Research Article Open Access
Interprofessional Communication and Health Information Technology Education as Main Pillars of Medicine, Healthcare Administration and Public Health
Samadi-niya A*Principal Investigator, CANSIRPH Research; President and Co-founder, IRACA Solutions Inc., Canada
- *Corresponding Author:
- Atefeh Samadi-niya, PhD
Principal Investigator: CANSIRPH Research
Greater Toronto Area, Ontario, Canada
Tel: +416-402-3906
E-mail: Atefeh.Samadiniya@gmail.com
Received date: November 21, 2016; Accepted date: January 21, 2017; Published date: February 02, 2017
Citation: Samadi-niya A (2017) Interprofessional Communication and Health Information Technology Education as Main Pillars of Medicine, Healthcare Administration and Public Health. J Community Med Health Educ 7:500. doi:10.4172/2161-0711.1000500
Copyright: © 2017 Samadi-niya A. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community Medicine & Health Education
Abstract
Canadian healthcare leaders who participated in the pan Canadian National Study of Interprofessional Relationships between Physicians and Healthcare Administrators (CANSIRPH) emphasized that improving interprofessional relationships between physicians and healthcare administrators is the most important factor in success of healthcare systems and patient care quality. The leaders also considered that improving physicianmanager relations, patient care quality, medical errors reduction and efficient budget management are strongly correlated with improving communication and teamwork as well Health Information Technology (HIT). In fact, communication and teamwork shape 56% and HIT shapes 22% of satisfaction level of leaders with quality of interprofessional relationships between physicians and hospital administrators. CANSIRPH results also revealed that healthcare leaders across Canada are from different generations so a practical gap exists in healthcare professionals and leaders’ ability to use various HIT applications as previous generations are more prone to use of pen and paper whereas newer generation of leaders are more technology savvy. HIT applications should be transferable and easy to use by all professionals at different healthcare organizations across continuum of care because HIT tremendously affects interprofessional communication and to improve patient care, improving communications and teamwork among all members of healthcare teams including clinicians and managers seems extremely necessary.
Keywords
Health information technology; Communication; Patient care quality; Physician; Interprofessional relationships; Hospital; Public health; Community medicine; Healthcare education; Doctor manager relations
Abbreviations
CANSIRPH: Canadian National Study of Interprofessional Relationships between Physicians and Hospital Administrators; HIT: Health Information Technology; PHR: Physician hospital Relations; IRPH: Interprofessional Relations of Physicians and Hospital Administrators
Introduction
In a pan-Canadian research study, Canadian National Study of Interprofessional Relationships between Physicians and Healthcare Administrators (CANSIRPH), physician leaders and healthcare administrators across Canada considered Interprofessional relationships of doctor and manager as the foundation of success of healthcare systems. Canadian healthcare leaders at mid to senior level of management working at various healthcare organizations across Canada have chosen Communication and teamwork as the main factor that affect patient care safety, improving physician-manager relations, and efficient financial planning for healthcare [1]. CANSIRPH participants also emphasized that improving Health Information Technology (HIT) leads to improving Interprofessional relationships of physicians and healthcare administrators.
The results of CANSIRPH were published by the American Hospital Association, Canadian College of Health Leaders (CCHL), and Canadian Society of Physician Leaders (a branch of Canadian Medical Association) [2-6]. The results were also presented to thousands of healthcare leaders in different conferences, congresses, and events planned by the American Hospital Association, American College of Healthcare Executives, International Hospital Federation, Canadian College of Healthcare Leaders, HealthcareCAN, Ontario Association of Community Care Access Centers, and Ontario Hospital Association [7-10]. Presentations and publications based on CANSIRPH have encouraged many researchers and decision-makers to pay closer attention to improving interprofessional communication.
Healthcare system of countries with national health coverage such as Canada, focus their planning on the preventive measures and adequate health education. As the results of such important role that Community Medicine plays in the planning of healthcare budget and resource allocation of industrialized countries, improving inter professional communication of healthcare professionals and healthcare managers not only improves quality of prevention but also creates opportunities for more efficient healthcare educational programs for public and professionals.
One of the main educational points suggested by this article is providing an opportunity for the healthcare leaders of different sectors to learn the effective use and management of Health Information Technology (HIT). HIT is connecting different healthcare settings in Public Health and prevention, Community Medicine and health networks, healthcare education, and professional educational programs. E-health, M-health, Electronic Medical Records, Electronic Health Records, Patient Health Records, E-pharmacy, E-laboratory, email, Social Media, websites, internal and external applications for healthcare users and patient data are among some of the daily applications of HIT in industrial countries [11-15].
Professionals who are part of the large network of Community Medicine and Health Education are also affected by the quality and different usages of HIT. Primary health care providers, Family Physicians, Nurse Practitioners, Family Health Teams, Physician private offices, hospitals, Community Care Access Centers, Health Links, Professional organizations’ websites for patients and healthcare providers, government and universities are some of the users of the HIT. For example, one of the topics that require extra attention is preventing and treatment of child obesity, which requires collaboration of all healthcare sectors and public education [16].
The data is affected by the harmony among different applications and different users of HIT. Canadian Institute of Health Information, Canadian Institute of Health Research, Health Canada, National Institute of Health, and many other professional organizations rely on the accuracy, transferability, and convenience of use of data produced by HIT application across different healthcare sectors. Improving interprofessional communication should be a priority in different sectors of healthcare system including acute care, post-acute care, community care, and home care.
Role of health information technology (HIT) in physicianhospital relations
One of the recent pressing discussions in healthcare is the widespread use of health information technology (HIT): e-charts, econsultations, e-health, e-medicine, e pharmacy, and e-everything else in healthcare [17]. Healthcare administrators could benefit from wise use of HIT to align physicians with hospitals [18,19]. Connecting physicians’ offices to hospitals’ main intranet and patient charts, connecting hospitals with other hospitals, giving patients access to their personal medical charts, e-prescribing, communicating via e-mail and providing long-distance specialty consultation for remote and rural areas have created a new era in healthcare [17]. One of the very crucial roles of information technology in medicine or patient care is its usefulness as a computerized decision-support system that enables physicians to make evidence based decisions [20,21].
Some hospitals, especially in the United States, provide IT donations to physicians and strengthen physician-hospital relations by providing connections between physicians’ offices and hospitals [22,23]. Using IT applications, online resources for interprofessional care can help professionals work together more effectively [24]. Use of online scholarly journals, official websites and such audiovisuals as online educational video clips or synchronized web-based presentations (webcasts) are a few examples of how physicians and hospitals can benefit from HIT. This new era is very expensive because of the technology installation, licensing, and maintenance and implementation of clinical information systems, which are useful and appealing to physicians [25].
Use of IT helps in management of clinical services as well as collaboration among professions [26-28]. Different aged systems can result in a technology mismatch. Some initiatives involve physicians, and some do not relate to the clinical part of medical care. The use of HIT needs to be adjusted and changed in the practice of medicine. Some older generation physicians prefer paperwork while some newer generation physicians are technology savvy. Hospitals face a generation gap in use of technology, but they should focus on younger physicians as they build the future of healthcare [29].
Physicians do not practice as solo practitioners anymore; they practice in groups of professionals and in systems intertwined with information technology, e-health, and electronic patient records [29]. One doctor is only part of a very large system of care with time divided among clinics, hospitals, emergency rooms, private offices and hospital units. The hospital leaders would like to see doctors accessible everywhere at the same time, but it is not possible unless appropriate communication technology is provided to physicians [27]. Dividing time and energy among many required activities creates extra pressure on physicians and increases the possibility of burnout and medical errors. An organized and easily accessible system of care for physicians can enable them to be present physically in other locations but respond to the communications needed for patient care, such as refilling prescriptions and discharging patients’ notes [28,29].
Physician leaders and trusted physicians have been trying to encourage more physicians to use e-solutions for their practice because physician engagement is the key to use of any HIT application, such as electronic medical records (EMR), computerized physician order entry (CPOE) or medication order entry (MOE) [30,31]. Based on a survey completed in 2009 for nine industrialized countries, use of EMRs among family physicians is the lowest in Canada [32]. The reported percentages for countries were 99% for the Netherlands; 90% for Australia, Italy, New Zealand, Norway, Sweden and U.K; 72% for Germany; 68% for France; 46% for the United States and 37% for Canada. A different research study also reported that Canada is behind the United States in adoption of e-prescribing [33].
Change is inevitable although very difficult [17,29]. Adoption of HIT has created some friction between physicians and hospitals, especially when physicians cannot afford to use e-applications that are as sophisticated as those the hospitals [34]. In addition, some hospitals charge physicians for access to patients’ e-charts.
An advantage of HIT is having fast access to everything in patients’ charts in one single place. Physicians’ speed in reading charts and providing consultations is not as fast as X-ray or lab results, which can be speedily loaded into patients’ charts. Sometimes it takes only 30 seconds for an X-ray to be uploaded from the X-ray room to a patient’s chart, but physicians cannot perform patient consultations every 30 seconds for 24 hours 7 days of the week [17]. Adequate and appropriate use of HIT can improve the IRPH if the applications are user friendly and efficient for the physicians [29]. EMRs could provide a source of information for research and practice improvement as well [35]. Physicians could possibly use EMR data for their contribution in the advancement of quality of care [35].
The important role of hospital board members in using the hospital budget for information technology and its applications such as physicians’ portal is obvious [20]. If physicians do not cover the ER appropriately or if physicians do not accept on-call responsibilities, patients suffer. A formula approach to determine the financial cost of on-call physicians has been suggested [36]. Considering that, in rural regions of Canada, there might be only one hospital for hundreds of kilometers, if patients encounter an ER without an on-call physician, they must travel long hours to reach another hospital to receive care. Using different applications or portals such as telehealth, specialists in urban hospitals can help clinicians in rural areas in ERs or in specialty clinics. Using the formula could also help hospital administrators to monitor, manage, and control the costs of call coverage [36].
Physicians’ portal is the term used for information technology application used for physicians. Physicians’ relations with hospitals and healthcare organizations are directly related to the ease of use of physicians’ portals [37]. The components of physicians’ portal include (a) types of clinical data and transaction support available, (b) types of providers who have access to them, (c) the extent to which the systems can communicate electronically with Electronic Medical Records (EMRs), and (d) the directionality of information as uni-directional from hospital to physician, or bi-directional [37].
Methods
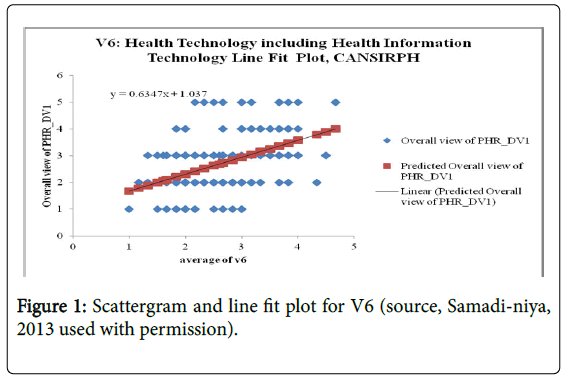
CANSIRPH was a quantitative multivariate correlational survey administered through the web, using Likert-type responses to items to collect data representing the opinions, attitudes and needs of Canadian physicians and Canadian hospital administrators concerning the IRPH in Canadian hospitals. The two research questions used for this paper are among a few research questions used to assess the results of CANSIRPH. Few thousands of healthcare leaders across Canada received the questionnaire. The results are generalizable and can be used as a baseline for further research studies. Factor Analyses of the results showed seven factors that affect quality of physician-manager relations and quality of patient care. Among them is Health Technology, which includes Health Information Technology as well as Communication and Teamwork. The reported tests for this article are a single-regression analysis, part of a multiple regression analyses, and percentages. V6 refers to Variable 6 and it is used as a code for HIT. V2 refers to Communication and teamwork. Detailed analyses are available in a complete open-access Dissertation published by ProQuest Open [1]. Summary of recommendations are available in publications based on CANSIRPH results [2-6].
Results
Research Question 1 and Hypothesis 1
R1Q: To what extent does technology, including Health Information Technology influence IRPH across Canada?
H10: Technology (including Health Information Technology) does not influence IRPH across Canada.
H1A: Technology (including Health Information Technology) influences IRPH across Canada.
H10: β=0
H1A: β ≠0
A single linear regression analysis revealed that adequacy of Health Technology, including Health Information Technology or HIT was a significant predictor of overall view toward IRPH (β=0.634714172, p=4.32E-12), accounting for (R2=0.219554686) the 22% of the variance in overall view. The correlation was a positive correlation (Figure 1). The line fit for the single linear regression was y=β0+β1 × 1 or y=1.037036316+(0.634714172 × V6). Considering the reported pvalue, which was far less than 0.05 and very close to zero, the null hypothesis was rejected. The correlation between these two variables is positive and moderately strong because β is in the upper half range but closer to mid-point (Figure 1).
The null hypothesis was rejected so technology (including Health Information Technology) influenced IRPH across Canada. The regression line shows that improving Health Information Technology improves quality of IRPH. CANSIRPH results showed that any factor that affect quality of physician-hospital relations in fact has a direct effect on quality of patient care safety, value-based patient care quality and healthcare budget management.
In summary, technology (including health information technology) moderately but significantly influenced IRPH across Canada accounting for about 22% of the variance in overall view toward physician-hospital relations (PHR) or interprofessional relations between physicians and hospital administrators (IRPH) for further discussions and detailed analyses refer to the chapter 3-5 of the open access complete research report (dissertation) [1].
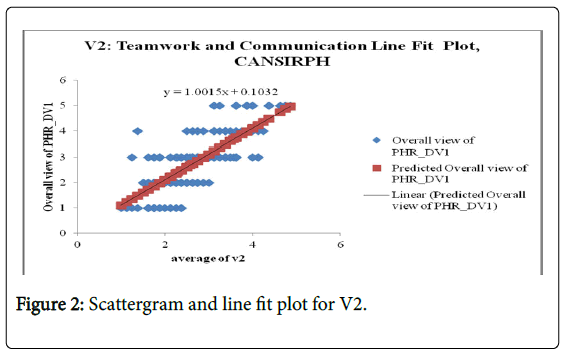
Research Question 2 and Hypothesis 2: RQ2 and H2: perspective on teamwork and communication (V2).
RQ2: To what extent does perspective on communication and teamwork issues influence IRPH across Canada?
H20: Perspective on communication and teamwork issues does not influence IRPH across Canada.
H2A: Perspective on communication and teamwork issues influences IRPH across Canada.
H20: β=0
H2A: β ≠ 0
A single linear regression analysis revealed that perspective on communication and teamwork was a highly significant predictor of overall view toward IRPH (β = 1.00148819, p=1.29E-35), accounting for (R2=0.556667532) the 56% of the variance in overall view. The correlation was a positive correlation (Figures 1 and 2).
The line fit for the single linear regression was y=β0+β1 × 1 or y=0.103240788+ (1.00148819 × V2). Considering the reported p-value, which was far less than 0.05 and very close to zero, the null hypothesis was rejected. The correlation between these two variables was very strong because β is 1. The coefficient (β) is a number reported between 0 and 1, in which 1 is the highest level of correlation. Perspective on communication and teamwork issues extremely influenced the overall view toward IRPH.
In summary, the analysis showed that perspective on communication and teamwork issues extremely and significantly influenced IRPH across Canada (the highest among seven factors if considered individually) accounting for about 56% of total variance in overall view toward IRPH (Figure 2). The effect of this factor on the IRPH was amazingly significant.
Discussions
The issue of time demand on physicians is crucial [34]. Any project that can increase efficiency and decrease the time demand for physicians should receive positive attention from hospital medical staff. For example, if administrators could show physicians that their new projects for e-pharmacy and e-prescription decrease the time they need to communicate with nurses and diminish the number of calls from hospital staff regarding the written prescription, they may have more buy-in from physicians [17]. If a HIT application is too difficult to learn, too complex to operate, and even too confusing because of frequent updates, physicians will ignore it and continue the status quo [37].
Healthcare administrators could benefit from wise use of HIT to align physicians with hospitals. Connecting physicians’ offices to hospitals’ main intranet and patient charts, connecting hospitals with other hospitals, giving patients access to their personal medical charts, e-prescribing, communicating via e-mail, and providing long-distance specialty consultation for remote and rural areas have created a new era in healthcare [17]. One of the very crucial roles of information technology in medicine or patient care is its usefulness as a computerized decision-support system that enables physicians to make evidence-based decisions [20,21].
Health information Technology (HIT) has become one of the main pillars of delivering healthcare in 21st century and beyond [38]. One of the contemporary leadership issues, which have attracted so much attention, is appropriate education of Health Information Technology for healthcare professionals both at universities and in healthcare organization [38]. This paper emphasizes the importance of improving interprofessional communication including Health Information Technology and addresses educational needs of healthcare leaders and specifically physician leaders in healthcare organizations.
A gap exists between the new generations of technology savvy health administrators and physician leaders and the previous generations who used pen and paper not only for their education but also during their professional work so far [38]. Suggesting some aspects of teaching HIT, this research article provides some insight into providing appropriate information for healthcare administrators, physician leaders and other healthcare organization managers to become familiar with HIT and participate in planning for efficient use of HIT’s different applications. Providing an on-going education regarding different perspectives related to use of HIT seems necessary for all healthcare organization executives, physician leaders and healthcare organization managers [26].
Effective and adequate knowledge level of Health Information Technology is the prerequisite of acceptance into the Governor’s Board Exam offered by the American College of Healthcare Executives as part of the Board Certification in Healthcare Management and Fellowship status of ACHE (FACHE), which is the highest possible distinction for healthcare administrators and medical managers.
HIT has become one of the main components of delivery of healthcare in 21st century [12]. Appropriate use of HIT has great impact on physician-healthcare organization relations, employee satisfaction, patient satisfaction, and quality of care provided for the patients [12]. However, a physician does not need to know about the details of running a wireless network. A healthcare manager, on the contrary should be aware of all aspects of HIT although not required to work with all domains. A network administrator must know about all aspects of the HIT as the person whose main responsibility is installing, running, and maintaining HIT for healthcare systems [11-15]. More publications related to CANSIRPH results will be available in near future [39].
Conclusion
This article sheds light on the importance of improving interprofessional communication and Health Information Technology and their effects on quality of interprofessional communication, doctor-manager relationships, quality of patient care, and budget management in Medicine, healthcare administration, and education. To address the gap that exist in the knowledge level of healthcare leaders of different generations, HIT educational programs should be designed to teach healthcare leaders how to use HIT or plan for its different applications effectively in their healthcare organizations across the continuum of care. Community Medicine, Public Health, and Health Education rely on the proper and adequate education of HIT. Although healthcare organization managers do not need to learn about all aspects of HIT but it seems necessary for the healthcare organization executives to be aware of HIT’s different perspectives. Community Medicine, health education, and Public Health performance measures also heavily rely on the adequate use of HIT because data collected to report healthcare status and social determinants of health depend on effective use of HIT’s applications by professionals, researchers, leaders and healthcare policy makers.
In summary, Canadian healthcare leaders considered IRPH as the most important factor in success of healthcare systems and patient care quality. On one hand, communication and teamwork shaped about 60% and Health Information Technology shaped 22% of satisfaction level of leaders with quality of IRPH. On the other hand, effective use of Information Technology tremendously affects communication and teamwork. In other word, to improve patient care, effective, clear, concise interprofessional communications among all members of healthcare teams including clinicians and managers is necessary. As the result, improving interprofessional communication and Health Information Technology education are considered main pillars of Medicine, Healthcare Administration, and Public health.
Study Limitations
The questionnaire was sent to all Canadian provinces and territories in English Language only. The French version was not available. In future follow-up studies, both versions could possibly be used if funding and resources are available.
Acknowledgement
This paper is written in response to an invitation from the Journal of Community Medicine and Health Education. Some parts of current paper have been published in a Doctor of Health Administration open access Dissertation (Thesis) written by Dr. Atefeh Samadi-niya, MD, DHA (PhD), FACHE, CCRP, CRA. The content of the Dissertation and this paper are copyrighted by Dr. Atefeh Samadi-niya. A few of publications and presentations based on CANSIRPH results are included at the beginning of the list of references. To access further information regarding the publications and presentations related to CANSIRPH please contact info@CANSIRPH.com or visit its upcoming website at www.CANSIRPH.com or http://cansirph.com
Dr. Samadi-niya has been nominated and awarded as one of the Leading Physicians of the World and as one of the Worldwide Leaders in Healthcare in year 2016 and her profile is published in both 2017 top doctors’ directories by the International Association of Healthcare Professionals. To access the latest publications and presentations by Dr. Samadiniya, including this paper, you can visit her profile at http://www.theleadingphysiciansoftheworld.com/Atefeh.SamadiNiya.8137339.MedicalManagement.html.
References
- Samadi-niya A (2013) Interprofessional relationships between physicians and hospital administrators across Canada: A quantitative multivariate correlational study. PQDT Open.
- Samadi-niya A (2015) How strengthening the relationships between Medicine and Management improves care. H&HN Daily.
- Samadi-niya A (2015) Suggested methods to improve physician-hospital relationships in Canada [Youtube video]. Health Leaders Canada.
- Samadi-niya A (2015) Suggested methods to improve physician-hospital relationships in Canada. Healthc Manage Forum 28: 106-113.
- Samadi-niya A (2015) Part 2: The perception of Canadian healthcare leaders toward physician-hospital relations. The official Magazine of the Canadian Society of Physician Executives: Canadian Physician Leadership J 4: 35-39.
- Samadi-niya A (2014) Part 1: The importance of physician-hospital relations in Canadian healthcare system. The official Magazine of the Canadian Society of Physician Executives: Canadian Physician Leadership J.
- Samadi-niya A (2015) Interprofessional relationship of medicine and management is the foundation of success of global healthcare systems. International Hospital Federation: Chicago, USA.
- Samadi-niya A (2015) Interprofessional relationship of medicine and management is the foundation of success of global healthcare Systems. American Hospital Association, and International Hospital Federation: Chicago, USA.
- Samadi-niya A (2015) Factors that influence relationships of medicine and management as well as leadership and governance of healthcare systems in canada. OACCAC annual Conference.
- Samadi-niya A (2015) Effects of interprofessional doctor-manager relationships on patient care Quality. OACCAC Annual Conference 2015.
- Eom SB (2005) Inter-organizational information systems in the Internet age. Idea Group Publishing, Hershey, Pennsylvania, USA.
- Galliers RD, Leidner DE (2003) Strategic information management: Challenges and strategies in managing information systems (3rd edn), Elsevier, New York, USA.
- Fjermestad J, Saitta J (2005) A strategic management framework for IT outsourcing: A review of the literature and the development of a success factors model. J Inform TechCase& Application Research 7: 42-60.
- Harbert T (2010) When IT is asked to spy. Computer World 44: 14-20.
- Turban E, Leidner D, McLean E, Wetherbe J (2008) Information technology for management: Transforming organizations in the digital economy. (6th edn), John Wiley & Sons, Inc., Hoboken, New Jersey.
- Samadi-niya A (2016) Case study: importance of timely diagnosis of non-alcoholic fatty liver disease in a child with Vague Symptoms: part 1. Annals of Clinical Case Reports 1: 1111.
- Cash J (2008) Technology can make or break the hospital-physician relationship. Healthcare Financial Management 62: 104-109.
- Fera WA (2007) Using information technology to align physicians and hospitals. Frontiers of Health Services Management 24: 27-30.
- Jbilou J, Landry R, Amara N, El Adlouni S (2009) Combining communication technology utilization and organizational innovation: Evidence from Canadian healthcare decision makers. J Med Syst 33: 275-286.
- Johnson B (2006) Hospitals, physicians and information technology. Trustee 59: 23, 27.
- Straus S, Haynes RB (2009) Managing evidence-based knowledge: The need for reliable, relevant and readable resources. CMAJ 180: 942-945.
- Whitham JC, Bernstein SW (2007) Bonding with physicians: Hospitals and IT donations. Trustee 60: 29-30.
- Amatayakul M (2006) Digital perspectives: will you provide IT relief to physicians? Healthcare Financial Management 60: 116-117.
- Macdonald CJ, Stodel EJ, Chambers LW (2008) An online interprofessional learningresource for physicians, pharmacists, nurse practitioners, and nurses in long-term care: Benefits, barriers, and lessons learned. Inform Health Soc Care 33: 21.
- Callen JL, Braithwaite J, Westbrook JI (2008) Contextual implementation model: A framework for assisting clinical information system implementations. J Am Med Inform Assoc 15: 255-262.
- Litch BK (2007) The re-emergence of clinical service line management. Healthc Exec 22: 14-18.
- Simpson RL (2008) Caring communications: How technology enhances interpersonal relations, Part I (Review). Nursing Administration Quarterly 32: 70-73.
- Simpson RL (2008) Caring communications: How technology enhances interpersonal relations, Part II. Nursing Administration Quarterly 32: 159-162.
- Ansel D (2009) Portal to better physician relationships: If you’re going to do a physician portal, do it right! Marketing Health Services 29: 27-28.
- Aarts J, Ash J, Berg M (2007) Extending the understanding of computerized physician order entry: Implications for professional collaboration, workflow and quality of care. Int J Med Inform 76: S4-S13.
- Rossos PG, Abrams H, Wu R, Bray P (2006) Active physician participation key to smooth MOE/MAR rollout . Healthcare Quarterly 10: 58-64.
- Silversides A (2010) Canadian physicians playing “catch-up” in adopting electronic medical records. CMAJ 182: e103-e104.
- Eggertson L (2009) Canada lags US in adoption of e-prescribing. CMAJ 180: e25-e26.
- Cohn KH, Berman J, Chaiken B, Green D, Green M, et al. (2009) Engaging physicians to adopt healthcare information technology. J HealthcManag 54: 291-299.
- Mitiku TF, Tu K (2008) Using data from electronic medical records: Theory versus practice (ICES Report). Healthcare Quarterly 11: 23-25.
- Reed HL, Hayduk MC, Tollefsen BL (2010) The burden of call: An objective approach to determining financial payment. Physician Executive 36: 40-46.
- Bujak SJ (2009) Overcoming generational differences. Healthcare Executive 24: 80,82.
- Tan FB (2003) Advanced topics in global information management. Hershey, Idea Group, USA.
- Gabarro J (2007) When a new manager takes charge. Harvard Business Review 85: 104-117.
Relevant Topics
- Addiction
- Adolescence
- Children Care
- Communicable Diseases
- Community Occupational Medicine
- Disorders and Treatments
- Education
- Infections
- Mental Health Education
- Mortality Rate
- Nutrition Education
- Occupational Therapy Education
- Population Health
- Prevalence
- Sexual Violence
- Social & Preventive Medicine
- Women's Healthcare
Recommended Journals
Article Tools
Article Usage
- Total views: 5101
- [From(publication date):
February-2017 - Nov 23, 2024] - Breakdown by view type
- HTML page views : 4407
- PDF downloads : 694