Internuclear Ophthalmoplegia as a Sole Presentation of Acute Ischemic Stroke Involving the Midbrain with an NIH Stroke Scale of One
Received: 15-Nov-2017 / Accepted Date: 20-Nov-2017 / Published Date: 27-Nov-2017
Abstract
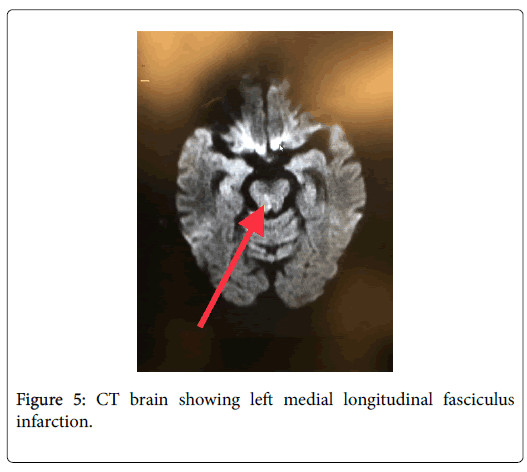
The National Institute of Health Sciences Scale (NIHSS) is a popular screening tool in the Emergency Department to rule out strokes. However, a small number of cases can be missed. But it is useful to remember that any sudden onset cranial nerve involvement could be a symptom of stroke and hence must be investigated thoroughly as time is brain. Internuclear ophthalmoparesis (INO) or internuclear ophthalmoplegia is very typical of a brainstem lesion. Our patient had complaints of sudden onset diplopia secondary to internuclear ophthalmoplegia with no other signs or symptoms. Though her NIHSS was only 1, given her longstanding history of hypertension, an immediate CT Brain was ordered which showed a fresh infarct of the left Medial Longitudinal fasciculus.
Keywords: Stroke; Internuclear ophthalmoplegia; Diplopia; Medial longitudinal fasciculus; Emergency medicine
Introduction
Internuclear ophthalmoparesis (INO) or internuclear ophthalmoplegia, is a distinct gaze abnormality characterized by impaired horizontal eye movements with weak adduction of the affected eye, and abduction nystagmus of the contralateral eye. Its presence is very typical of a brainstem lesion, specifically due to involvement of the medial longitudinal fasciculus (MLF) in the dorsomedial brainstem tegmentum of either the pons or the midbrain. Isolated unilateral internuclear ophthalmoplegia is a relatively rare occurrence and can be seen in a minor acute ischemic stroke involving the Medial longitudinal fasciculus. It is important to differentiate uniocular and binocular diplopia as the former could be a result of a refractive error however, the later could imply the involvement of a cranial nerve or a higher Central Nervous System lesion. National Institute of Health Stroke Scale (NIHSS) is the most popular Emergency Department tool to evaluate stroke. However, as per an American Heart Association (AHA) study it had detected 88% of the ischemic strokes [1]. Implying a certain percentage may lie outside its realm. However, in case of acute onset neurological involvement of cranial nerves must always raise a suspicion for a stroke and must be investigated thoroughly and even a low NIHSS must not deter the physician from following the stroke protocol.
Case Report
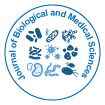
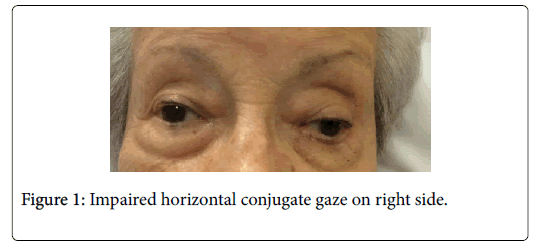
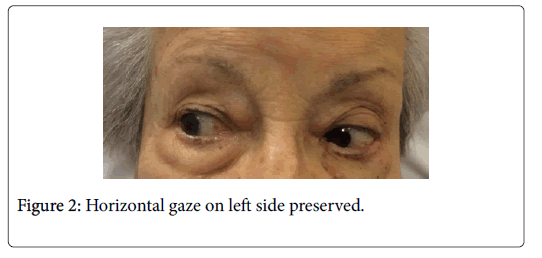
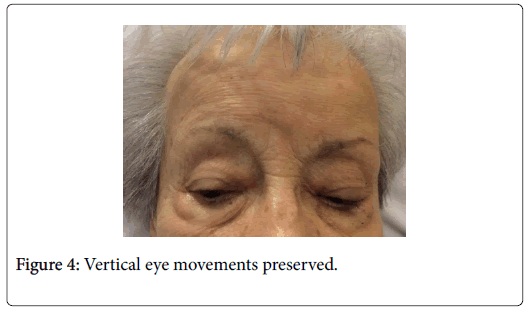
A 93 year old woman presented to the Emergency Department with past medical history of Hypertension, and chief complaints of sudden onset diplopia. The patient reported difficulty seeing upon waking up which led to unsteadiness and hence decided to seek medical attention. She denied any history of falls, weakness or numbness, any trouble swallowing or hearing. She reported a recent knee replacement surgery of the right knee. The patient was on no other blood thinners or anticoagulants other than a daily aspirin dose of 80 mg. On physical exam, she was afebrile, with respiratory rate of 16 breaths/min, blood pressure of 166/45 mm hg, Heart rate of 80 bpm, and oxygen saturation of 98% on room air. An ocular exam showed disconjugate gaze at rest with right eye laterally deviated. Horizontal eye movements were impaired with weakness of right medial rectus muscle, preserved convergence test, and bilateral reactive pupils. The patient had an upgoing plantar on the right side. The remaining extraocular muscles (superior rectus, inferior rectus, lateral rectus, superior oblique, and inferior oblique) (Figures 1-4) and other cranial nerves were normal. There was no nystagmus, ptosis, flushing of the skin or peripheral visual field loss. Sensation, proprioception, joint and vibratory sense were normal.
Investigations
Finger stick glucose in the E.D documented a high blood sugar of 224 mg/dl, and subsequent blood glucose showed a spontaneously resolving trend with the last recorded blood glucose as 174 mg/dl.
Sr Sodium 135 mmol/l, Sr Potassium 3.2 mmol/l, Sr Chloride 96 mmol/l, Sr Phosphorus 2.1 mg/dl, Sr Albumin 3.3 g/dl. Urine was positive for glucose.
CT Brain, MRI brain with and without contrast, MRA of head and Neck was performed. Though the radiology report stated that there was an 11 × 11 mm focus of acute infarction within the left cerebellar tonsil, the neurologists stated that the affected area was in fact the left Medial Longitudinal fasciculus. Upon review of the anatomy of the midbrain MRI (Figure 5), it was decided the affected area was indeed the left Midbrain. (Comparison CT head from 05/26/2017).
Discussion
Diplopia is a common subjective complaint amongst patients. Identifying the etiology of diplopia can be a challenge because of the long list of differential diagnoses. Thus, a thorough history and physical examination is essential to diagnose and manage diplopia. Our patient had binocular diplopia, defined as “diplopia (that) resolves when the affected eye is occluded”, which indicates misalignment of the visual axes as being the cause of the diplopia. In contrast, monocular diplopia, defined as “diplopia (that) persists when the affected eye is occluded” is usually caused by ophthalmological pathology, such as refractive error [2]. The binocular diplopia in our patient limited the differential diagnosis to impaired neural control or function of the extraocular muscles. Thus it is extremely important to do a careful eye exam. The most likely differentials for her included sudden onset partial oculomotor neuropathy secondary to uncontrolled diabetes mellitus and a brainstem stroke. However, in view of her NIHSS being just 1, there was a good chance of missing the stroke based on preliminary screening. It is also useful to remember that cranial nerve involvements can help localize the site of lesion and detect incipient strokes.
Conclusion
In the emergency department, any acute onset cranial nerve involvement, especially in the setting of risk factors such as hypertension, must prompt investigations to rule out potential stroke even if the NIHSS is not strongly suggestive of one.
References
- Muir KW, Weir CJ, Murray GD, Povey C, Lees KR. (1996) Comparison of Neurological Scales and Scoring Systems for Acute Stroke Prognosis. Stroke 27: 1817-1820.
- Frohman EM1, Zhang H, Kramer PD, Fleckenstein J, Hawker K, et al. (2001) MRI characteristics of the MLF in MS patients with chronic internuclear ophthalmoparesis. Neurology 57: 762-768.
Citation: Shetty NU, Shpilko M (2017) Internuclear Ophthalmoplegia as a Sole Presentation of Acute Ischemic Stroke Involving the Midbrain with an NIH Stroke Scale of One. J Biol Med Sci 1: 104.
Copyright: © 2017 Shetty NU. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Usage
- Total views: 4268
- [From(publication date): 0-2017 - Nov 24, 2024]
- Breakdown by view type
- HTML page views: 3561
- PDF downloads: 707