Commentary Open Access
Integral of Pain Relief as an Innovative Method of Pain Measurement
Igor Wilderman* and Rachel Berkovich
Wilderman Medical Clinic, Thornhill, Ontario, Canada
- *Corresponding Author:
- Wilderman I
Wilderman Medical Clinic
8054 Yonge Street. Thornhill
Ontario, Canada, L4J1W3
Tel: 905-886-1212
Fax: 905-886-0248
Email: iw@drwilderman.com
Received date: November 24, 2016; Accepted date: December 09, 2016; Published date: December 13, 2016
Citation: Wilderman I, Berkovich R (2017) Integral of Pain Relief as an Innovative Method of Pain Measurement. J Pain Relief 6:277. doi: 10.4172/2167-0846.1000277
Copyright: © 2016 Wilderman I, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Pain & Relief
Abstract
Objective: To describe and bring awareness for the Integral of Pain Relief (IPR), a novel multidimensional measure which can be used by practitioners in daily practice.
Methods: The IPR incorporates both a patients’ percentage of pain relief since treatment, along with their duration of relief into a single, multidimensional value. This value can allow for practitioners to better understand optimal treatments for various patients, select between different treatment modalities, and visualize on a graph the efficacy of numerous treatment methods.
Conclusion: With the implementation of the IPR in daily practice, a multidimensional perspective on an individual’s overall pain relief can provide promising hope for upcoming practice and treatment. Future research can focus on discovering optimal IPR ranges for various treatment modalities, as well as for determining weighted values for both variables of the IPR.
Keywords
Chronic pain; Pain management; Novel method; Pain relief
Introduction
The Visual Analogue Scale (VAS) is the gold standard and most frequently used assessment to measure for pain relief and pain intensity [1]. The popularity of the VAS stems from its simplicity and convenience [1]; however, we pose a question here. How can researchers and medical practitioners alike rely on a one-dimensional scale that requires patients to recall their own pain at a remote time, in order to judge their pain at present, with allowing no consideration for the duration of how long the pain (or pain relief) had lasted? Past research has even deemed the VAS as a primary clinical outcome measure, undependable and sometimes producing unpredictable results [1]. It is peculiar that countless authors publish research articles on treating chronic pain but solely focus on the decrease in VAS score as their primary outcome measure while failing to involve the important value of the duration of relief. If there was a demonstrated VAS decrease but no reported timeline of how long this lasted, the results are deemed unreliable in our eyes, as pain relief without a timeframe does not prove the treatment efficacious. A new multidimensional, precise method to measure pain relief needs to be implemented in pain research. The sole purpose of this article is to bring about exposure to the Integral of Pain Relief (IPR), a method created at Wilderman Medical Clinic.
Many pain studies published rely on the VAS score as their outcome measure to prove how well their treatments and intervention methods have been working. An example of this is the research done by Geisler et al. [2]. The criterion in their research that predicted successful results was an 80% decrease in VAS scores to <3 for post-operative patients. A score of less than 3 would denote “mild pain”. Follow-up is done 6 hour and 24 hour post operation [2]. How can the results be validated when the duration of pain relief is not accounted for past 24 hours? A systematic literature review of pain intensity assessment methods in 239 studies found that VAS had a much lower compliance compared to the Numerical Rating Scale (NRS) and the Verbal Rating Scale (VRS) [3]. Compliance was mainly based on error rate percentages in scores. It was also found that VAS scores were more likely to include discrepancies in patients’ answers than NRS or VRS scales [3]. This leaves us quite skeptical about the reliability of the outcome. Foremost, patients must recall their VAS score from a prior time, which is most often the last time they were seen by their clinician, and they must then state their current score based on the previous. Instead, it is much simpler to have patients recall their average percentage of pain relief since treatment, as being relieved of pain tends to produce a lasting memory in the minds of chronic pain patients. Thus in our view, it is easier for patients to recall the percentage of pain relief, as opposed to a sole pain score at a follow- up appointment. From firsthand experience and chart reviews from our clinic, it has been found that there is a notable discrepancy between using the difference in VAS scores as the sole outcome measure to establish treatment efficacy, and using the percentage of pain relief. It has been revealed that when solely using VAS, patients tend to produce scores higher than their baseline, while saying that they have indeed experienced pain relief, introducing a contradiction in results. This could be attributed to a flaw in memory. It has been reported that there is a higher number of similar errors seen when using VAS in aging populations, and in the cognitively impaired [3]. Thus, VAS can be seen as an unreliable follow-up measure for a large population of chronic pain patients. It was noted in a 2011 review of all methods of pain measurement, that the VAS scale is difficult to understand for patients with cognitive impairment, and requires supervision to minimize errors [4]. Supervision could lead to probing, which can present a bias into results. The review also states that the recall period of VAS scores is most commonly limited to 24 hours after baseline [4]
Methods
It would be more logical and reliable to introduce the IPR, a measure created and implemented here at Wilderman Medical Clinic. The IPR involves recording an initial VAS score, which is taken at the initial visit, before any treatment. At the follow-up appointment, the patient is asked if he/she experienced pain relief. If they answered yes, they were asked about the percentage of pain relief experienced since the initial visit (e.g. 70% relief). This is one of the main differences between the IPR and the VAS. Patients are not required to recall their previous VAS score, they are simply asked to state how much relief they have experienced. A prospective study completed in 2014 showed that patient reports of the percentage of pain relief were statistically higher and more significant than reported VAS scores at the post-trial period [5]. Once patients give their percentage of pain relief, they are then asked to recall the duration of their relief; because knowing how long a treatment lasts is crucial in maintaining and implementing proper treatment. The IPR is then calculated in the following way:
Pain relief percentage (%) × duration relief in days=an IPR value.
Discussion
For each treatment modality used, (i.e. medication, injection, physiotherapy, etc.) a different range of IPR scores would be sufficienttherefore, the higher the IPR, the greater the pain relief, and the more effective the treatment. When the VAS score is used as the primary outcome measure, and it decreases from baseline to treatment, it is considered a successful result [6]. Thus, it can also be said that the greater the decrease in VAS, the more effective the treatment [6]. The IPR shares similarities with the Pain Relief Index (PRI), created by Wang et al. [7]. The index created by Wang et al. stems from the premise that cancer pain patients must first recall their pain intensity using a numeric scale. They are asked about their worst pain intensity (WPI) and their last recorded pain intensity (LPI). Once they have established their WPI, practitioners subtract the WPI value from their LPI to achieve a percent intensity difference (PID). The PRI is then calculated from these three values (WPI, LPI and PID %), to produce a score which provides a practitioner with an idea of a patient’s overall pain relief [7]. The PRI provides information on the magnitude of pain relief, ranged from-100% and 100%, with-100% being no relief and 100% denoting that complete pain relief has been achieved [7]. What is missing from the PRI is the important component of duration of relief. This is a major difference between the PRI and IPR. Another difference stems from the derivation of the PRI solely focusing on cancer patients, who receive treatment daily in a hospital setting. The IPR is applicable not just for daily treatment, but for all treatment modalities and a wide range of chronic pain sufferers.
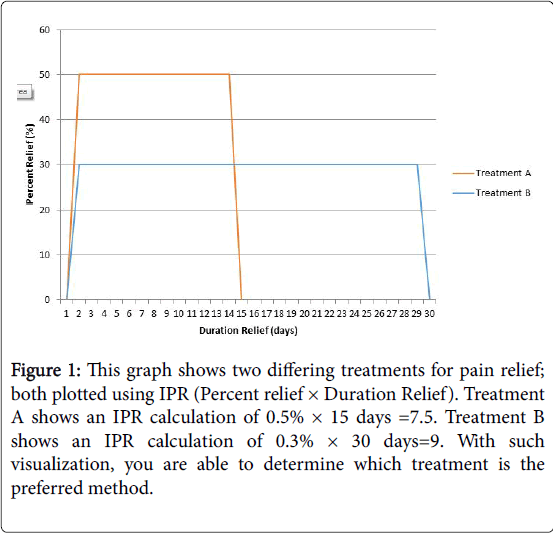
With the IPR in place, researchers and practitioners are able to visualize scores as they can be plotted on a curve. IPR can be plotted similarly to the area under the curve (AUC), which is a standard measure of medication pharmacokinetics. From AUC data, you are able to derive pain relief and duration of pain relief [8]. The area under the pain relief percentage vs. duration (IPR) curve can be used to produce the number of patients experiencing X% pain relief over a Y amount of time [8]. It also can allow for the visualization of the efficacy of various pain relief treatments (Figure 1). The multi-dimensional IPR measure would be able to render results found in publications solely relying on VAS as their primary outcome measure more reliable, as the IPR would have allowed the researchers to understand how long the pain relief lasted following treatment. Solely relying on the VAS score seems to be an outdated standard measure when trying to prove the efficacy of pain relief treatments.
Figure 1: This graph shows two differing treatments for pain relief; both plotted using IPR (Percent relief × Duration Relief). Treatment A shows an IPR calculation of 0.5% × 15 days =7.5. Treatment B shows an IPR calculation of 0.3% × 30 days=9. With such visualization, you are able to determine which treatment is the preferred method.
Conclusion
Currently, we are in the works of modifying the brief pain inventory, a questionnaire designed to measure a person’s pain severity. The goal is to replace the four VAS likert scales for the pain severity sub-domain from 0-10, with a single scale that uses the IPR. This will enable a pain practitioner to assess the necessity of certain treatments, or perhaps change the treatment modality during the visit. This is also providing more accurate predictions of when patients should be seen for followup. The goal of this research is to create the best approximation of a pain measurement index to be used in daily practice and medical research.
Future research on the IPR can attempt to investigate two things. The first investigative study can work towards discovering optimal IPR values for various intervention methods to determine the efficacy of a number of different treatment modalities (ex: physiotherapy, cortisone, lidocaine, etc.). Secondly, the IPR assumes both of its variables are of equal value, hence why you must simply multiply them to create a sole IPR value. This is a limitation of the measure. A prospective study can look towards assigning weighted values to both variables of the IPR (percentage of pain relief × duration of relief), as for some patients either variable would be of greater importance, depending on the severity and type of pain they suffer from.
Conflict of Interest
None.
Acknowledgement
Thank you to Jason Norman (General Manager at Wilderman Medical Clinic) and Omer Kleiner (Research Assistant at Wilderman Medical Clinic) for their internal review. We appreciate all your help.
References
- Reed M, Van Nostran W (2014) Assessing pain intensity with the visual analog scale: A plea for uniformity. J ClinPharmacol. 54:241-244.
- Geisler A, Dahl J, Karlsen A, Persson E, Mathiesen O (2016) Low degree of satisfactory individual pain relief in post-operative pain trials. ActaAnaesthesiol Scand. 61: 83-90.
- Hjermstad MJ, Fayers PM, Haugen DF, Caraceni A, Hanks GW, et al. (2011) Studies Comparing Numerical Rating Scales, Verbal Rating Scales, and Visual Analogue Scales for Assessment of Pain Intensity in Adults: A Systematic Literature Review. J Pain Symptom Manage. 41:1073-1093.
- Hawker GA, Mian S, Kendzerska T, French M (2011)Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res (Hoboken).63: S240-S252.
- Mironer YE, Satterthwaite J, Hutcheson KJ (2014) Comparison of the visual analog scale (vas) and the scaling pain relief (spr) measurements in the assessment of the results of spinal cord stimulation trial and therapy: A prospective study. Pain Studies and Treatment.2:1-5.
- Dong J, Li W, Wang Y (2016) The effect of pregabalin on acute postoperative pain in patients undergoing total knee arthroplasty: A meta-analysis. Int J Surg.34:148-160.
- Wang WY, Chu CM, Sung CS, Ho ST, Wu YS, et al. (2016) Using a New Measurement to Evaluate Pain Relief Among Cancer In- patients with Clinically Significant Pain Based on a Nursing Information System: A Three-Year Hospital-Based Study. Pain Med. 17: 2067-2075.
- Lee CJ, Lee LH, Wu CL, Lee BR, Chen ML (2006) Clinical Trials of Drugs and Biopharmaceuticals. CRC Presspp: 1-520.
Relevant Topics
- Acupuncture
- Acute Pain
- Analgesics
- Anesthesia
- Arthroscopy
- Chronic Back Pain
- Chronic Pain
- Hypnosis
- Low Back Pain
- Meditation
- Musculoskeletal pain
- Natural Pain Relievers
- Nociceptive Pain
- Opioid
- Orthopedics
- Pain and Mental Health
- Pain killer drugs
- Pain Mechanisms and Pathophysiology
- Pain Medication
- Pain Medicine
- Pain Relief and Traditional Medicine
- Pain Sensation
- Pain Tolerance
- Post-Operative Pain
- Reaction to Pain
Recommended Journals
Article Tools
Article Usage
- Total views: 3561
- [From(publication date):
January-2017 - Jul 18, 2025] - Breakdown by view type
- HTML page views : 2735
- PDF downloads : 826