn). Spinal Publications, Waikanae, New Zealand.
- Pellecchia GL (1994) Lumbar traction: a review of the literature.J Orthop Sports PhysTher 20: 262-267.
- Murrin KR, Rosen M (1985) Pain measurement. In: Smith G and Govindo BG (editors) Acute pain: London: Butterworth.
- Kremer E, Atkinson JH, Ignelzi RJ (1981) Measurement of pain: patient preference does not confound pain measurement.Pain 10: 241-248.
- Revill SI, Robinson JO, Rosen M, Hogg MI (1976) The reliability of a linear analogue for evaluating pain.Anaesthesia 31: 1191-1198.
- Vianin M (2008) Psychometric properties and clinical usefulness of the Oswestry Disability Index.J Chiropr Med 7: 161-163.
- Gordon SJ, Yang KH, Mayer PJ, Mace AH Jr, Kish VL, et al. (1991) Mechanism of disc rupture. A preliminary report.Spine (Phila Pa 1976) 16: 450-456.
- Veres SP, Robertson PA, Broom ND (2008) ISSLS prize winner: microstructure and mechanical disruption of the lumbar disc annulus: part II: how the annulus fails under hydrostatic pressure.Spine (Phila Pa 1976) 33: 2711-2720.
- Donelson R, Aprill C, Medcalf R, Grant W (1997) A prospective study of centralization of lumbar and referred pain. A predictor of symptomatic discs and anular competence.Spine (Phila Pa 1976) 22: 1115-1122.
- Adams MA, May S, Freeman BJ, Morrison HP, Dolan P (2000) Effects of backward bending on lumbar intervertebral discs. Relevance to physical therapy treatments for low back pain.Spine (Phila Pa 1976) 25: 431-437.
- Coulehan JL (1985) Adjustment, the hands and healing.Cult Med Psychiatry 9: 353-382.
- Miller JK (1992) TheMcKenzie Approach. ClinOrthop 279: 8-20.
- Meszaros TF, Olson R, Kulig K, Creighton D, Czarnecki E (2000) Effect of 10%, 30%, and 60% body weight traction on the straight leg raise test of symptomatic patients with low back pain.J Orthop Sports PhysTher 30: 595-601.
- Wieting JM (2005) Massage, Traction, and Manipulation. Medscape.
- Werners R, Pynsent PB, Bulstrode CJ (1999) Randomised trial comparing interferential therapy with motorized lumbar traction and massage in management of low back pain in a primary care setting. Spine (Phila Pa 1976) 24: 1579-1581.
- Armstrong JR (1965) Lumbar disc lesions, (3rd edtn). Williams and Wilkins, Edinburgh, Livingstone.
- McKenzie RA (1981) The lumbar spine. Mechanical diagnosis and therapy. Spinal publications, Waikanae, NewZealand.
- Youssef J, Davidson B, Zhou BH, Lu Y, Patel V, et al. (2008) Neuromuscular neutral zones response to static lumbar flexion: Muscular stability compensator. ClinBiomech (Bristol, Avon) 23: 870-880.
- Laslett M (2009) Manual correction of an acute lumbar lateral shift: maintenance of correction and rehabilitation: a case report with video.J Man ManipTher 17: 78-85.
- McGill SM, Kippers V (1994) Transfer of loads between lumbar tissues during flexion-relaxation phenomenon. Spine (Phila Pa 1976) 19: 2190-2196.
- McKenzie RA (1972) Manual correction of sciatic scoliosis.N Z Med J 76: 194-199.
- Santolin SM (2003) McKenzie diagnosis and therapy in the evaluation and management of a lumbar disc derangement syndrome: A case study.J Chiropr Med 2: 60-65.
- Key JA, Ford LT (1948) Experimental intervertebral-disc lesions.J Bone Joint Surg Am 30A: 621-630.
- Melbye M (2010) An adherent nerve root--classification and exercise therapy in a patient diagnosed with lumbar disc prolapse.Man Ther 15: 126-129.
- Alfredson H, Pietilä T, Jonsson P, Lorentzon R (1998) Heavy-load eccentric calf muscle training for the treatment of chronic Achilles tendinosis.Am J Sports Med 26: 360-366.
- Langberg H, Ellingsgaard H, Madsen T, Jansson J, Magnusson SP, et al. (2007) Eccentric rehabilitation exercise increases peritendinous type I collagen synthesis in humans with Achilles tendinosis.Scand J Med Sci Sports 17: 61-66.
- Raghda A, AL-Farhan (2006) Effect of the repeated end range lumbar extension with lateral shift on centralisation monitored by soleus h-reflex. Department of Health Rehabilitation Sciences College of Applied Medical Sciences King Saud University.
- Solomonow D, Davidson B, Zhou BH, Lu Y, Patel V, et al. (2008) Neuromuscular neutral zones response to cyclic lumbar flexion.J Biomech 41: 2821-2828.
- Cailliet R (1981) Low Back Syndrome. (3rd edtn). Davis, Philadelphia, USA.
- Beattie PF, Nelson RM, Michener LA, Cammarata J, Donley J (2008) Outcomes after a prone lumbar traction protocol for patients with activity-limiting low back pain: a prospective case series study.Arch Phys Med Rehabil 89: 269-274.
- Colachis SC Jr, Strohm BR (1969) Effects of intermittent traction on separation of lumbar vertebrae.Arch Phys Med Rehabil 50: 251-258.
- Lee RY, Evans JH (2001) Loads in the lumbar spine during traction therapy.Aust J Physiother 47: 102-108.
- Saunders HD (1979) Lumbar traction*.J Orthop Sports PhysTher 1: 36-45.
- Carpenter DM, Nelson BW (1999) Low back strengthening for the prevention and treatment of low back pain.Med Sci Sports Exerc 31: 18-24.
- Cholewicki J, Lee AS, Reeves NP, Calle EA (2009) Trunk muscle response to various protocols of lumbar traction.Man Ther 14: 562-566.
- Costi JJ, Hearn TC, Fazzalari NL (2002) The effect of hydration on the stiffness of intervertebral discs in an ovine model.ClinBiomech (Bristol, Avon) 17: 446-455.
Relevant Topics
- Electrical stimulation
- High Intensity Exercise
- Muscle Movements
- Musculoskeletal Physical Therapy
- Musculoskeletal Physiotherapy
- Neurophysiotherapy
- Neuroplasticity
- Neuropsychiatric drugs
- Physical Activity
- Physical Fitness
- Physical Medicine
- Physical Therapy
- Precision Rehabilitation
- Scapular Mobilization
- Sleep Disorders
- Sports and Physical Activity
- Sports Physical Therapy
Recommended Journals
Article Tools
Article Usage
- Total views: 14502
- [From(publication date):
specialissue-2016 - Apr 03, 2025] - Breakdown by view type
- HTML page views : 13333
- PDF downloads : 1169