Research Article Open Access
Inter-Professional Collaboration between Family Doctors and Nurses at the End of Life. Challenges of Community-Based Palliative Care in Switzerland
Vanessa Alvarado and Brigitte Liebig*
Applied Psychology, University of Applied Sciemces Northwestern Switzerland, Olten, Switzerland
*Corresponding Author:
- Brigitte Liebig
Professor, Applied Psychology
University of Applied Sciemces Northwestern Switzerland
Olten, Switzerland
Tel: 41 62 62957 23 61
E-mail: brigitte.liebig@fhnw.ch
Received date: May 18, 2016; Accepted date: May 26, 2016; Published date: May 31, 2016
Citation: Alvarado V, Liebig B (2016) Inter-Professional Collaboration between Family Doctors and Nurses at the End of Life; Challenges of Community-Based Palliative Care in Switzerland. J Comm Pub Health Nurs 2:124. doi:10.4172/2471-9846.1000124
Copyright: © 2016 Alvarado V, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community & Public Health Nursing
Abstract
Inter-professional collaboration between family doctors and nurses is a decisive element of the quality in community-based palliative care. Previous research shows that professional interactions between nurses and family doctors are embedded in formal structures and social relationships, and can be challenging in terms of professional behaviour and self-concept.
While research has focussed on inter-professional collaboration in hospitals, only little is known about the premises and problems of inter-professional collaboration in community-based palliative care. This article focuses on the challenges of inter-professional collaboration between family doctors and nurses in community-based palliative care in Switzerland, using an explorative research design. 24 group discussions were conducted in 2013/14 with 91 family doctors and 72 nurses in French, Italian and German speaking language regions of Switzerland. The care givers were asked about their everyday experiences and perspectives. For the interpretation of data qualitative content analysis has been applied.
Results show that inter-professional collaboration in community-based palliative care is highly challenging due to different factors: First of all deficits related to organizational aspects of work constitute a source for conflict: The asynchrony of working hours of family doctors and nurses prevent personal contact, communication and trust building. More than that different professional values regarding palliative care and dying can cause disturbances in collaboration and affect the personal relationship between professionals negatively. Uncertainties regarding leadership and a failure of meta-communication provide further impediments for inter-professional collaboration. The article provides recommendations how to support and instruct collaborative processes between family doctors and nurses in end-of-life care.
Keywords
Inter-professional collaboration; Palliative care; Community care; Family doctors; Nurses; End of life
Introduction
The collaboration of family doctors (FDs) with nurses and other health care professionals represents important elements of quality in community–based palliative care (CBPC) [1]. In palliative care, at home or in the nursing home, successful collaboration is of great importance to guarantee the fulfilment of patients’ needs and wishes, to ensure the longest possible stay in the patients’ place of choice and to avoid unnecessary admission into intensive care units [2-4]. In addition, good inter-professional collaboration (IPC) can be associated with an increase in mutual support and an improvement in employee satisfaction [5,6].
Nursing and health sciences emphasize the collective, goal-oriented aspect of IPC between doctors and nurses [7,8]. They show that the collaborative process is embedded in formal structures, just as it is in social relationships and interactions [9]. This requires not only the willingness of caregivers to contribute to collaboration, but also a specific set of knowledge and interpersonal skills, which include mutual respect, trust and effective communication [10,11]. Petri [11] also describes awareness about one’s own professional role and the role of others in IPC as crucial for a successful collaboration.
Further studies illustrate that collaboration between doctors and nurses is enormously challenging in terms of professional behaviour and self-concept as well as in terms of organization [12]. Different professional traditions, training paradigms and professional experiences contribute to different perceptions, ways of thinking and acting in the medical and nursing profession [13]. A number of studies also report disputes between doctors and nurses about areas of competence or roles in combination with professional rivalries [14-16], which can impair communication and knowledge transfer. And whilst nursing training and education seem to favour collaborative abilities [13], physicians seem to look at IPC with a markedly hierarchical perspective [17] and are not always informed about the professional competences of nurses [18].
Whilst literature on IPC in the clinical context is extensive [6] the possibilities and limitations of IPC have not been sufficiently addressed in CBPC [19]. Care situations at the end of life require specific forms of organization and collaboration [20,21]. In a review of literature, Xyrichis and Lowton [22] report various aspects which foster and prevent IPC in primary and community care: Besides challenges related to the spatial distance between care providers, team sizes and compositions, the (in)stability of team membership or uncertainties about leadership in primary health care teams are described as significant factors of IPC. Further, a lack of regular team meetings,time pressure and especially a lack of clear goals and objectives are identified as important determinants of less effective team processes.
As in many other European countries the development of CBPC is an important public health issue and part of national palliative care strategies also in Switzerland, where the number of palliative care patients is increasing rapidly [23,24]. According to recent surveys three quarters of patients requiring palliative care services could be looked after by means of primary care [25]. Due to the federalist organization of the Swiss health system, the history and standing of palliative care in community care settings vary considerably across regions and cantons in Switzerland; uniform structures and standards of CBPC services are generally lacking, and improvements of inter-professional collaboration between PC providers is estimated as highly important by Swiss health care representatives [26]. First studies point out that considerable challenges exist with respect to information sharing about patients' situation, that inter-professional collaboration between FDs, hospital doctors and other specialists or mobile palliative acre teams in primary palliative care is seen rather critically [27] .
Aside from first studies the preconditions of work in CBPC settings is rather unknown; especially very little is known about the limitations and possibilities for inter-professional collaboration between FDs and nurses in this field. This article emanates from the need for more information about the specific challenges related to IPC between FDs and nurses in community-based palliative care in Switzerland. It especially aims at the identification of challenges related to the collaboration between FDs and nurses in palliative home care and in nursing homes.
Methodology
Since knowledge regarding the conditions of IPC between physicians and nurses in CBPC is very limited, an exploratory research design seemed most appropriate for this study. For data collection, 12 groups of FDs (with 6-8 doctors each) and 12 groups of nurses (with about 6 nurses each) were constituted and invited to discuss premises, challenges, and practices of community-based palliative care, concentrating on decision making in end-of-life care. Groups were created based on a sample of about 91 FDs, who were contacted and preselected with the help of regional institutes of general practice in the German, French and Italian speaking regions of Switzerland (namely Lucerne, Vaud and Ticino). Then, about 72 community and nursing home nurses involved in palliative care were recruited with the help of nurses associations and the nursing homes management. The groups were kept professionally homogeneous in order to identify professional views of both FDs and nurses and allow group members of one profession to express themselves freely about IPC. The professional groups varied with respect to gender and specialization: they included nurses with specialization in home care, palliative or oncological care, and FDs with different years of experience in palliative care.
For the group discussions a semi-structured discussion guideline was created, which followed the analytic objectives (see below). The discussion guidelines directed the group discussions, whilst still allowing participants to develop their own perspectives [28]. After the group discussions, FDs and nurses were asked to answer a brief standardized questionnaire, providing us with basic demographic and work related data (such as e.g. professional experience, institutional context). On average, the FDs were 53.1 years old and worked already 16.6 years as family physicians (range: 1-42 years); the nurses were 44.6 years old and working 16.7 years in their profession on average (range:1-36 years). The group of nurses was mixed regarding their expertise in palliative care: there were nurses from mobile palliative care teams, nursing homes, and home care nurses.
The group discussions were conducted from November 2013 to April 2014 in three Swiss cantons; they were recorded and transcribed verbatim. A qualitative analysis of data has been conducted following the procedures of qualitative content analysis [29]. The organization of data has been supported by the computer software Atlas/ti. Based on generative questions and sensitizing concepts concerning IPC, the analysis successively intended to elaborate key categories of explanatory character. To begin with, the data analysis focused on the identification of challenges of IPC in community-based palliative care, as nurses and FDs have reported them. Then, the main sources for these challenges as well as the care givers strategies to overcome potential problems were analysed.
Limitations
The qualitative study is limited to the specific cases which it addresses. We are aware that the sample size of 91 FDs and 72 nurses is small and that the professionally homogeneous composition of both medical and nursing groups did not allow for a triangulation of perspectives with respect to the specific collaborative situations described. Both groups referred to situations that were not verifiable by the other groups (on triangulation see [30]). Yet, the quality of the results was improved by systematic and comparative analysis of data generated by group discussions with FDs and nurses, as well as within the groups of professionals. After having coded the data from French, German and Italian texts, the codes were triangulated across language regions in order to enlarge and validate the findings. A member check of findings was provided in three workshops, at which a selected number of respondents participated.
Ethical approval by an institutional review board was not required for the study because our research did not include clinical trials, patient interviews or real-time observations of doctor-patient interaction. The study was based on the narratives of FDs and nurses, who voluntarily took part in group discussions. No questions about sensitive patient data were included into the research.
Results
As our data show, FDs and nurses emphasize the importance of IPC in dealing with patients and families in community-based palliative care.
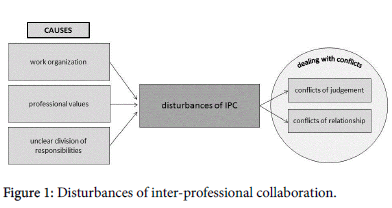
The professional groups rely strongly on each other's presence and expertise when daily tasks have to be managed. However, when asked about the challenges of IPC, group discussions with FDs and nurses revealed a number of conflicts, which create strong barriers for collaboration and potentially reduce the quality of palliative care [31]. Within the variety of narratives from both professional sides, two main types of conflicts have been identified: we labelled them as ‘conflicts of judgement’ and ‘conflicts of relationship’ [32] (Figure 1).
'Conflicts of judgement' frequently arise between FDs and nurses when they both share the goal of providing high quality palliative care for patients, but do not agree with the proposed or taken course of action. From the nurses’ point of view, this type of conflict issues from different professional perspectives on dealing with patients’ symptoms in end-of-life care: According to them, FDs intervene medically too often, instead of assessing the patients’ situation in a holistic way. Conflicts of judgement are also described by family doctors, as the following statement of a FD illustrates:
Family doctor: “nurses thought that no more treatment should be given (.), and then in the doctor’s office (.) ehm (.) they had to set up an infusion and when they called the head nurse and she looked inside [the room], she said "you cannot be serious about this”, in front of all the people (she said) you cannot be serious about this” (LU_doctorsGD3:748-751)
This excerpt documents not only a considerable gap in the interpretation of the need for action in this situation, but also a hiatus in the perception of the collaborating professions as to the palliative care experience. Different viewpoints and the lack of mutual professional recognition can result in a 'conflict of relationship', which again causes profound impairment of collaboration, as will be shown later.
A lack of appreciation from FDs was also reported by nurses: in these cases conflicts of relationships mainly resulted from the FDs enactment of professional hierarchies and a lack of respect. From the nurses’ perspective, FDs did not seem to acknowledge nurses' competences in situations of decision-making. In their eyes doctor’s attitude seemed even more misplaced, since nurses felt usually close to patients, and therefore wanted to be closely involved into decisionmaking processes at the end of life.
Nurse 1: "Our problem is that they [doctors] often don’t acknowledge our competences. Sometimes they still have a vision of "
Nurse 2: "Omnipotence"
Sources of disturbances in inter-professional collaboration
A closer look at the data shows that inter-professional conflicts are linked to a variety of work-related challenges in CBPC: Besides organizational aspects, different professional values and levels of competence were identified as the three main underlying factors.
a) Challenges related to work organization
Organizational deficits constitute a main source for conflicts between professionals in community-based palliative care. Mostly, a lack of continuity and availability of the professional counter-part (either nurses or FD) is mentioned as a source of complications in IPC. This mainly results from the asynchrony of work processes. A heavy workload in the surgical field implies that FDs often visit palliative care patients at home or in nursing homes during off-hours. Nurses, though, often work part-time and in shifts in order to provide an around-the-clock-service. This means that at the time when nurses are at a patient’s bedside, FDs often receive patients in their surgery.Consequently FDs try to contact nurses during their breaks or after work. The asynchrony of working hours results in a lack of personal contact, which again impedes on communication and mutual understanding. Due to this fact, also the organization of care processes become highly challenging: Agreements on further steps in the palliative care process have to be made during work breaks or after work, and are based on written reports, e-mails or phone calls – which leave room for misunderstandings and potentially impair shared decision-making.
Nurse: “In the moment in which I am with the patient, the doctor is not necessarily available (.) and later, when I am not with the patient anymore it is difficult for me to assess a patient’s situation (.) normally, I should do that when I am with the patient” (LU_nursesGD2: 910-915)
While FDs complain about the discontinuity of nursing staff in home care service teams (“the nurse who saw the patient the other day is not the nurse who is going to see the patient the day after (…) this makes it difficult”), nurses mention a lack of availability of doctors in palliative home care, which causes them to look for other medical colleagues (“homecare nurses are so helpless due to unattainable doctors, so they contact MPCTs [mobile palliative care teams]”). And in nursing homes, nurses mention that they would prefer to work with in-house physicians.
b) Different professional values
Further, significant disturbances in IPC result from different goals and orientations related to palliative care between the two professional groups: FDs and nurses often report that they "just see things in a different way". As our study shows, these differences mainly relate to different professional values regarding the process of dying: FDs are open to suggest medical treatments which are to some degree curative at the end of life. This attitude is not only mentioned by nurses, but also reported in self-descriptions of FDs, who feel that nurses omit curative treatments for patients in end-of-life situations. Divergent orientations are expressed by FDs reporting nurses as being “homeopathic” (LU_doctrosGD1: 880), thinking “the less the better” (LU_doctorsGD1: 885-887) or almost practicing “euthanasia” (LU_doctorsGD4:611). As the following extract from a group discussion with FDs demonstrates, different viewpoints and the perceived "withholding" of nurses regarding medical interventions can cause conflicts and have to be taken very seriously due to the frequency of the reports.
Family doctor: “I would say nurses have this attitude (.) they tend not to do anything in situations when (.) death is foreseeable (.) well, they are very reluctant (.) there are situations (.) when something could be done in such a phase (.) to improve quality of life or so (.) or maybe (.) even do something else (.) this is difficult (.) conflicts come up due to this’’ (LU_doctorsGD2: 565-569)
On the other hand though, nurses often report that physicians "withhold" medication such as pain killers. From their perspective this might also result from a lack of knowledge and experience. FDs also agree that there are different degrees of knowledge among colleagues, when medication in palliative care situations is concerned. Beyond that, conflicts between FDs and nurses turn out to be rooted in different viewpoints with respect to the process of dying. Nurses describe themselves as being able to better "accept", "withstand" or "bear" the process of dying, while they perceive FDs as being strongly oriented towards curative aspects in end-of-life situations.
Nurse: “You have the feeling that some physicians took the oath to save lives and that they have difficulties when someone is going to die, and to let that happen” (LU_nursesGD4: 480-481)
Different attitudes regarding the process of dying are stated quite frequently by nurses and are a principal source of conflict, which again has a strong impact on the planning and coordination of interprofessional actions.
c) Lack of competences and unclear sharing of responsibilities
The perception of each other's competences regarding self-reflection varies considerably between the professional groups involved in our study. For instance, nurses mention a high degree of self-reflection with respect to values and ideas regarding dying and death. They see themselves accompanying a dying person and being able to "bear" situations. Nearly half of the nurses, who participated in the group discussions, have attended a training or further education program related to palliative care at least once, compared to only 37% of the FDs. It might be due to this fact that nurses describe the knowledge and experience of FDs as comparatively small, and report considerable challenges of IPC resulting from this:
Nurse: “I think there is a lack of education and training sometimes”
Interviewer: “Regarding who?”
Nurse: “Regarding physicians (…) it makes us, well it makes me, feel uncomfortable explaining to the physician "no, you know, you don’t have to do that". This makes me (.) I always try to (.) well if you contradict them, you don’t have any collaboration anymore. It is difficult” (VD_nursesGD1: 407-414)
Then again, nurses feel strengthened in their professional autonomy due to their acquired competences: in their eyes, doctors' reference to hierarchical positions seems outdated and inappropriate. Quite contrary, according to nurses’ professional self-understanding, a close collaboration should be based on shared responsibilities between care providers. They demand more responsibility in the caring and decision-making process based on their strong relationship to patients and families.
At the same time, the discussions among FDs illustrate that they wish to retain the lead in managing the palliative care process. From their perspective, they are occasionally not even sufficiently involved in decision-making. This is especially the case for FDs who provide palliative care in nursing homes: Here, as critically discussed in groups of FDs, nurses often prepare decisions with patients and relatives or handle end-of-life situations on their own. Sometimes, this includes the fact that nurses do not call the FD when a patient is dying or even inform FDs only after patients have died.
How to deal with conflicts?
Also in dealing with the challenges of IPC, as they have been documented above, the two professional groups show considerable differences: FDs often see themselves as generally adapting to conflicts and accepting the somewhat less than perfect situation, in order to protect the patient. This seems especially true when inter-professional conflicts based on different values and attitudes turn up. The following quotation is derived from a discussion between two FDs, who discuss strategies of overcoming disagreements between nurses and FDs.
Family doctor: “because I noticed (.) there was something in the room, they had already discussed it, it made sense for the relatives and the patient (.) and when I come and play the wise guy (.) then nobody gains anything” (LU_doctorsGD2: 859-861)
The excerpt illustrates, that this FD does not agree with the fact that the collaborating nurse has already discussed further steps with the patient and family without consulting him; but he does not react critically in order to not endanger the palliative care situation. This behaviour is perceived positively by nurses: they experience FDs as being open to discussing further steps and considering nurses' opinions.
However, conflicts related to work organization seem not only to be overcome defensively, but also by selecting "good partners" from the very beginning. FDs report to collaborating much better with private homecare nurses - because private service organizations provide more continuity regarding staff - and with nurses they have known for a long time. The benefit of a long lasting relationship between FDs and nurses is that it allows the development of mutual trust: "they know what I want and I know what they are able to do" (LU_doctorsGD2: 579).
Nevertheless, statements from nurses indicate that they quite often feel left alone with questions related to IPC: In their opinion, FDs tend to avoid communication concerning challenges of IPC, so nurses discuss respective questions primarily within their own professional group. Nurses rarely give feedback on collaborative issues to their medical colleagues because they anticipate disinterest or rejection. The following statement illustrates this strategy:
Nurse: “it is difficult to say it, but very often we don’t give feedback because we already gave it 50 times and no one listens to us and they say "I knew what I was doing". It is a pity and I think (…) probably it’s part of our profession. We want to talk and share because we learned it that way, all of us have learned to work like this. Physicians probably learned it differently and it seems they have to defend their power” (TI_nursesGD2: 1014-1020)
In general, meta-communication, in the sense of "communicating about communication" [33], between care providers appears hard to realize. As nurses report, FDs scarcely communicate about the status of collaboration. Also discussions between FDs show that they tend to avoid communication on collaborative situations with nurses. FDs seem to prefer external consultancy (e.g. by medical colleagues from MPCTs) or exchange within their professional group, rather than talking about perspectives with their nursing colleagues.
Discussion
As the group discussions with FDs and nurses in CBPC illustrate, inter-professional collaboration is highly demanding, and can generate various conflicts in everyday interaction. Often conflicts of relationship and task-related conflicts seem to be interrelated. While these conflicts are well described in organizational psychology [32] and not specific to any professional field, the sources of these conflicts, as they arise in IPC between FDs and nurses, can be related to the specific characteristics of the community-based palliative care setting. One of these characteristics is the hierarchical organization of this field, as part of the medical arena [34]. While the norms and rules of IPC are integrated into institutionalized work processes in hospitals or hospices, the freedom of the CBPC setting and the isolation from other care givers allows the negotiation on professional roles and actions.
Challenges of IPC are accentuated, because CBPC is strongly characterized by a lack of time: Often FDs are able to get only "snapshots" of patients and therefore have to decide quite often on a fragmented basis of knowledge about the patients’ situation and his or her familiar situation. Since FDs and nurses do not necessarily perceive palliative care situations in the same way, conflicts are triggered. As studies on the formal conditions of CBPC suggest, the scarcity of time might be related to the minor financial reward for home visits - a barrier to IPC, which has also been identified CBPC in many European countries [26,24]. In Switzerland, activities which are important for inter-professional exchange and relationship building (e.g. coordinative tasks or case discussions), and which do not take place at the patient’s bedside are not financially rewarded [26]; this seems a plausible cause for time shortages in CBPC.
Beyond that, the work setting in CBPC is strongly characterized by repeated changes in caring personnel: In two of the three cantons studied here, FDs have to adjust repeatedly to new nursing staff during the palliative care process. This obstructs the exchange of information as well as communication between care givers and therefore forces patients and/or relatives into the role of a connecting link - even in cases where they don’t necessarily have to be involved. Besides discontinuities in staff, the asynchrony of work processes - especially inherent in home care settings - prevents care givers from building up common knowledge and experience in delivering palliative care, as well as creating trust in each other's competences - which is an important aspect of successful collaboration [35]. The asynchrony in care provision results in a lack of personal contact, so that trust can difficultly be built up and conflicts cannot be solved efficiently [36].
Furthermore, collaboration is a goal-oriented professional action, which is based on shared values, knowledge and skills [14]. Differences in professional values have been reported to be an important source of disturbance between caregivers also in CBPC. This is due to the fact that the shortcomings of work organization mentioned above do not allow the development of common norms and values. As our data show, FDs and nurses pursue the same goal, namely to provide good care for patients. But the professional groups do not often agree on how to achieve this goal, as they have different values and attitudes regarding medical treatment and the process of dying.
The division of responsibility has been found to be an organizational source of disturbance for inter-professional collaboration in CBPC. The findings let us assume that leadership is insufficiently defined especially in palliative home care, which causes unmet expectations and disappointments from all sides. Previous research shows that unclear spheres of responsibilities in combination with professional rivalries generate considerable challenges for collaboration [16]. When the division of responsibility remains unsolved, this results in conflict between care providers which in return generates negative effects on the professional well-being. The wide range of expectations concerning responsibility might be explained by the self-designation of competences, but also by the different expectations from IPC.
Numerous studies describe the ability to work as part of a team, to communicate and to be respectful of others as fundamental attributes of IPC between nurses and physicians [37,38]. However, care providers, namely FDs and nurses, enter the care process with already established ideas regarding collaboration which are quite contrary [17]. Yet, communication about different viewpoints is very restricted due to work related elements in CBPC, as well as to professional hierarchies and tensions, and therefore cannot help to improve the work situation of palliative home and community care providers [39]. Different expectations are rarely communicated in palliative care teams, as they are confronted with a lack of personal contact and trust. Therefore, rules are often not set for the care process and a shared perspective of the balance of power between care givers is missing [7].
Finally, our data show that the two professional groups deal with disturbances of inter-professional collaboration in different ways. Whereas FDs tend to avoid or to adapt to conflicts, nurses retreat into their own professional team. According to Drinka and Clark [40] this is a common phenomenon in inter-professional health care teams. According to Tuckmans’ "Model of development in small groups" (first published in 1965) we can assume that FDs and nurses in palliative care teams constantly remain in a very early phase of 'norming', in which common values have to be formed, but where conflicts are not addressed. This challenge as well as the anticipated lack of a common future as a team might cause, especially in CBPC, the tendency for care givers to ‘retreat into their comfortable discipline-specific ways of operating’ (p. 26) or to avoid conflicts [40].
Conclusion
The above mentioned conflicts resp. disturbances in interprofessional collaboration in CBPC do have considerable negative consequences for professionals and patients: First of all, they may impede inter-professional approaches to shared decision making [41], which is known as an important pillar of the quality of care [31]. Further, it has already been demonstrated that the quality of IPC has an impact on workplace conflicts and job satisfaction of care providers [42].
Based on our findings it can be concluded, that the improvement of collaboration between health care providers in CBPC can be strongly supported - first of all - improving working conditions of the professionals. As a recent study on CBPC in Switzerland shows, FDs are only marginally supported by ambulant care structures (especially in rural areas), and also the availability of guidelines or standards in CBPC is small [26]. Beyond that, the possibilities to acquire interprofessional competences in palliative care are limited, and CBPC is poorly financed. FDs and nurses in Switzerland both act as single players due to the basic shortcomings of work organization.
Further, the organization of CBPC should enable the possibility of constructing long-lasting working relationships, as they have been found to increase the effectiveness of inter-professional teams [22]; if possible, FDs and nurses should be given the opportunity to work in the same team repeatedly. The creation of regular team meetings is necessary for inter-professional groups and should therefore be financially supported in CBPC. It allows to generate common norms and understanding and to diminish professional hierarchies, which have been shown to foster IPC. As evaluations of the Golden Standard Framework in the UK demonstrate, regular meetings enhance interprofessional communication [43]. As it is suggested for the treatment of patients with chronic conditions [44], the status of trained nurses as "care managers" could be strengthened, who are assigned to work in group physicians practice and follow FDs recommendations. 'Care managers' as part of FDs staff and/or palliative care networks could enhance direct collaboration between professionals, and improve the quality of care. In addition, to enhance communication styles, communication mechanisms can be improved in CBPC by using "unified and standardized documentation" which strengthens IPC (p. 140) [45].
Moreover, we recommend a stronger focus on inter-professional education and training prog45rams for CBPC providers, as it enables to understand and value the perspectives and attitudes of other carers [46]. Although the timing of inter-professional education has been found to be critical [47], it has been shown to reduce negative stereotypes concerning the other professional group [48]. Further, emphasis should be put on the training of open and sensitive interprofessional communication [22], including the communication of roles and responsibilities. Generally, the explicit content of interprofessionalism must be addressed in undergraduate studies and vocational training [27]; health care providers have to be informed about facilitators of IPC, and how possible conflicts can be managed. Measures can also be taken at the level of team processes: Enhancing care givers’ ability for meta-communication is highly recommended as part of the education.
As our results show, different levels of competence regarding PC in combination with professional hierarchies may lead to conflicts between FDs and nurses. There are several reasons why physicians tend not to attend further education programs in palliative care in Switzerland; once more they seem strongly related to working conditions resp. time constraints [26]. Nurses describe themselves as professionally socialized for caring, but even they do not necessarily attend training and further education programs in PC. However, a common understanding of palliative care is basic for successful IPC in CBPC. For this reason it should be fostered throughout the medical and nursing curriculum.
References
- Borgsteede S, Deliens L, van der Wal G, FranckeA, Stalman W, et al. (2007) Interdisciplinarycooperation of GPs in palliative care at home: A nationwide survey in the Netherlands. Scand J Prim Health Care 25: 226-231.
- Gilbert M, Staley C, Lydall-Smith S, Castle DJ (2008) Use of Collaboration to Improve Outcomes in Chronic Disease. Disease Management and Health Outcomes 16: 381-390.
- Alsop A (2010) Collaborative working in end-of-life care: developing a guide for health and social care professionals.Int J PalliatNurs 16: 120-125.
- Martin J, Ummenhofer W, Manser T, Spirig R (2010) Interprofessional collaboration among nurses and physicians: making a difference in patient outcome. Swiss Med Wkly149:(w13062).
- Zangaro GA, Soeken KL (2007) A meta-analysis of studies of nurses' job satisfaction.Res Nurs Health 30: 445-458.
- Tang CJ, Chan SW, Zhou WT, Liaw SY (2013) Collaboration between hospital physicians and nurses: An integrated literature review. International Nursing Review 60: 291-302.
- D'Amour D, Ferrada-Videla M, San Martin Rodriguez L, Beaulieu MD (2005) The conceptual basis for interprofessional collaboration: core concepts and theoretical frameworks.J Interprof Care 19 Suppl 1: 116-131.
- Boon H, Mior S, Barnsley J, Ashbury F, Haig R (2009) The difference between integration and collaboration in patient care: Results from key informant interviews working in multiprofessionalhealth care teams. J Manipulative PhysiolTher 32: 715-722.
- Marcus L, Dorn B, McNulty E (2011) Renegotiating health care: Resolving conflict to build collaboration. San Francisco: Jossey-Bass.
- Gaboury I, Bujold M, Boon H, Moher D (2009) Interprofessional collaboration within Canadian integrative healthcare clinics: Key components. SocSci Med 69: 707–715.
- Petri L (2010) Concept analysis of interdisciplinary collaboration.Nurs Forum 45: 73-82.
- Schalk R, Curseu P (2010) Cooperation in organizations. Journal of Managerial Psychology 25: 453-459.
- Garman A, Leach D, Spector N (2006) Worldviews in collision: Conflict and collaboration across professional lines. Journal of Organizational Behavior 27: 829-849.
- Brown J, Lewis L, Ellis K, Stewart M, Freeman TR, et al. (2011) Conflict on interprofessional primary health care teams--can it be resolved?J Interprof Care 25: 4-10.
- Suter E, Arndt J, Arthur N, Parboosingh J, Taylor E, et al. (2009) Role understanding and effective communication as core competencies for collaborative practice.J Interprof Care 23: 41-51.
- Pape R (2006) Das Beziehungsdreieck Patient-Pflegender-ArztimKrankenhaus. Einequalitative StudiezurInteraktion. Humboldt Universität Berlin.
- Lützenkirchen A (2005) InterdisziplinäreKooperation undVernetzungimGesundheitsweseneineaktuelleBestandesaufnahme. Gruppendynamik und Organisationsberatung 36: 311-324.
- Macdonald MB, Bally JM, Ferguson LM, Lee Murray B, Fowler-Kerry SE, et al. (2010) Knowledge of the professional role of others: A key interprofessional competency.Nurse EducPract 10: 238-242.
- Oishi A, Murtagh F (2014) The challenges of uncertainty and interprofessional collaboration in palliative care for non-cancer patients in the community: A systematic review of views from patient, carers and health-care professionals. Palliat Med 28: 1081-1098.
- Burtscher MJ, Manser T, Kolbe M, Grote G, Grande B, et al. (2011) Adaptation in anaesthesia team coordination in response to a simulated critical event and its relationship to clinical performance.Br J Anaesth 106: 801-806.
- Jensen HI, Ammentorp J, Erlandsen M, Ording H (2011) Withholding or withdrawing therapy in intensive care units: an analysis of collaboration among healthcare professionals. IntensiveCare Medicine 37: 1696-1705.
- Xyrichis A, Lowton K (2008) What fosters or prevents interprofessionalteamworking in primary and community care? A literature review.Int J Nurs Stud 45: 140-153.
- Binder J, von Wartburg L (2009) NationaleStrategie Palliative Care 2010-2012. BundesamtfürGesundheitund SchweizerischeKonferenz der kantonalenGesundheitsdirektorinnen und –direktoren. Bern.
- European Association of Palliative Care (2014) Promoting palliative care in the community: producing a toolkit to improve and develop primary palliative care in different countries internationally.Report of the Taskforce in Primary Palliative Care.
- Von Wartburg L, Näf F (2012) NationaleStrategie Palliative Care 2013-2015. BundesamtfürGesundheit (BAG) und SchweizerischeKonferenz der kantonalenGesundheitsdirektorinnen und – direktoren (GDK). Bern.
- Alvarado V, Liebig B (2015) Conditions and Challenges of Palliative Home Care: The Case of Family Physicians in Switzerland. Primary Health Care 5: 180.
- Otte I, Jung C (2014) Akteure und Strukturen in der schweizerischenpalliativmedizinischenVersorgung. In: Decker M, Bellucci S, Brochler S, Nentwich M, Rey L, Sotoudeh M (eds). Technologiefolgenabschatzungimpolitischen System. ZwischenKonfliktbewältigung undTechnologiegestaltung, Berlin: edition sigma, pp: 253-268.
- Loos P, Schäffer B (2012) Das Gruppendiskussionsverfahren. TheoretischeGrundlagen und empirischeAnwendung. VerlagfürSozialwissenschaften: Wiesbaden.
- Mayring PH (2014) Qualitative content analysis: theoretical foundation, basic procedures and software solution. Klagenfurt.
- Denzin NK (1989) The Research act: A theoretical introduction to sociological methods, New York.
- Zwarenstein M, Goldman J, Reeves S (2009) Interprofessional collaboration: Effects of practice-based interventions on professional practice and healthcare outcomes. Cochrane Database Syst Rev 3: CD000072.
- Solga M (2011) Konflikte in Organisationen. In:Nerdinger FW, Blickle G, Schaper N (eds.)Arbeits- und Organisationspsychologie, Berlin Heidelberg: Springer, pp: 122-134.
- Bateson G (1956) The message 'this is play'. In: SchaffnerB (eds.)Group Processes: Transactions of the Second Conference, New York: Josiah Macy, pp: 145–242.
- Dresske S (2001) Cooperation and negotiations in the home-healthcare sector. ZeitschriftfürGesundheitswissenschaften 9: 68-84.
- Jünger S, Pestinger M, Elsner F, Krumm N, Radbruch L (2007) Criteria for successful multiprofessional cooperation in palliative care teams.Palliat Med 21: 347-354.
- Lewicki RJ (2006) Trust, trust development, and trust repair. In: Deutsch M, Coleman P, Marcus E (eds.) The Handbook of Conflict Resolution: Theory and Practice, San Francisco: Wiley.
- Axelsson SB, Axelsson R (2009) From territoriality to altruism in interprofessional collaboration and leadership.J Interprof Care 23: 320-330.
- Harris M, Chan B, Daniel C, Wan Q, Zwar N, et al. (2010) Development and early experience from an intervention to facilitate teamwork between general practices and allied health providers: the Team-link study. BMC Health Services Research 10: 104.
- Krauss RM, Morsella E (2006) Communication and conflict. In: Deutsch M, Coleman P (eds.) The handbook of constructive conflict resolution: Theory and practice. San Francisco: Jossey- Bass.
- Drinka T, Clark P (2000) Health Care Teamwork: Interdisciplinary Practice and Teaching. Westport: Greenwood Publishing Group.
- Légaré F, Stacey D, Brière N, Fraser K, Desroches S, et al. (2013) Healthcare providers’ intentions to engage in an interprofessional approach to shared decision-making in home care programs : A mixed methods study. J Interprof Care 27: 214-222.
- Nakakis K, Ouzouni C (2008) Factors influencing stress and job satisfaction of nurses working in psychiatric units: A research review. Health Science Journal 2: 183-195.
- Walshe C, Caress A, Chew-Graham C, Todd C (2008) Implementation and impact of the Gold Standards Framework in community palliative care: A qualitative study of three primary care trusts.Palliat Med 22: 736-743.
- Ciccone MM, Aquilino A, Cortese F, Scicchitano P, Sassara M, et al. (2010) Feasibility and effectiveness of a disease and care management model in the primary health care system for patients with heart failure and diabetes (Project Leonardo).Vasc Health Risk Manag 6: 297-305.
- San Martín-Rodríguez L, Beaulieu MD, D'Amour D, Ferrada-Videla M (2005) The determinants of successful collaboration: A review of theoretical and empirical studies.J Interprof Care 19 Suppl 1: 132-147.
- Khalili H, Hall J, DeLuca S (2014) Historical analysis of professionalism in western societies: implications for interprofessional education and collaborative practice. JInterprof Care 28: 92-97.
- Mandy A, Milton C, Mandy P (2004) Professional stereotyping and interprofessional education. Learning in Health and Social Care 3: 154-170.
- Ateah CA, Snow W, Wener P, MacDonald L, Metge C, et al. (2011) Stereotyping as a barrier to collaboration: Does interprofessional education make a difference?Nurse Educ Today 31: 208-213.
Relevant Topics
- Chronic Disease Management
- Community Based Nursing
- Community Health Assessment
- Community Health Nursing Care
- Community Nursing
- Community Nursing Care
- Community Nursing Diagnosis
- Community Nursing Intervention
- Core Functions Of Public Health Nursing
- Epidemiology
- Epidemiology in community nursing
- Health education
- Health Equity
- Health Promotion
- History Of Public Health Nursing
- Nursing Public Health
- Public Health Nursing
- Risk Factors And Burnout And Public Health Nursing
- Risk Factors and Burnout and Public Health Nursing
Recommended Journals
- Epidemiology journal
- Global Journal of Nursing & Forensic Studies
- Global Nursing & Forensic Studies Journal
- global journal of nursing & forensic studies
- journal of community medicine& health education
- journal of community medicine& health education
- Palliative Care & Medicine journal
- journal of pregnancy and child health
Article Tools
Article Usage
- Total views: 13855
- [From(publication date):
May-2016 - Apr 04, 2025] - Breakdown by view type
- HTML page views : 12731
- PDF downloads : 1124